Name the six primary muscles of the velopharyngeal mechanism.
Levator veli palatini, tensor veli palatini, musculus uvulae, palatoglossus, palatopharyngeus, superior constrictor.
 Which of these muscles is innervated by V3?
Which of these muscles is innervated by V3?
Tensor veli palatini. (The others are all innervated by from the pharyngeal plexus—IX, X, XI)
 What is the primary function of tensor veli palatini?
What is the primary function of tensor veli palatini?
Opening of the eustachian tube.
 In what direction(s) does the soft palate move to close the velopharyngeal portal?
In what direction(s) does the soft palate move to close the velopharyngeal portal?
Posteriorly and superiorly.
 What muscle is primarily responsible for this movement?
What muscle is primarily responsible for this movement?
Levator veli palatini.
 What muscle is primarily responsible for medial movement of the lateral pharyngeal walls during closure of the velopharyngeal portal?
What muscle is primarily responsible for medial movement of the lateral pharyngeal walls during closure of the velopharyngeal portal?
Levator veli palatini.
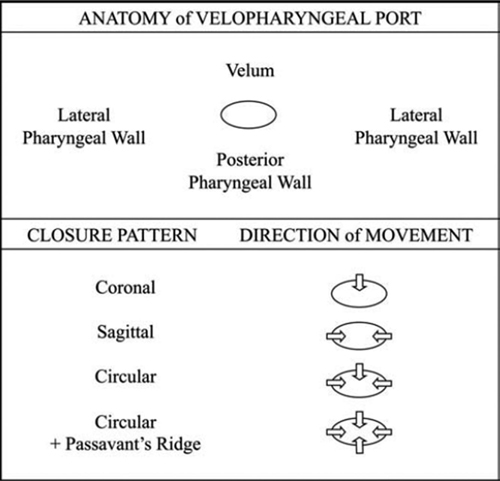
 Name the four patterns of velopharyngeal closure (Fig. 63-1).
Name the four patterns of velopharyngeal closure (Fig. 63-1).
Figure 63-1 Pattern of velopharyngeal closure. (Reproduced with permission from, Fisher DM, Sommerlad BC. Cleft lip, cleft palate, and velopharyngeal insufficiency. Plast Reconstr Surg. 2011;128(4):342e–360e.)
Coronal, sagittal, sphincteric, and sphincteric with Passavant’s ridge.
 What is Passavant’s ridge?
What is Passavant’s ridge?
Transversely oriented ridge on the posterior pharyngeal wall, due to bulging of the fibers of superior constrictor.
 Where does Passavant’s ridge usually lie relative to the level of velopharyngeal closure?
Where does Passavant’s ridge usually lie relative to the level of velopharyngeal closure?
Approximately 1 cm inferior, often does not close the velopharyngeal gap.
 Which arteries supply the soft palate?
Which arteries supply the soft palate?
Lesser palatine artery, ascending palatine branch of facial artery, palatine branches of ascending pharyngeal artery.
 What is the difference between velopharyngeal incompetence (VPI) and velopharyngeal insufficiency?
What is the difference between velopharyngeal incompetence (VPI) and velopharyngeal insufficiency?
VPI is the inability to adequately close the palate against the pharyngeal wall leading to nasal air escape.
Insufficiency refers to an anatomic or structural defect that can be congenital or due to surgery. Examples include: cleft palate, congenitally short palate/large pharynx, or after an adenoidectomy or an ablative surgery.
Incompetence refers to neuromuscular deficit. Examples include: myasthenia gravis, cerebral palsy, stroke, head injury, or upper/lower motor neuron lesions.
 What is rhinolalia aperta?
What is rhinolalia aperta?
Hypernasal speech due to inadequate closure of the velopharyngeal portal.
 Can hypernasality be quantified?
Can hypernasality be quantified?
Yes, with a nasometer. This device uses a nasal microphone, an oral microphone, and a computer to analyze the relative sound output from each source. It calculates the nasalance as a ratio of the nasal acoustic emission to the nasal and oral acoustic emission.
 What is a fricative?
What is a fricative?
Consonant sound produced by the constriction of the air stream to create friction, as in f, v, s, z, th, or sh.
 What distinguishes the different fricatives?
What distinguishes the different fricatives?
Position of the articulators (e.g., the tongue articulates with the teeth for th, and with the alveolar ridge for s or z).
 What is a pharyngeal fricative?
What is a pharyngeal fricative?
Fricative produced by articulation of the tongue base against the posterior pharyngeal wall.
 Name an example of a pharyngeal fricative in normal English speech.
Name an example of a pharyngeal fricative in normal English speech.
There is none. A pharyngeal fricative is used by patients with VPI as a substitute for a normal oral fricative.
 What is a stop plosive?
What is a stop plosive?
Consonant sound produced by the sudden release of intraoral pressure, as in p, b, t, d, k, or g.
 What is a glottal stop?
What is a glottal stop?
Plosive sound made after the adducted vocal cords suddenly open. It is a common misarticulation by patients with VPI. The only example in normal English is “uh.”
 What is a posterior nasal fricative?
What is a posterior nasal fricative?
The back of the tongue articulates against the velum (attempt to close the posterior nasal aperture). This sounds like a nasal snort.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree