I. DEVELOPMENT
A. Structures are derived from
1. Mesoderm (wolffian/müllerian ducts)
2. Endoderm (cloaca, membrane)
3. Ectoderm (external genitalia)
B. Wolffian ducts: Epididymis, vas deferens, and seminal vesicles
C. Müllerian ducts: Fallopian tubes, uterus, and upper two-third of vagina
D. Gonads begin as ridges, differentiate after 6 weeks
E. Male differentiation
1. H-Y antigen on Y chromosome initiates gonadal differentiation into testes.
2. Testes contain Sertoli cells and Leydig cells.
3. Müllerian inhibiting substance (MIS) secreted from sertoli cells in testes causes regression of müllerian ducts.
4. Leydig cells produce testosterone analog → development of Wolffian ducts
5. Dihydrotestosterone → virilization of external genitalia
F. Female differentiation
1. Female differentiation is the default.
2. No H-Y antigen → gonads become ovaries, no MIS and Müllerian ducts develop
II. ANATOMY
A. Male
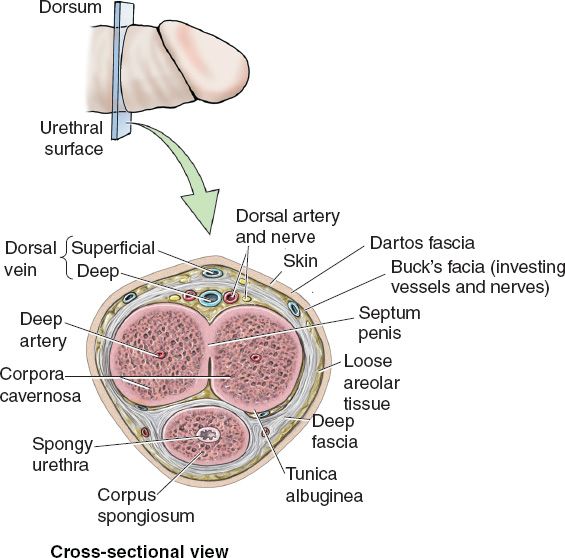
1. Penis: Superficial to deep (Fig. 53-1)
a. Skin
b. Dartos (superficial) fascia
c. Buck (deep) fascia
d. Neurovascular bundle: Deep dorsal vein, dorsal artery, paired dorsal penile nerves.
e. Tunica albuginea (surrounds each corpora individually).
f. Erectile tissue: Paired corpora cavernosa, corpora spongiosum surrounds urethra.
2. Arterial supply. Internal pudendal artery branches into
a. Perineal artery to perineum and scrotum.
b. Common penile artery branches to bulbourethral artery, dorsal artery, deep cavernosal artery.
3. Urethral divisions
a. Posterior: Proximal to the bulb (prostatic and membranous portions).
b. Anterior: Distal to bulb; contained within corpus spongiosum (bulbar and penile/pendulous portions, fossa navicularis).
III. PENILE RECONSTRUCTION
A. Goals of reconstruction
1. Sufficient length and adequate skin for unrestricted erections.
2. Protective sensation to prevent chronic skin breakdown.
3. Ability to spontaneously void standing up.
4. Erectile function.
______________
*Denotes common in-service examination topics
Figure 53-1. Cross-sectional anatomy of the penis (From Agur AMR, Dalley AF, eds. Grant’s Atlas of Anatomy. 12th ed. Lippincott Williams & Wilkins; 2008.)
B. Defects of penile surface
1. Can occur due to SCC of shaft, glans, or traumatic injury
2. Split thickness skin graft (STSG) or full thickness skin graft (FTSG) are viable options.
3. Urethral exposure requires more durable coverage with local flap.
C. Peyronie’s Disease: 1% males age 40 to 60 years
1. Painful erections, chordee curvature, firm nodules or plaques on shaft, 10% have Dupuytren’s contracture.
2. Plication procedure: Circumcising incision with degloving of shaft. Tunica albuginea opposite area of maximal curvature is identified and an ellipse excised. This will slightly shorten the penis but correct curvature.
3. Evaluation: Requires Doppler ultrasound of induced (pharmacologic) erection.
4. Treatment options
a. Inflammatory phase: Vitamin E may help
b. Mild disease/sexually functional: Treatment discouraged
c. Advanced disease/sexually disabled
i. Implant prosthesis if impotent.
ii. Plication procedure (mild curve, 30 to 45 degrees): Excise ellipse of tunica from opposite side; shortens penis slightly.
iii. Excision/dermal graft (curves >45 degrees): Excise plaques and use defatted dermal graft for patch.
iv. Erections avoided for 6 weeks; full recovery takes months.
5. Outcomes
a. 10% to 15% rate of impotence post-op: Venous leak phenomenon versus psychogenic.
b. 85% successful (straight penis, spontaneous erections, and successful intercourse).
1. Indicated for sharp, nonavulsive injuries.
2. Contraindications include gross contamination, extended warm ischemia time >8 hours.
3. Relative contraindication is self-mutilating injury and uncontrolled psychiatric disease.
4. Must perform debridement of nonviable tissue, and dissection of two dorsal arteries, two dorsal veins, two dorsal nerves for anastomosis.
5. Spatulated urethral repair over Foley catheter.
6. Direct repair of tunica albuginea or corporal bodies.
7. *End-to-end anastomoses of dorsal arteries and veins
8. Close Buck’s fascia and skin
9. Dressings must be supportive, Foley × 2 to 3 weeks to prevent urethral stricture.
IV. SCROTAL RECONSTRUCTION
A. Fournier’s gangrene: Necrotizing fasciitis of the perineum
1. Higher incidence in immunosuppressed and those with diabetes.
2. Mixed aerobic/anaerobic bacteria.
3. Fournier’s gangrene is a surgical emergency. Mechanical debridement is necessary to control infection.
4. Testes are often spared of direct infection secondary to independent blood supply and lymphatic drainage.
5. Scrotal defect—STSG over testes which are sutured together in midline, meshed graft. Medial thigh pockets are a temporary option as higher temperature will alter sperm production.
V. MALE PERINEAL DEFECTS ARE MOST COMMONLY ENCOUNTERED SECONDARY TO CANCER RESECTION
A. Patients s/p XRT have high risk of delayed wound healing and fistulas.
B. Flap options
1. Vertical rectus abdominis musculocutaneous flap (VRAM): Obliquely oriented skin paddle may give more length to traverse the very long and narrow male pelvis. Be cautious with patients requiring lifelong ostomies (s/p abdominopelvic resection for rectal cancer).
2. Pedicled anterolateral thigh flap (ALT) flaps based on descending branch of lateral circumflex femoral artery: Tunnel under sartorius and rectus femoris.
3. Bilateral gracilis: Myocutaneous, or muscle only flaps with primary closure over the flap or STSG.
4. Bilateral posterior thigh flaps.
5. Singapore flap.
VI. VAGINAL RECONSTRUCTION
A. Goals
1. Sufficient length of vaginal wall.
2. Adequate transverse dimension of introitus and pouch for intercourse.
B. Congenital absence
1. MRKH (Mayer–Rokitanski–Kuster–Hauser syndrome)
b. 1/4,000 to 1/80,000 live births
c. Maldevelopment of müllerian duct system (upper vagina, uterus, fallopian tubes).
d. Patients are 46XX with normal ovaries, rudimentary uterus, female external genitalia.
e. Often present with primary amenorrhea.
f. Vaginal atresia and absent cervix noted on examination.
g. Associated with rib and vertebral anomalies, 25% to 50% with renal duplications, agenesis, and ectopy.
h. Need intravenous pyelogram and renal ultrasound prior to surgical intervention.
i. Child bearing is possible with surrogate and in vitro fertilization.
j. Timing of procedure—14 to 20 years old, start with dilation.
k. Treatment options
i. Serial dilation: Motivated patients are successful, requires daily dilation either with manual dilators or with manufactured seats.
ii. Abbe–McIndoe technique
a) Blind pouch dissected between urethra and rectum, STSG harvested and placed over obturator.
b) Obturator removed at 7 days and dilation started at 14 days.
c) Majority of patients report satisfactory sexual relationships post-op.
d) PAP smears recommended in future to monitor for graft conversion to SCC.
iii. Sadove & Horton: FTSG into dissected blind pouch, advantage over STSG is that it may grow with patient if she is still young.
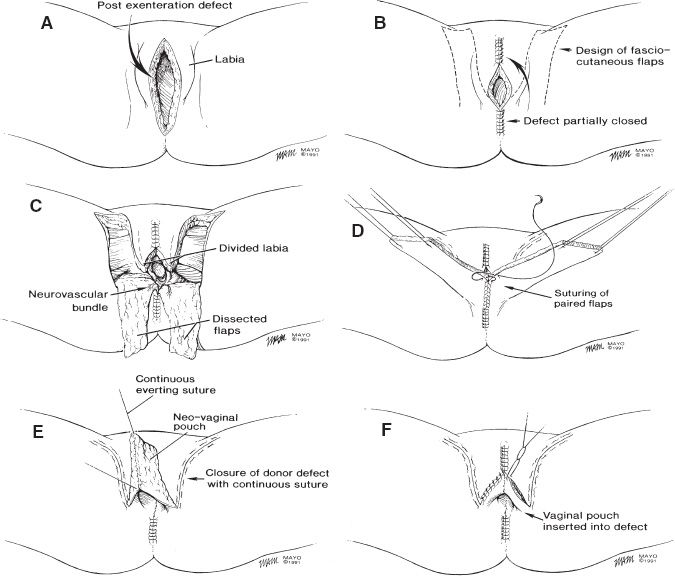
iv. Fasciocutaneous flaps (i.e., Singapore flaps)
a) Based on terminal branches of internal pudendal a. (posterior labial a.)
b) Hairless skin just lateral to labia is used, 15 cm × 6 cm may be harvested.
c) Sensate flap: Posterior labial branches of pudendal nerve and perineal branches of posterior cutaneous nerve of thigh.
d) Not typically performed as it alters external anatomy in young patients.
v. Colonic/small bowel interpositions: Salvage procedure, associated with persistent foul smelling secretions, requires laparotomy, friable mucosa bleeds with intercourse.
C. Acquired absence of the vulva
1. Most commonly secondary to resection of SCC or melanoma.
2. Rhomboid flaps and laterally based advancement flaps excellent options.
3. Skin grafts for large defects (FTSG from lower abdomen, closed primarily), require a bolster for 7 days. Post-op foley and constipating medications improve graft take.
4. Superficial external pudendal artery (SEPA) flap
a. More reliable anatomy than superficial inferior epigastric artery flap (SIEA) flap.
b. Small skin territory is OK for unilateral vulva reconstruction.
5. Gracilis myocutaneous V–Y advancement flap
D. Acquired absence of the vagina
1. Most commonly result of resection of urologic, gynecologic, and GI malignancies.
2. Prior radiation therapy is indication for flap at the time of resection.
3. Be cautious using abdominal-based flaps when patient has diverting ostomy.
4. Try to avoid circumferential incision at introitus—will stricture with time.
5. Flap options
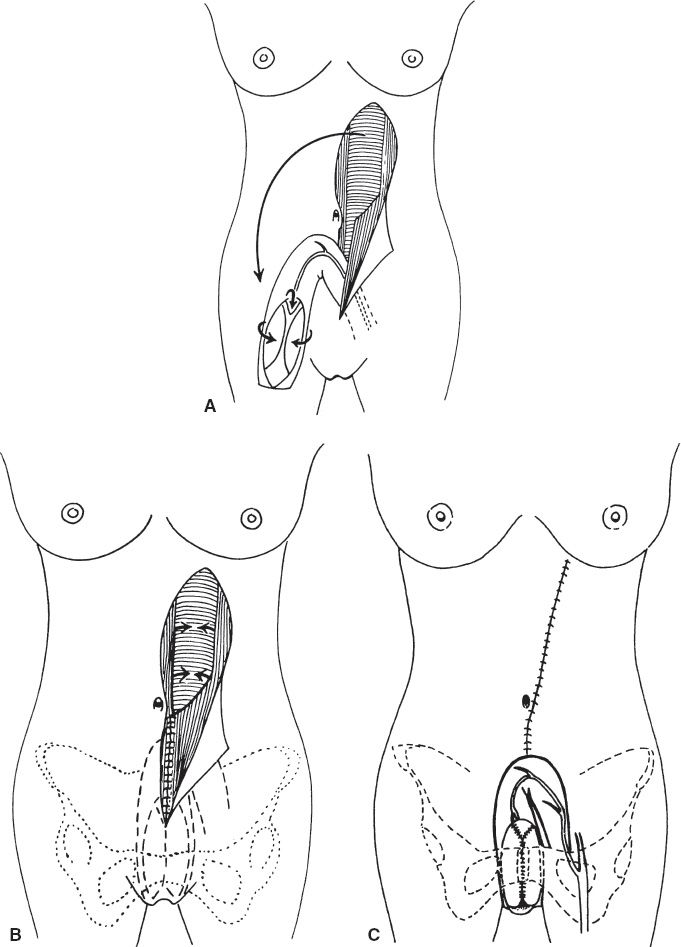
a. VRAM (Fig. 53-2)
i. Skin paddle can provide epidermis for perineum and posterior vaginal wall.
ii. Rolled VRAM can reconstruct circumferential vaginal defect and is the treatment of choice for total absence of the vagina.
iii. Based on deep inferior epigastric artery and vein.
b. Pedicled ALT
i. Excellent option with favorable donor site, best in thin patients.
ii. Based on descending branch of lateral femoral circumflex.
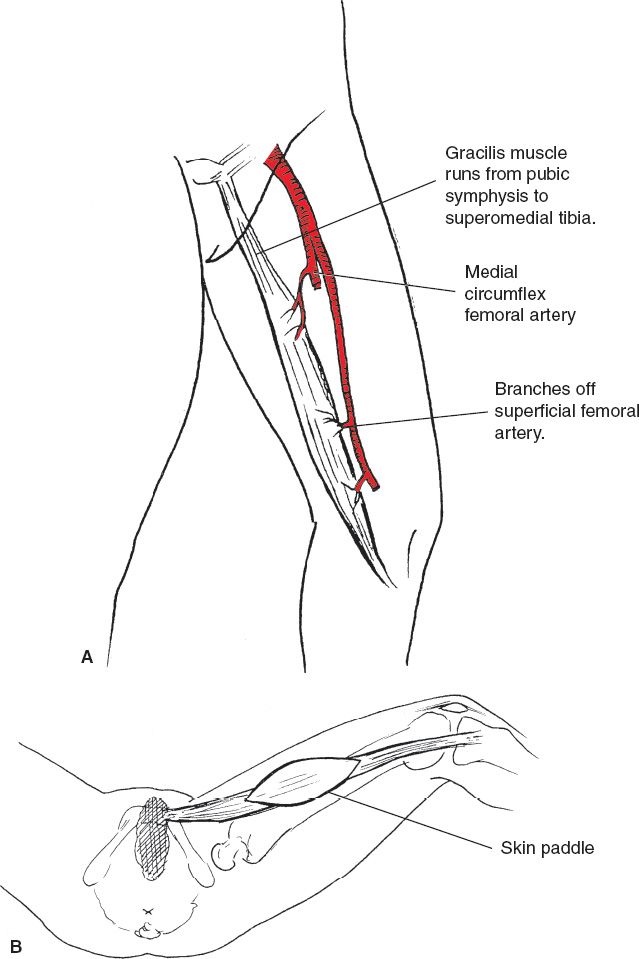
c. Bilateral gracilis flaps
i. Minimal donor site morbidity but with temperamental skin paddle, may require STSG.
ii. Based on medial circumflex femoral (Fig. 53-3).
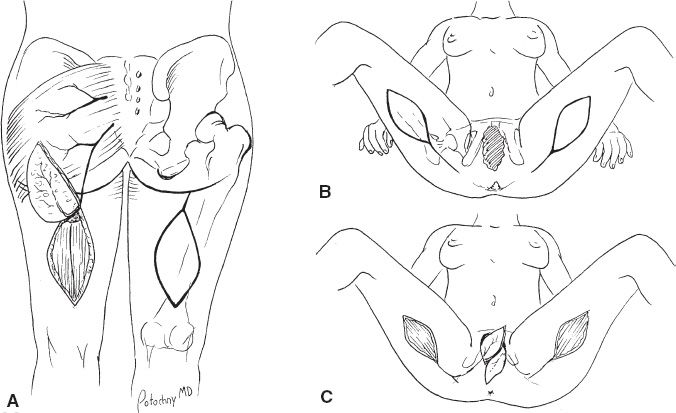
d. Posterior thigh flaps (Fig. 53-4): May have difficulty reaching vaginal defect.
e. Singapore (pudendal thigh) flaps (Fig. 53-5): May be difficult to contour if patient is previously radiated.
Figure 53-2. VRAM flap A: The flap is harvested from the abdomen and turned down into the pelvis on its pedicle. B: The abdominal fascia is repaired. C: The flap is inset at the recipient site. (From Fischer JF, ed. Mastery of Surgery. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012.)
VII. GENDER SURGERY
A. Patients must have formal diagnosis of Gender Identity Disorder (DSM-5 criteria).
B. Multidisciplinary approach is best to provide best comprehensive care for patients.
C. Very high incidence of depression, anxiety, addiction, suicidality, alienation from social support systems, homelessness, poverty in this patient population.
D. This is the one instance when the operative plastic surgeon is not competent to decide who is ready for surgery.
Figure 53-3. Gracilis flap. A: Vascular supply. B: Example of overlying skin paddle design. Innervation is from obturator nerve.
E. *Patients must meet WPATH criteria prior to OR
F. WPATH (World Professional Association of Transgender Health) requisites for surgery
1. 1 year of hormonal therapy.
2. 1 year of real-life experience.
3. Stable medical and mental health.
4. Two letters of readiness from qualified mental health professionals.
Figure 53-4. Posterior thigh flaps.
Figure 53-5. Singapore flaps (From Fischer JF, ed. Mastery of Surgery. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012.)
1. “Top” surgery
a. Chest reconstruction.
b. Limited liposuction and periareolar resection of glandular tissue is an option in small-breasted patients.
c. Larger breasts require mastectomies through IMF incision, contour liposuctioning, and free nipple grafts.
d. Post-op compression garment for 6 weeks important to maintain contour of chest.
2. “Bottom” surgery
a. Goals: Extend urethra, provide tactile protective sensation, plan to complete reconstruction in a single stage, aesthetically acceptable, limited donor site morbidity.
b. Metaidoioplasty
i. Penile substitution with clitoral enlargement and urethral transfer.
ii. Clitoris partially released from ventral chordae and advanced anteriorly by 3 cm.
iii. Urethra lengthened to end of clitoris.
iv. Labia majora are transposed posteriorly.
v. Caudally based, pedicled musculomucosal flap raised from anterior vaginal wall, must reach beyond tip of clitoris with width 3 cm, this will serve as lining of fixed perineal aspect of neourethra.
vi. Pros: Erogenous sensation maintained, shorter operation with no donor site.
vii. Cons: Suboptimal appearance and variable ability to urinate in standing position.
c. Phalloplasty
i. Pedicled options: Extended groin flap, tensor fascia lata flap, SIEA skin flap, rectus.
ii. Free tissue transfer options: Radial forearm flap, ulnar forearm flap, lateral upper arm flap, scapular, dorsalis pedis, fibula flap (pre-op tissue expansion).
iii. Current gold standard is the radial forearm free flap
a) Must perform and document normal Allen test, nondominant arm.
b) Significant donor site morbidity, slightly improved with Integra placement and delayed STSG to forearm.
c) China technique of “roll in a roll” to use skin of forearm to construct neourethra and outer phallus.
d) Create protective sensation by coapting lateral antebrachial cutaneous nerve to one dorsal clitoral nerve.
e) Second dorsal clitoral nerve left intact for erogenous sensation.
f) Inflatable hydrolic prosthesis for erectile function is possible, we do not perform these at our institution given risk of wound breakdown and extrusion.
iv. Recipient site is saphenous vein and femoral artery in groin or DIEA and SIEV in lower abdomen.
v. Norfolk technique of coronal ridge and sulcus construction to produce circumcised appearance—triangle flaps at distal end of neophallus create conic glans and sagitally slitted aspect of urethral orifice.
vi. Cons: High rates of urethral fistulae and strictures, morbid donor site.
vii. Pros: Adequate phallus length to urinate standing up.
H. Male to Female
1. “Top” surgery
a. Facial feminization: Endoscopic brow lift, rhinoplasty, tracheal shave, reduce supraorbital rim and glabella, and rhyditectomy.
b. Chest reconstruction
i. Hormonal therapy will produce modest breast development.
ii. Augmentation mammoplasty with submuscular silicone or saline implants.
a. Penile inversion vaginoplasty
i. Blunt dissection of perineal canal between prostate and rectum.
ii. Perineal triangular flap with apex on posterior scrotum creates the posterior vaginal vault lining.
iii. Orchiectomy performed, scrotal skin contoured into labia majora.
iv. Penile shaft is degloved, erectile bodies resected.
v. Glans penis pedicled graft based on dorsal artery, vein, and paired dorsal nerves is dissected from penile shaft and relocated to become neoclitoris.
vi. Penile shaft skin is inverted to form anterior and lateral vaginal walls.
vii. Urethra is shortened.
viii. Cons: High rates of vaginal and urethral structuring, delayed wound healing.
ix. Pros: Excellent aesthetic result, 1 stage operation.
PEARLS
1. In patients who require an ostomy be cautious about using VRAM flaps. Abdominal wall integrity is important to prevent parastomal hernias.
2. Beware of local tissue rearrangement or Singapore flaps to close a previously irradiated perineum. These tissues will have also been irradiated. The tissues may be difficult to move into defect and will have a high rate of delayed wound healing and breakdown.
3. Patients must meet WPATH criteria prior to Gender Reassignment Surgery.
4. Gender patients are best cared for in a multidisciplinary team setting with professionals that regularly treat these patients
QUESTIONS YOU WILL BE ASKED
1. What is the path of the pedicled ALT in perineum reconstruction?
The flap must be tunneled under the rectus femoris and sartorius muscles.
2. Where are your ALT flap perforators of the descending branch of lateral femoral circumflex artery?
Located within 3 cm of midpoint on axis from anterior superior iliac spine to lateral aspect of patella.
3. What is unique about the blood supply to the penis?
The glans and the shaft have separate blood supplies. The skin of the shaft is supplied by a dermal plexus while the dorsal artery supplies the glans. This allows these structures to remain viable after they are divided to create vaginal lining and neoclitoris in gender reassignment surgery.
4. Describe the layers of the penis.
See Figure 53-1.
THINGS TO DRAW
Draw cross section of the penis (Fig. 53-1).
Recommended Readings
Cordeiro PG, Pusic AL, Disa JJ. A classification system and reconstructive algorithm for acquired vaginal defects. Plast Reconstr Surg. 2002;110(4):1058–1065. PMID: 12198418.
Hollenbeck ST, Toranto JD, Taylor BJ, et al. Perineal and lower extremity reconstruction. Plast Reconstr Surg. 2011;128(5):551e–563e. PMID: 22030517.
Monstrey S, Hoebeke P, Selvaggi G, et al. Penile reconstruction: is the radial forearm flap really the standard technique? Plast Reconstr Surg. 2009;124(2):510–518. PMID: 19644267.
Wong S, Garvey P, Skibber J, Yu P. Reconstruction of pelvic exenteration defects with anterolateral thigh-vastus lateralis muscle flaps. Plast Reconstr Surg. 2009;124(4):1177–1185. PMID: 19935301.
< div class='tao-gold-member'>