6. Perioperative Anesthesia Considerations for the Aesthetic Surgery Patient
Deborah Stahl Lowery
Anesthesia is an important consideration in any aesthetic procedure. Close communication between the anesthesiologist, surgeon, and patient are paramount to a safe and successful surgery. Risk stratification, proper patient selection, and optimization are needed to decrease complications.
CARDIOVASCULAR DISEASES1–6
HYPERTENSION
■ Continue preexisting beta-blocker on day of surgery (DOS).
■ Hold diuretics on DOS.
■ Hold ACE inhibitors (lisinopril, ramipril, benazepril, captopril) and angiotensin-receptor blockers (ARBs) (candesartan, losartan, valsartan, irbesartan) on DOS because of exaggerated hypotension with induction of general anesthesia.
CORONARY ARTERY DISEASE
CAUTION: Defer elective surgery if diagnosed within the last 6 months.
■ If history of angioplasty or stents: How many, when implanted, type, need for ongoing antiplatelet therapy or anticoagulation? This is important! Consult with cardiology or primary care physician (PCP).
■ Cardiomyopathy
■ Valvular disease
• Aortic stenosis is always a concern (determine mild, moderate, severe).
• Note any cardiac implantable electronic device (CIED) such as pacemaker or automated implantable cardioverter defibrillator (AICD).
NOTE: With bipolar electrocautery ONLY, the chance of adverse CIED interruption is minimal; safe for ambulatory surgery center office.
CONGESTIVE HEART FAILURE (CHF)
■ Consider only stable, well-compensated chronic CHF for low-risk procedures.
CEREBROVASCULAR DISEASE
■ Evaluate if there is a history of TIA or CVA, including presence of any residual effects.
PERIPHERAL VASCULAR DISEASE
■ Pacemakers (elective surgery) should have device checked within last 12 months.
■ Defibrillators (elective surgery) should have device checked within last 6 months.
■ If monopolar electrocautery is necessary, consider doing these cases in hospital setting.
PULMONARY DISEASES
PULMONARY HYPERTENSION
■ Patients with severe pulmonary hypertension are high risk and should not undergo elective cosmetic surgery.
ASTHMA3,9,10
■ Prevalence in United States is 8.2%
■ Closed claim analysis indicates incidence of intraoperative bronchospasm or laryngospasm is as low as 2%, but 90% of these type claims were for severe brain injury or death.
■ Preexisting, well-controlled asthma has been associated with low increased risk of bronchospasm (1.7%).10
■ Most authors conclude patients with well-controlled asthma are acceptable for ambulatory surgery.
CHRONIC OBSTRUCTIVE PULMONARY DISEASE (COPD)3,10–12
■ Identified as independent risk factor for increased morbidity and mortality and unplanned intubations
■ Most frequent risk factors for postoperative complications include atelectasis, pneumonia, respiratory failure, and COPD exacerbation.3
• Choose a facility that allows extended PACU stay or 23-hour observation.
■ Highest risk for hypoxia and hypoventilation is in the immediate postoperative period.
SMOKING10,13
■ Patients who smoke >1–2 packs per day are at increased risk for perioperative respiratory complications, wound infections, flap necrosis.
■ Smoking cessation immediately before surgery may not improve patient outcome and may actually cause increased risk of pulmonary complications because of increased secretions and increased airway reactivity.
■ Although no definitive consensus exists in literature, Centers for Disease Control (CDC) recommends at least 30 days of smoking cessation before and after surgery.
POSTOPERATIVE PULMONARY COMPLICATIONS (PPCS)10,14
■ Rate across all types of surgery is 6.8%, according to recent systematic review.
■ More prevalent in patients with known underlying disease
■ Clinically significant complications include:
• Atelectasis
• Infection, bronchitis, or pneumonia
• Respiratory failure that could result in reintubation or continued mechanical ventilation
• Exacerbation of preexisting chronic conditions
• Bronchospasm
■ Patient-related risk factors
• Poor functional status
• Poor general health status
► ASA PS class has good correlation with risk.
► ASA >II confers almost fivefold increase in risk.
• Increasing age >50 years
• Smoking
• Obesity
■ Procedure-related risk factors
• Site of surgery is single, most important factor.
► Abdominal (upper > lower) or thoracic surgery
► Abdominoplasty or massive-weight-loss procedures should promote caution.
• Duration >3-4 hours
• Type of anesthesia, neuraxial or regional, may confer benefit.
• Residual neuromuscular blockade
■ PPCs are associated with increased mortality, increased length of stay, and increased cost of care.
OBSTRUCTIVE SLEEP APNEA (OSA)15–17
BACKGROUND
■ Rising incidence in United States
■ Male/female ratio 3:1
■ Clinical correlation with obesity
■ High index of suspicion for difficult airway
■ Remains largely undiagnosed in up to 80% of patients
■ Episodic airway obstruction results in sleep disruption/disorder and daytime hypersomnolence.
■ Apnea defined as cessation of airflow from mouth or nose for >10 seconds
■ Hypopnea defined as 50% reduction in airflow that causes slow respiration for >10 seconds
■ Physiologic derangement includes:
• Oxygen desaturation/hypoxia
• Hypercarbia
• Acidosis
• Polycythemia
■ Polysomnography is the standard diagnostic test?determines apnea-hypopnea index and stratifies into mild, moderate, or severe.
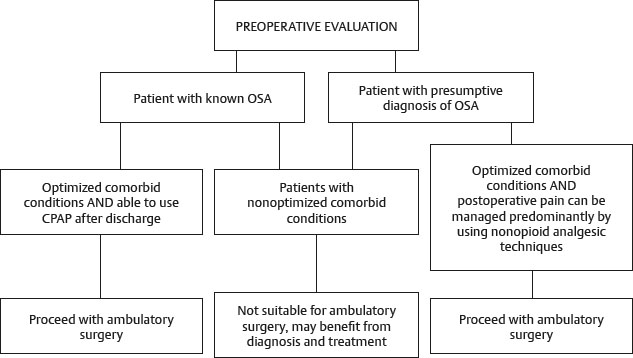
PREOPERATIVE ASSESSMENT
■ American Society of Anesthesiologists (ASA) strongly recommends anesthesiologists and surgeons work together to develop protocols to evaluate patients before the day of surgery to aid in patient selection, preparation, and management.
■ STOP-BANG questionnaire most commonly used and recommended in SAMBA (2014) Consensus Statement on OSA and Ambulatory Surgery 17 (Fig. 6-1)
1. Do you Snore loudly? Yes/No
2. Do you feel Tired, fatigued, or sleep during the daytime? Yes/No
3. Has anyone Observed you stop breathing during your sleep? Yes/No
4. Have you been or are you now being treated for high blood Pressure? Yes/No
5. Is your Body Mass Index greater than 35 kg/m2? Yes/No
6. Are you over 50 years of Age? Yes/No
7. Is your Neck circumference greater than 40 cm? Yes/No
8. Gender (male)? Yes/No
Fig. 6-1 STOP-BANG questionnaire used for screening patients to determine the risk of OSA. Fewer than three questions positive = low risk of OSA; three or more questions positive = high risk of OSA; five to eight questions positive = high probability of moderate to severe OSA.