2 Preoperative Assessment and Perioperative Management Abstract This chapter will provide an overview of preoperative assessment as it relates to plastic surgery. It will include medication management and will review perioperative antibiotic management. The reader will be able to prepare management plans for different scenarios. Keywords: preoperative assessment, perioperative management, DVT, antibiotic prophylaxis, SCIP Six Key Points • The Surgical Care Improvement Project (SCIP) defines postoperative events and makes recommendations on perioperative management. • Superficial plastic surgery cases are low risk. • Patients with cardiac stents should remain on anticoagulation. • Smoking increases complications fivefold. • Patients should stop smoking 8 weeks prior to elective surgery. • Assess the risk of obstructive sleep apnea. While the preoperative workup can be tailored to a specific problem, there are general principles of perioperative management that are useful for any case. The Surgical Care Improvement Project (SCIP) was created in 2003 as an initiative of the Centers for Disease Control and Prevention (CDC) and Centers for Medicare & Medicaid Services (CMS), and has a defined goal to reduce surgical morbidity and vmortality. It has defined postoperative events and makes recommendations on perioperative management. 1. What is considered low-risk surgery? Superficial plastic surgery cases and general breast surgery are considered low-risk surgeries. Low-risk surgery can become moderate risk surgery if general anesthesia is required. 2. What are the revised cardiac risk indicators? Invasive surgery, ischemic heart disease, heart failure, cerebrovascular accident (CVA), creatinine greater than 2.0, and diabetes mellitus requiring insulin. 3. Your patient was found to have a cardiac condition and had stents placed. Under what conditions do you proceed with surgical intervention? If a patient has had a previous balloon angioplasty over 14 days ago, one can proceed with surgery if the patient continues aspirin. If the patient has a bare-metal stent, and it has been more than 6 weeks (ideally 3 months), the patient can be taken to surgery with aspirin. If the patient has had a drug-eluting stent, nonurgent surgery should be postponed until after a year, and then surgery can proceed if the patient continues aspirin. 1. Your patient wants to know which medications he can take before surgery (Table 2.1). What do you tell him? Some medications can be taken up to and including the day of surgery, some should be taken until surgery but not taken on the day of surgery, and some should be stopped prior to surgery. These are summarized in Table 2.1. 1. Your patient is a smoker. What sorts of perioperative pulmonary risks are associated with smoking? All complications (major and minor) related to smoking are increased almost fivefold when compared with never smokers. Past smokers are also at increased risk.1 2. How long should a patient have quit smoking prior to surgery? Ideally, a patient should have quit smoking for at least 8 weeks prior to elective surgery.2 3. How do you verify the patient has quit smoking prior to surgery? One always has discussion with patients regarding smoking prior to surgery. Identification and verification of smoking cessation is a two-pronged approach: direct discussion with the patient and a serum cotinine test. RATIONALE: A serum cotinine test can be ordered either qualitatively or quantitatively. The quantitative test will help distinguish between an active tobacco user and one who has recently quit; it takes approximately 2 weeks for serum cotinine to return to normal.
Overview
Questions
Case 1
Preoperative Assessment
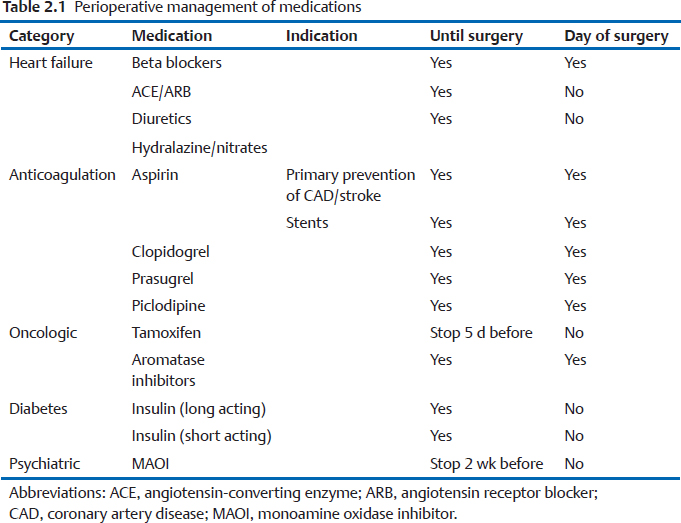
Medication Management
Pulmonary
Plastic Surgery Key
Fastest Plastic Surgery & Dermatology Insight Engine