Periorbital scarring with eyelid retraction can have serious visual effects and can lead to loss of vision or even loss of the eye. Understanding of eyelid anatomy and the delicate balance of its structural supports is critical for the identification of the eyelid disorder responsible for the cicatrix and helps to guide treatment. The 2-finger test and lateral distraction of the lid can also be of significant help in proper diagnosis of the underlying disorder. Proper reconstruction with respect to the anterior and posterior lamellae helps to ensure a favorable outcome.
Key points
- •
Eyelid reconstruction must respect the anterior and posterior lamella.
- •
Proper identification of the anatomic cause of cicatrix guides treatment.
- •
Appropriate graft selection for eyelid retraction repair is paramount to maintaining proper eyelid function and protection of the eye.
- •
5-Fluorouacil mixed with Kenalog injected into the retracted eyelid can be an effective treatment modality for periorbital scarring.
Introduction
Scar formation around the eyes can be aesthetically unpleasing but can also have serious consequences if not appropriately treated. Correction of eyelid and adnexal tissue presents a unique challenge: not only must defects be corrected but the delicate balance of the support system maintaining the position of the eyelids must be restored and augmented against the contractile forces that occur during healing. Even minor disturbances in the three-dimensional forces that act on the eyelids can lead to debilitating malposition and highly visible esthetic deformity.
As a result, scarring of the eyelid can cause eyelid retraction, entropion, and ectropion, which in turn can lead to exposure keratopathy, corneal scarring, infection, blindness, and even perforation of the globe. Periocular scarring can be one of the most challenging conditions facing surgeons who operate in this area, and a thorough understanding of eyelid anatomy as well as function are essential for proper reconstruction of the lid.
Introduction
Scar formation around the eyes can be aesthetically unpleasing but can also have serious consequences if not appropriately treated. Correction of eyelid and adnexal tissue presents a unique challenge: not only must defects be corrected but the delicate balance of the support system maintaining the position of the eyelids must be restored and augmented against the contractile forces that occur during healing. Even minor disturbances in the three-dimensional forces that act on the eyelids can lead to debilitating malposition and highly visible esthetic deformity.
As a result, scarring of the eyelid can cause eyelid retraction, entropion, and ectropion, which in turn can lead to exposure keratopathy, corneal scarring, infection, blindness, and even perforation of the globe. Periocular scarring can be one of the most challenging conditions facing surgeons who operate in this area, and a thorough understanding of eyelid anatomy as well as function are essential for proper reconstruction of the lid.
Anatomy
The function of the eyelids is to lubricate and protect the cornea and conjunctival surface. Incomplete closure or lagophthalmos can lead to ocular surface decompensation and vision loss. The lower eyelid should rest at the inferior limbus and the upper eyelid should sit 1 to 2 mm below the superior limbus with the eye open. Scleral show, or visualization of the sclera above or below the limbus, suggests upper or lower eyelid retraction respectively.
One of the most important anatomic concepts for eyelid surgery is the anterior and posterior lamella, which can be separated along the gray line on the lid margin. Some investigators describe a middle lamella, making the eyelid a trilaminar structure. Reconstruction without respect and attention to these structures is likely to result in unfavorable outcomes. The anterior lamella is composed of the skin and orbicularis muscle ( Fig. 1 ). The skin of the eyelid has no subcutaneous fat and is the thinnest skin in the body. The orbicularis oculi muscle is the protractor of the eyelid and is divided into the pretarsal, preseptal, and orbital portions. The pretarsal and preseptal portions are responsible for involuntary closure of the lid, whereas the orbital portion is responsible for forced closure. Scarring of the anterior lamella often leads to eyelid retraction and/or eyelid ectropion.
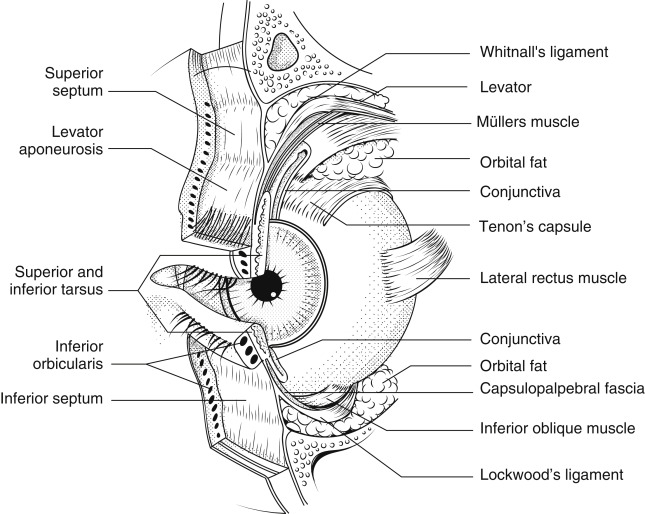
The posterior lamella consists of the tarsus and conjunctiva. The conjunctiva is a nonkeratinized mucous membrane that lines the eyelid and the sclera. It contains goblet cells that secrete mucus to lubricate the eye as well as accessory lacrimal glands that contribute to the aqueous layer of the tear film. There is redundancy of the conjunctiva deep in the fornix to allow proper movement of the globe. Scarring of the conjunctiva and symblepharon formation can cause restriction of the eye, resulting in diplopia. The tarsus is located anterior to and firmly adherent to the conjunctiva. The tarsal plates are formed of dense fibrous connective tissue and provide structural integrity to the lids. The height of the tarsus in the upper eyelid is around 8 to 12 mm and 3.5 to 5 mm in the lower lid. The tarsus tapers medially and laterally before condensing in to the medial and lateral canthal tendon respectively. Scarring of the posterior lamella can lead to eyelid retraction and/or entropion.
The middle lamella consists of the tissue between the anterior and posterior lamella inferior to the tarsal plate, which includes the orbital septum, the preaponeurotic fat pad, and the lower eyelid retractors. Scarring of the middle lamella can cause eyelid retraction, entropion, and even ectropion. Scarring of the middle lamella is often caused by trauma or surgery.
The medial and lateral canthal tendons attach the tarsal plate to the periosteum of the orbital rim, providing support for the eyelid ( Fig. 2 ). The medial canthal tendon separates into an anterior and posterior portion. The anterior portion extends to the anterior lacrimal crest on the frontal bone and provides the major support for the medial canthal angle. The posterior portion inserts on the posterior lacrimal crest and provides posterior tension on the eyelid, maintaining close approximation to the globe. The anterior and posterior portions of the medial canthal tendon surround the lacrimal sac and play an important role in the lacrimal pump mechanism. Any reconstruction of the medial canthal tendon should respect the lacrimal drainage system and be designed to provide appropriate support and posterior tension.
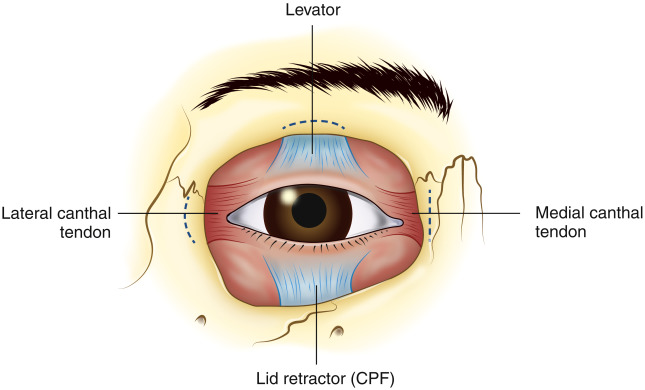
The lateral canthal tendon provides support of the lateral eyelid and inserts at the lateral orbital (Whitnall) tubercle 3 to 4 mm deep to the lateral palpebral raphe. The posterior insertion of the lateral canthal tendon is important to recreate during reconstruction to provide adequate contact between the eyelid and globe. The lateral canthus lies 2 to 4 mm higher than the medial canthus (with some variation by age and race) and periorbital scarring can distort this cosmetically and functionally important upward slant to the eyelid.
Evaluation
The goal of scar revision and eyelid reconstruction is to provide a functional and aesthetically pleasing result. Often these two outcome goals are related. Evaluation of the scarring and retraction should identify the cause of retraction. The lid should be evaluated for anterior lamellar shortening, posterior lamellar shortening, middle lamellar shortening, canthal tendon laxity, or a combination of these variables. Eyelid retraction may present as an entropion, ectropion, or simply as eyelid retraction. Identification of the anatomic abnormality is paramount to proper scar revision and retraction repair.
The 2-finger test ( Fig. 3 C ) is useful to help identify the disorder causing the eyelid retraction. In this test, 2 fingers are placed on the skin below the eyelid and the skin is elevated superiorly. This test provides extra anterior lamellar skin to the periorbital area. When applying superior traction to the skin, pay attention to the eyelid margin. If after elevation of the skin, the lid moves superiorly and the retraction is resolved, the cause of retraction is likely deficiency of the anterior lamella. If the lid does not move and the traction remains despite providing adequate skin to the lid, the retraction is likely caused by posterior or middle lamellar cicatrix.
The laxity of the eyelid must also be considered when evaluating eyelid retraction. The cause of eyelid malposition may be canthal tendon weakness. In many cases there is a combination of lid laxity as well as lamellar shortening and both pathologic states must be addressed for proper repair. The lower lid distraction ( Fig. 3 B, I) can be used to measure lid laxity. In this test, the lid is pulled anteriorly away from the globe and a distraction of greater than 6 mm is considered abnormal. The snap back test can also be used to test for lower lid laxity. The lid is pupped away from the globe and released. The lid should return to its position on the globe without blinking.
Another helpful examination technique for evaluating eyelid malposition is using a finger to place lateral traction on the lid. If lateral tension on the lid corrects an observed entropion or ectropion the eyelid malposition may be caused by eyelid laxity and possibly disinsertion of the eyelid retractors.
Ectropion occurs when the eyelid margin everts from the globe. This condition can be caused by cicatricial change, paralysis of the orbicularis muscle, or can be involutional, and can result in excessive evaporation of the tear film and epiphora. Applying the examination techniques discussed earlier can be helpful to identify the cause and direct treatment. If the 2-finger test is applied and the lid margin remains retracted, the ectropion is likely caused by a middle lamellar deficiency and should be corrected with scar lysis and middle lamellar augmentation. If the lid margin is elevated with superior traction on the lid, lateral traction should then be applied. If the ectropion corrects, the retraction may be caused by eyelid laxity and may be corrected with an eyelid tightening procedure such as a lateral tarsal strip. If the retraction improves with 2-finger elevation but does not correct with lateral tension on the lid, the disorder is likely caused by anterior lamella deficiency and can be corrected with anterior lamella augmentation ( Fig. 4 ).
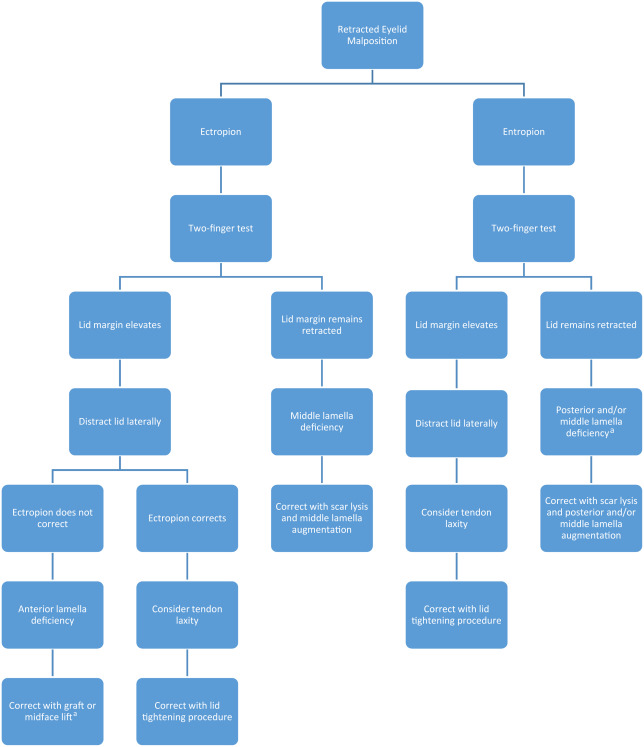
Entropion occurs when the lid margin turns posteriorly toward the globe. The lashes and keratinized skin rubbing against the eye can cause mechanical damage to the cornea and conjunctiva and can cause extreme pain and irritation. Entropion can be caused by cicatrix, but is most commonly caused by involutional change. Evaluation of an entropion can also be aided by the examination techniques described earlier. If the 2-finger test is applied and the lid margin elevates and the entropion improves with lateral tension on the lid, the entropion is likely involutional and can be corrected with a lid tightening procedure. If the lid remains retracted after the 2-finger test the entropion is likely caused by posterior and middle lamella deficiency and should be treated with scar lysis and lamella augmentation (see Fig. 4 ).
Surgical correction
Optimization of scar outcome is best done during the initial operation, whether it is repair of a traumatic or oncologic deformity. Prevention of unfavorable outcomes requires meticulous attention to reconstruction of anatomic layers, restoration of underlying support structures, and precise suturing technique with wound edge eversion as appropriate. Consideration can then be given to adjuvant postoperative therapies such as topical silicone gel or laser camouflage as described elsewhere in this issue.
For proper scar revision and retraction repair, the anterior and posterior lamella must be reconstructed separately. Once the disorder has been identified by proper examination techniques and observation of lid movement, the malposition can be appropriately addressed. The anatomic function of each layer of the eyelid must be respected. The thin skin of the anterior lamella must be matched as closely as possible to allow the natural dynamic movement of the eyelid blink. Full-thickness skin graft options include the contralateral eyelid skin, posterior auricular skin, and supraclavicular skin. Graft donor sites should be free of hair, as well as evidence of malignancy, and care should be taken to ensure the closest color and texture match. Partial-thickness skin grafts have a high contraction rate and are not well suited for anterior lamellar grafting. The orbicularis should be preserved if possible to provide adequate closure and tonic tone of the eyelid.
The posterior lamella including the tarsus and conjunctiva should also be reconstructed if necessary. The tarsus provides structural support for the eyelid and is important to maintain stability of the eyelid margin. The conjunctiva provides a smooth mucosal surface that is in constant contact with the eye and is important to help prevent mechanical damage to the cornea and conjunctiva.
Cicatricial Retraction with Ectropion
Anterior lamellar shortening may be caused by trauma, overly aggressive lower eyelid blepharoplasty with skin removal, actinic changes, or after excision of eyelid malignancies. If the anterior lamella has been identified as insufficient by the 2-finger test, local flaps such as Z-plasties can be considered to direct tension horizontally instead of vertically. Elevation of the midface may also provide adequate anterior lamellar skin to resolve the retraction. Some regression of surgical effect can occur with these procedures.
Anterior lamellar skin grafting is the gold standard for cicitrical ectropion.
- 1.
A subciliary incision is marked after identifying the scar tissue to be lysed, taking care to extend the lysis beyond the cicatrix.
- 2.
Local anesthetic with epinephrine is injected into the eyelid with a 30-gauge needle.
- 3.
Place two 4.0 silk sutures into the lid margin to provide traction.
- 4.
Make a subciliary incision with a number 15 Bard-Parker blade.
- 5.
Use sharp dissection with Westcott scissors to lyse all scar tissue.
- 6.
With the eyelid on traction with the silk sutures, mark a template for the full-thickness skin graft.
- 7.
Harvest a full-thickness skin graft from the contralateral upper eyelid, supraclavicular skin, or posterior auricular skin.
- 8.
Thin the graft, removing any subcuticular fat with scissors.
- 9.
Suture the graft into place using 5.0 fast gut suture or 6.0 nylon suture and cover the graft with ophthalmic antibiotic ointment.
- 10.
Tape the 4.0 traction silk sutures to the forehead to provide traction.
- 11.
Tie a bolster over the graft with 4.0 silk sutures.
- 12.
If there is any eyelid laxity, a lid tightening procedure such as a lateral tarsal strip should be performed. This procedure also provides tension during the healing process to decrease further cicatrix.
The bolster and traction sutures are removed after 1 week. The lid may appear overcorrected and the graft may be dark, but this typically resolves with healing. Massage is encouraged after 2 weeks.
Cicatricial Retraction with Entropion
Posterior lamellar cicatrix can be caused by trauma, surgery, chemical injury, ocular cicatricial pemphigoid, Stevens-Johnson syndrome, trachoma, and chronic inflammation. If the cicatrix is caused by inflammatory disorders, ideally surgical intervention should be delayed until the disease is quiescent if possible.
There are many options for posterior lamellar spacing for correction of eyelid retraction and entropion. Free tarsus grafting from the contralateral upper eyelid is ideal because it is matched tissue and has conjunctival lining attached. Hard palate is considered to be an excellent option because of its structural rigidity and mucosal lining, although caution should be exercised because the hard palate mucosa is keratinized and can cause corneal irritation and damage. Auricular cartilage can be effective because of its rigidity, but it can become lumpy and can be associated with eyelid thickening. Xenografts (EnduraGen; Stryker Corporation, Newnan, GA) and Acellular dermis matrix allografts (AlloDerm; LifeCell Corporation, Branchburg, NJ) are associated with a high rate of retraction and resorption but are often used because a donor site is not needed. Upper eyelid grafting is particularly important because it comes in contact with the cornea and the authors prefer free tarsal grafting from the contralateral eyelid if possible.
Cicatricial Retraction with Entropion: Correction with Free Tarsal Graft
Harvesting graft
- 1.
Local anesthetic with epinephrine is injected into the pretarsal orbicularis on the contralateral upper eyelid of the recipient site ( Fig. 5 ).








