This article provides a review of the surgical and nonsurgical options available to manage a variety of auricular scars. The basics of wound healing are discussed in addition to the etiology of keloids and the cauliflower ear. Many auricular scars can be revised with scar excision techniques, but separate discussions for the treatment of keloids and the cauliflower ear are provided. The management plan for auricular scarring requires appropriate patient counseling regarding the risk of recurrence in keloids, regrowth of scar tissue in cauliflower ears, scar hypertrophy at the line of closure, widening of the scar, and persisting ear contour deformities.
Key points
- •
Auricular skin does not have much laxity. Providing tensionless closure during scar repair helps minimize further scarring and ensures a favorable aesthetic result.
- •
Small keloids may be amenable to simple excision but larger and recurrent keloids are best managed with surgery and an adjuvant therapy.
- •
The cauliflower ear is often managed surgically. The most effective preventative measure is complete evacuation of the preceding auricular hematoma.
Introduction
Scarring represents an inextricable component of the healing process. From healing minor abrasions to restoring some measure of structural integrity, scarring is an inevitable outcome. Certain aesthetic and functional sequelae of scarring in the auricular region are important to understand. The external ear has inherent aesthetic value that warrants appropriate restoration during any form of reconstruction, and this has been recognized for centuries. The Sushruta Samhita , an ancient subcontinental Indian text, provides a description of a crude ear lobe reconstruction using a pedicled cheek flap dating back to 600 bce . Since then, enough medical and surgical experimentation has been completed to formulate treatment options for scarring in the auricular region.
Introduction
Scarring represents an inextricable component of the healing process. From healing minor abrasions to restoring some measure of structural integrity, scarring is an inevitable outcome. Certain aesthetic and functional sequelae of scarring in the auricular region are important to understand. The external ear has inherent aesthetic value that warrants appropriate restoration during any form of reconstruction, and this has been recognized for centuries. The Sushruta Samhita , an ancient subcontinental Indian text, provides a description of a crude ear lobe reconstruction using a pedicled cheek flap dating back to 600 bce . Since then, enough medical and surgical experimentation has been completed to formulate treatment options for scarring in the auricular region.
Relevant anatomy and embryology
The auricle, or pinna, is the visible external component of the ear. At approximately the sixth week of gestation, the external ear develops from the proliferation of the first and second branchial arch mesenchymal cells. The tragus, helical crus, and helix are derived from the first branchial arch (Meckel cartilage). The antihelical crus, antihelix, lobule, and antitragus are derived from the second branchial arch (Reichert cartilage). The auricle reaches full adult size in many cases by 5 years of development. The external ear is formed by a framework of elastic cartilage and perichondrium with tightly adherent overlying skin, particularly over the anterior surface. The lobule is the singular noncartilaginous component, formed by a wedge of adipose tissue. The presence of only scant subcutaneous tissue necessitates careful surgical planning to preserve cosmetic auricular structure. The anterior surface of the average auricle consists of a skin envelope only 0.8 mm to 1.2 mm in thickness, firmly attached to the underlying perichondrium. In comparison, the posterior surface of the auricle bears an additional layer of fat that affords greater skin mobility and a total cumulative thickness of 1.2 mm to 3.0 mm.
Basics of cutaneous wound healing
Scarring is an irreplaceable component of wound healing, which tends to follow a predictable pattern. Although an exhaustive explanation of the process is beyond the scope of this article, a fundamental understanding of cutaneous wound healing can shed insight on how to anticipate scarring from a therapeutic perspective.
The 3 steps of wound healing include inflammation, proliferation, and remodeling, which collectively involve a web of interactions among cytokines, vascular elements, parenchymal cells, and extracellular matrix. After tissue injury causes the disruption of blood vessels, degranulating platelets work to form a hemostatic plug and secrete wound-healing mediators, including platelet-derived growth factor (PDGF) and transforming growth factor-β (TGF-β). These growth factors are released by multiple cell types in an inactive form. Re-epithelialization of cutaneous wounds begins within hours of the initial insult, facilitated by epidermal cells migrating from skin appendages (eg, hair follicles). Wound healing continues with the formation of granulation tissue and neovascularization until fibroblasts undergo a phenotypic change to become myofibroblasts that participate in wound contraction and extracellular matrix reorganization. The transformation from granulation to scar tissue is contingent on the catabolism of collagen, which is achieved via matrix metalloproteinases. Although scarring allows the reclamation of some measure of integrity, wounds only have the opportunity to gain 20% of their final total strength within the first several weeks after the insult. Scar tissue, at maximal strength, is 70% as strong as native skin tissue.
Keloids
Although benign in nature, keloids and hypertrophic scarring represent clinical challenges. Keloids were already recognized in ancient times as unusual tissue growth. They were referenced in the Smith papyrus from approximately 1700 bce . The term keloid is derived etymologically from the Greek word, chele , which translates roughly to “claw of [the] crustacean,” an apt reference to the tenacious grasp with which keloids resist definitive treatment.
The auricular region is a well-recognized site for keloid formation after iatrogenic, incidental, or planned traumatic insult, including burns, ear piercings, and otoplasty. Keloid scarring, by definition, extends beyond the borders of the original trauma and tends to have limited prospect of natural regression (a characteristic that distinguishes it from hypertrophic scarring). It occurs with a frequency in the nonwhite population 15 times that in the white demographic.
Although they remain prevalent, keloids have eluded a definitive pathophysiologic explanation. In normal skin, collagen bundles run parallel to the epithelial surface; however, types I and III collagen exist in random orientation within keloid scars. Not only is the collagen production disorganized in keloids but also it is amplified—20 times as prevalent than in normal skin. Keloid formation is known to occur only in humans.
Multiple theories have been postulated regarding the etiology of keloids. Several novel studies have focused on the aberrant production of various growth factors, including TGF-β and PDGF, which are involved in the chemotaxis and proliferation of keloid fibroblasts. Chen and Davidson report that there are low concentrations of TGB-β in the fetal wound environment, which is significantly less prone to scarring. Aberrant scar formation is also compounded by diminished synthesis of matrix metalloproteinases and higher relative apoptotic rate of normal fibroblasts compared with keloid fibroblasts. In any case, keloid formation is likely the culmination of multiple derangements in the wound healing process.
Hypertrophic scarring
The important clinical distinction between hypertrophic scarring and keloid is the theoretic potential for regression and the tendency to remain within the confines of the original wound. From a histologic standpoint, hypertrophic scarring consists of type III collagen bundles (apparently absent in keloids), which are oriented relatively parallel to the epithelial surface. Both types of aberrant scarring, however, are characterized by overexpression of both TGF-β and PDGF, suggesting similar pathologic derangement in the wound healing signaling process. Unlike the tendency of keloids, hypertrophic scarring has not been found more prevalent in the nonwhite population.
Auricular hematoma and cauliflower ear
Much like keloid scarring, auricular hematomas and their associated chondropathology are a well-recognized entity. Visual representations of the cauliflower ear, as it is known colloquially, are recorded in the annals of ancient Greek and Roman accounts as a stigmata of boxing, wrestling, and the ancient sport of pankration. The first published description of auricular hematomas as a precursor to the auricular chondropathology, was written by Bird in 1833. He described 6 cases of “inflammation of the auricle,” and reported the following: “the auricle…getting hot…getting more red and even bluish” before “it will feel very hard rather soon.”
A more contemporary explanation for the development of the cauliflower ear is based on the result of blood collecting between the auricular perichondrium and the auricular cartilage. The blood clot essentially separates the underlying cartilage from its oxygen and nutrient source—the perichondrium. This was first recognized by Ohlsén and colleagues, in which rabbit ears were injected with blood in multiple locations. Park and colleagues describe their own experience with recalcitrant auricular hematomas, observing that unsuccessful management with aspiration and bolster dressings was a result of hematomas that were intracartilaginous instead. In most cases, undisturbed or residual hematomas recruit fibroblasts to create fibrosis. There also may be areas of potential neocartilage formation within the fibrotic tissue. Eventually, the resultant appearance within the auricular soft tissue is one that resembles that of a cauliflower ( Fig. 1 ).
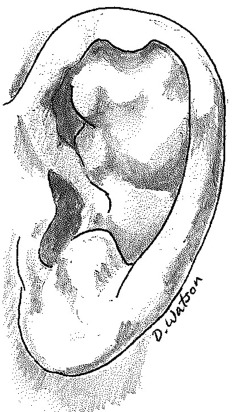
In addition to being an aesthetic deformity, cauliflower ear that involves the concha can create external canal stenosis. Noormohammadpour and colleagues comment on the higher incidence of audiometry-confirmed hearing loss in wrestlers affected by cauliflower ear, which is attributed to obstruction of the external auditory canal and disruption of the inherent cerumen expelling process.
Scars from rhytidectomies
Preauricular and postauricular incisions are standard for most rhyditectomy procedures. Poor wound closure technique and excess tension at the incision contribute to unsightly scars and scar widening. Scarring that results from postauricular flap necrosis after a rhytidectomy is 12.6 times likely in smokers, due to the toxic effects of nicotine on vascular supply in random-pattern flaps.
To address closing tension issues across rhytidectomy incisions, Knize described his experience using a force measurement instrument to quantify the force required to advance facialplasty flaps to the periauricular position, realizing that the force applied to the superficial muscular aponeurotic system flap approximates 1 kg. Similar force vector measurements were made on the same cohort of 20 ears for postauricular skin closure (approximately 0.5 kg). From his results, Knize recommended the internal splinting technique, which uses auricular cartilage as a functional anchor in 4 positions (anterior, inferior to the antitragus, superior auricular sulcus, and posterior auricular sulcus) for the facelift soft tissue advancement planes using 3-0 polyglactin sutures. He suggests that the auricular cartilage can sustain up to 5 kg of force before manifesting signs of aesthetic deformity. In addition to relieving tension, the superior auricular sulcus anchor suture offers the benefit of preventing superior advancement of the temporal hairline.
Management and treatment
General Principles of Scar Revision
Surgical scar management, particularly in the auricular region, requires careful planning. Certain immutable guidelines govern scar creation and revision in most areas. The ideal placement of a scar, revised or not, would follow a natural skin crease or relaxed skin tension line (RSTL) to maximize imperceptibility and to minimize the tension across the wound. RSTLs may not be readily apparent in youthful skin. In this situation, it may be beneficial for the clinician to ask the patient preoperatively to exaggerate facial expressions to reveal their RSTLs. In addition, proper suture technique (eg, adequate wound eversion) is an important component that helps optimize scar cosmesis. A final consideration prior to planning scar revision is timing. It is prudent to allow the normal scar an adequate amount of time to achieve its mature appearance prior to opting for surgical intervention. Hypertrophic and keloid scars, on the other hand, are candidates for earlier treatment.
Surgical Repair Options
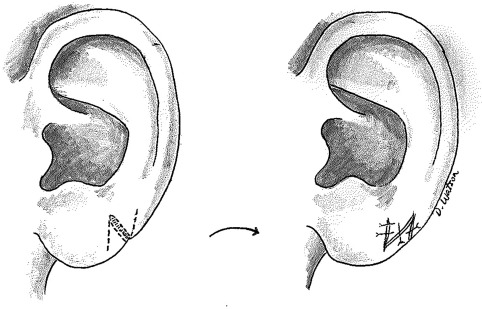
Fusiform elliptical excision
The fusiform elliptical excision represents a simple method of scar excision, with the angles of the elliptical apices measuring 30° or less to prevent the formation of the dog-ear deformity. After undermining the surrounding skin to relieve tension, multiple layers of closure are completed to accomplish adequate wound eversion ( Fig. 2 ).
W-plasty scar revision
The W-plasty and the geometric broken line closure (GBLC) are methods of scar irregularization, predicated on the principle that irregular lines are less perceptible than linear scars. Both of these methods are of particular utility in scars that are not oriented parallel to RSTLs. The W-plasty technique is performed by creating opposing zigzag lines on each side of the scar and to interdigitate them during closure. Ideally, the points of the resulting W shape run parallel to RSTLs or natural skin folds. The arms of the W should be approximately 5 mm in length and angled between 60° and 90°. The surrounding tissue is undermined, and the zigzagged edges of the excised scar are reapproximated with multiple layers of closure.
Geometric line scar revision
The GBLC technique is the more exaggerated scar irregularization method preferred in longer scars typically on the face. The GBLC method entails incising a series of random geometric shapes (eg, semicircles, squares, and triangles) from one side of the scar and corresponding-shaped excisions on the contralateral edge of the scar. The excised scar is then reapproximated with a multilayer closure.
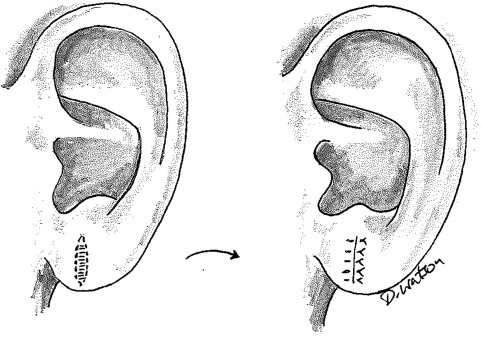
Z-plasty scar revision
The Z-plasty technique is used to lengthen irregularly contracted scars and alter the direction of a scar that is opposed to an RSTL or natural skin crease. Although the scar acts as the common limb of the Z, 2 triangular flaps are incised and switched with each other. Geometric configurations are critical to the Z-plasty method, because the angles of the designed triangles determine the linear gains after transposition. The technique also carries the advantage of being able to realign landmark facial structures distorted by scarring ( Fig. 3 ).