Photoprotection
Vermén M. Verallo-Rowell
The deleterious effects of ultraviolet and visible light on human skin include sunburn, suntan, phototoxic and photoallergic reactions, aggravation of hyperpigmentary disorders, photoaging, immunosuppression, solar keratoses, and the induction of skin cancers. For more than 70 years, commercial sunscreens have been used to mollify these detrimental cutaneous effects of light. The first, containing benzyl salicylate and benzyl cinnamate, was developed and marketed in the United States in 1928.1
Since the development of the early formulations to prevent sunburn, sunscreens have evolved as the gold standard for skin protection from ultraviolet light. In general, sunscreens are used to prevent sunburn, limit photodamage, and decrease the risk of skin cancers, including basal cell carcinomas, squamous cell carcinomas, and malignant melanoma. The International Agency for Research on Cancer reported that although the data on sunscreen prevention of actinic keratoses and squamous cell carcinomas is adequate, that on basal cell carcinomas and melanomas is inadequate.2 Despite this finding, most clinicians and researchers agree that an overall sun protection program should include limited sun exposure, protective clothing, sun visors, hats, and daily use of sunscreen.
Indications for Sunscreen Use in Darker Racial Ethnic Groups
Individuals encompassing Fitzpatrick’s skin types III/IV through VI generally have olive, brown, or black skin (see Chapter 2). Such individuals have a substantially lower incidence of skin cancers and photoaging. Photoimmunosuppression has been reported to be milder, and photosensitivity is less common.3 Why, then, do people with darker skin need sunscreens?
Disorders of hyperpigmentation have emerged as a key indication for sunscreen use in darker skin types. These include melasma, postinflammatory hyperpigmentation (PIH), ephelides, lentigines, Hori’s nevus, postlaser, and phototherapy hyperpigmentation. Albeit less life threatening than cancers and melanomas, these skin problems seriously affect quality of life (see Chapter 6). Skin cancers are another indication. Although still relatively rare among those with darker skin, the incidence is growing. The Cancer Registry in Singapore in 1988 noted increasing incidence of skin cancers, excluding melanoma.4 By 2002, skin cancer, including melanoma, reached the top-ten cancers list.5 This higher ranking for skin cancer may be attributed to more affluence, a favoring of increased outdoor leisure activities, longer life spans, and exposure to more solar ultraviolet rays brought on by the factors that promote stratospheric ozone depletion.6
Sociological/cultural issues further influence the use of sunscreens in darker skin. A unique irony regarding skin color is that those with lighter skin cherish being darker (i.e., acquiring a tan), whereas many of those with olive or darker skin prefer to have lighter-colored skin. Toward this goal, sun avoidance is a popular practice. Unless demanded by work or for play, when outdoors, those with darker skin who prefer light skin color look for deep shades, use parasols, wear wide-brimmed hats, and cover up with clothing.7 They also frequently use skin lighteners.8 Both practices are common among those who are generally of mixed heritage: African Americans;9 Africans;10 Asians;11 Hispanics;12 Middle Easterners;13 and Caribbean Islanders.14 This is true even among some of the more ethnically homogenous Asians from Japan,15 China,16 or Korea, who, despite being fairer than other Asians, consider themselves “brown.”17
Use of sunscreens is not a common practice because darker skin phototypes III/IV to VI do not burn readily and have a baseline color that darkens easily and is perceived to be protective.
Because sun-induced/aggravated hyperpigmentations are common in those with darker skin, their customary sun behavioral practices are obviously not enough to avoid these conditions. What follows is a review of the light wavelengths that sunscreens protect against to understand which to use for the specific indications needed by those with darker skin.
Electromagnetic Radiation Wavelength Effects and Protection
Sunlight is divided into three components, including ultraviolet (UV) light, visible light (VL), and infrared light (IRL), with UV representing the most important component (Fig. 12-1). UV is divided into three groups based on the wavelength of light: (i) UVC (100–280 nm), which minimally affects the earth’s surface because it is blocked by the ozone layer, (ii) UVB (290–320 nm), which causes erythema, sunburn, DNA damage, solar elastosis, hyperpigmentation, and skin cancer, and (iii) UVA (320–400 nm), which requires a higher dose to induce erythema but easily elicits two pigment-darkening responses, both produced by the photo-oxidation of melanin.18 Immediate pigment darkening (IPD) starts in seconds after UVA exposure and disappears within 2 hours. At higher doses of 8 to 25 J/cm2 from 2 to 24 hours after exposure, IPD is followed by more pigmentation, the PPD or persistent pigment darkening. In those with lighter skin, this lasts about 24 hours.19 In those with darker skin, it lasts much longer, often continuing into the delayed tanning effect of both UVB and UVA.20 UVB does not produce IPD nor PPD, but produces, with UVA, a delayed tanning response that peaks at 72 hours. This is brought on by an increase in the number of active melanocytes and tyrosinase, which together produce new melanosomes, melanin, and transfer to keratinocytes.21
IPD and PPD are not photoprotective,21 an important point to remind those with darker skin who may think that their immediate darkening protects them from the sun. The UVB-induced delayed tanning after erythema has a sun protection factor (SPF) of 3, which is a few points higher in darker skin.21
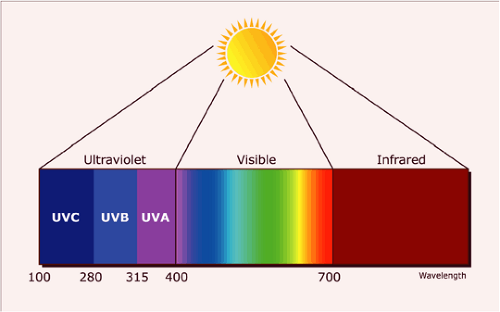 Figure 12-1 Schema of the electromagnetic spectrum of light and the wavelengths of its three components discussed in the text in regard to their specific effects on darker skin. |
Erythema reactions
Both UVB and UVA produce acute erythema, but UVA is much less efficient than UVB. Approximately 1,000 times more UVA than UVB is needed to elicit the same erythema response.22
Solar UVB-induced acute erythema starts after about 4 hours of exposure, peaks at 8 to 24 hours, and fades after a day or so. However, among the very fair or very old, this may last for weeks.23 The acute erythema induced by UVA for both light and darker skin color is milder than the UVB erythema and biphasic. The first phase appears immediately after exposure and fades in several hours. The second phase starts at about 6 hours and peaks at 24 hours.24
After a single erythema response, both UVB and UVA increase epidermal and dermal mitotic activity. That of UVB persists for days to weeks, with much more thickening of the epidermis and dermis.24 Only after repeated exposures does UVA produce thickening of the epidermis, but this is much less than that from UVB.24
Chronic erythema produces P53 gene mutation, which is found in 90% of squamous cell carcinomas, 60% of actinic keratosis, and 50% of basal cell carcinomas.25 Even nonerythemal sun exposure induces reactive oxygen species-mediated DNA change and pyrimidine dimer formation leading to skin cancer in animal models.26
Repeated UVA radiation has in recent years been shown to produce even more immunosuppression than UVB.27 Animal models develop skin alterations of the Langerhans cells—their number, functions and morphology—resulting in photoimmunosupression. This is mediated
in part through the generation of cis-urocanic acid, tumor necrosis factor, and interleukin-10.28
in part through the generation of cis-urocanic acid, tumor necrosis factor, and interleukin-10.28
UVA, much more than UVB, elicits the photosensitivity reactions to cosmetics, drugs, and environmental chemicals, often resulting in the appearance of PIH in darker skin types.29
Visible light
Verallo-Rowell, in a cross-sectional photopatch testing of 20 patients with melasma, compared with 20 without, used VL to irradiate photoallergens.30 In the melasma group, 29 photopatch tests to 11 fragrances, 11 North American Contact Dermatitis Group (NACDG), and 7 plant allergens were (+), relevant, and significant (p = 0.005, CI: 1.54–4.49). A follow-up open study of 20 melasma patients examined the exposed parts of the body. All showed irregular subtle pigmentation in a classic pattern of photosensitivity. The subtlety of the dyschromia was attributed to the “sun-shy” behavior of the all Asian patients. Patch tests with the same photoallergens as the previous study, irradiated with UVA at slightly less than the predetermined Minimal Erythema Dose (MED) elicited (+) to (+++), relevant reactions.31
Melasma cases that worsened instead of improving as expected following intense pulsed light (IPL) therapy prompted a study by Negishi et al. on very subtle epidermal melasma (VSEM).32 Best seen under UV photography, VSEM was described as otherwise “invisible to the naked eye” although photographs “under normal light” appear similar to the subtle melasma and photosensitivity among the sun-shy Asians reported by Verallo-Rowell.31
The importance of these initial observations is relevant to the VL and IRL-emitting lasers and light devices used to treat melasma. We have just started a multicenter, prospective controlled study on the relationship of melasma and photosensitivity. The results of this study may continue to improve our understanding on the specific sunscreens and light devices to use in the prevention and treatment of melasma patients. In this respect, among Negishi et al.’s 223 IPL-treated melasma patients, 63 (28.3%) had VSEM. Of the 45/63 nonusers of sunscreens, 50.6% had VSEM. Of the rest—18/63 who were sunscreen users—only 13.4% had VSEM.32
To summarize, despite outdoor sun avoidance practices, people with darker skin are prone to hyperpigmentations. UVA and VL (much more than UVB) aggravate and elicit photosensitivity, PIH, and melasma. Anti-UVA and anti-VL sunscreens are thus indicated in normal skin to help prevent hyperpigmentations; in the treatment of melasma and other pigmentation problems to inhibit formation, retard proliferation of melanocytes, and protect lightened skin; and overall to facilitate therapeutic effects during and postmelasma treatment. Postlaser and light therapy sunscreens help prevent pigmentations and help avoid the stimulation by light of viable melanocytes. All these also help to avoid potentially more serious sun-related cancers and immunosuppression.33,34
Sunscreens against Lights Emitted by Outdoor/Indoor Light Sources
Outdoors
On the earth’s surface, the amounts of solar UVB and UVA, at a ratio of 20:1, are strongest between 10 A.M. and 4 P.M.22 and vary depending on latitude, altitude, season, time of day, clouds, and ozone layer. Compared with UVB, UVA is of longer wavelength, is less affected by these factors, and can penetrate deeper into the skin.22 Solar VL and IRL are much more abundant, but have longer, thus weaker, wavelengths, which therefore are considered harmless to the skin.22
Indoors
In cars and through windows, clear glass absorbs and acts as a protective shield against the shorter wavelengths (below 320 nm) of UVB.35 Untinted glass allows UVA through. Ordinary tint can block a large portion of UVA up to about 370 to 380 nm, whereas dark-tinted glass containing metals provides significant protection against UVA and VL. This is limited by the U.S. Federal Motor Vehicle Safety Standard,36 which requires that side window glass allow the transmission of at least 70% VL radiation. It has been estimated that approximately 50% of outdoor UVR also occurs indoors, from scatter and reflection on bright surfaces or rippling water.21
In short, for the hyperpigmentation problems of darker skin types who generally avoid the sun but do not use sunscreens: Indoors, where UVA and VL are ubiquitous, daily anti-UVA and anti-VL sunscreens are needed, especially after cosmetic surgery with laser and lights. Outdoors, in addition to the anti UVA and VL, anti-UVB sunscreens are needed. Sun avoidance,37 sunglasses,38 and hats and clothing39 extend skin photoprotection.
Sunscreen Ingredients
Active sunscreen ingredients are best called organic (chemical), or inorganic (physical, chemical-free). Table 12-1 lists the names, light wavelength absorption maximum or range, and their known safety and stability profiles. The U.S.-approved ingredients include 14 organic filters (9 anti-UVB; 5 anti-UVB and A) and 2 inorganic filters.40 Table 12-1 also lists the European–approved sunscreen ingredients.41,42,43,44,45 Two, called the Mexoryls, are made by L’Oreal (Clichy, France): Mexoryl SX41,42,43,44 (terephthalydene dicamphor sulphonic acid) and Mexoryl XL (drometrizole trisiloxane). Both are UVA absorbers at
344- and 345-nm maximum wavelengths. In addition, Mexoryl XL absorbs at UVB with 303 as its maximum wavelength.
344- and 345-nm maximum wavelengths. In addition, Mexoryl XL absorbs at UVB with 303 as its maximum wavelength.
Table 12-1 Absorption, safety, and photostability of some sunscreen ingredients approved by the United States and European Regulatory Boards40 | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||









