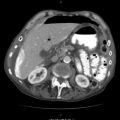
Fig. 17.1
Probe positions for FAST
Fig. 17.2
(a) Schematic drawings of scans. RV right ventricle, RA right atrium, LV left ventricle, LA left ventricle. (b) Four normal scans. (c) Four abnormal scans
All rotations of the probe in FAST should be anticlockwise from this starting position, such that the patient’s right side comes to lie to the right of the screen. This again maintains a standard accepted orientation.
Fluid is black and will collect in one of the areas as depicted in Fig. 17.2a–c.
You should be aware of the significant pitfalls in performing a FAST scan. Most important of these is the fact that you need blood to bleed. A negative scan does not exclude injury. Remember in all situations to trust your clinical judgement. Repeat regularly as this improves accuracy and detects evolving bleeding.
YOU NEED BLOOD TO BLEED.
The presence of significant surgical emphysema can make an image impossible to obtain (air is the enemy of ultrasound!). As you learn this technique, be wary of false positives, particularly interpreting the gall bladder and inferior vena cava (IVC) on the right as free fluid in the abdomen.
The only way to avoid this is to look for fluid in predefined spaces –If you are not getting a view of both the liver and kidney (as in figure 2) then you can easily mistake the IVC or gallbladder for free fluid. If you are not seeing both the kidney and liver do not call it.
17.1.4 Pearls
- 1.
Always start with notch (US probe indicator) at the top to orientate your image.
- 2.
Make all rotations anticlockwise.
- 3.
Look at the pericardium first to define fluid as black.
- 4.
Repeat! Repeat! Repeat!
- 5.
Do not forget – you need blood to bleed.
- 6.
In patients who are about to have or have a cardiac arrest, do not use US and delay your decision to perform a resuscitative thoracotomy – in this situation, it adds little to what should be a highly standardised protocol-driven scenario!
17.2 Pneumothorax
Detection of pneumothorax is an exciting use of point-of-care ultrasound and is much more sensitive than chest X-ray, which at best picks up 60 % of pneumothoraces. Even US-naive practitioners can be taught this technique in a short period of training.
It has the value of being fast, portable and repeatable, and in the often-noisy world of trauma, particularly prehospital, this ‘visual stethoscope’ has obvious advantages over an auditory stethoscope.
Air is considered the enemy of ultrasound, so in this scanning modality, it is not the detection of air rather the detection of the lack of normal signs/artefacts that is utilised. When visualising the interface between the two layers of pleura, certain signs are considered normal:
- 1.
Sliding – you will see this as a sliding motion between the two layers of the pleura; if air interposes between the layers, then this will be lost.
- 2.
Comet-tail artefacts – these are reverberation or ring-down artefacts caused by fluid in the interstitium of the lung; if the lung cannot be visualised because air has interposed, this artefact will be lost.
- 3.
You can use M-mode to look for motion of the lung – where there is motion of the lung, there is the appearance of a seashore sign (Fig. 17.3a, b).
Fig. 17.3
Photo of seashore sign (a) M-mode – note the lower part of image has texture like a beach with sea in the distance – this disappears with a pneumothorax when it all looks the same (b)
In the context of penetrating trauma, US is valuable for both detecting and ruling out a pneumothorax. In the prehospital arena and in resuscitation, this will decrease the need to undertake blind prophylactic thoracostomies/needle thoracocenteses.
17.2.1 Pitfalls
- 1.
Lack of sliding does not always equal a pneumothorax! In effect, lack of sliding is the visual equivalent of no breath sounds (e.g. in a right main bronchus intubation, only the right lung moves); so before you diagnose a pneumothorax in the intubated patient, check the tube distance at the teeth and consider pulling the tube back a bit. You may of course also find this useful as an adjunct in noisy environments for checking the tube position. Looking for a lung point, the point where sliding begins, is almost 100 % sensitive but can be time consuming.
- 2.
Bullae can be confused for pneumothorax, so proceed with caution in patients with chronic lung disease.
- 3.
Surgical emphysema can cause great difficulty in visualising anything.
- 4.
A one-off anterior probe position in the same site as you would listen for a pneumothorax will merely alert you to the presence of a pneumothorax. You can quantify the size by multiple site sampling or a chest X-ray – in this context, however, an ill patient with signs of a pneumothorax gets a drain and a well patient further imaging.
A PNEUMOTHORAX IS RECOGNISED BY THE ABSENCE OF NORMAL SONOGRAPHIC SIGNS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree