Pediatric Orbital Fractures
James Y. Liau
DEFINITION
Fractures of the inferior and/or medial orbital wall
ANATOMY
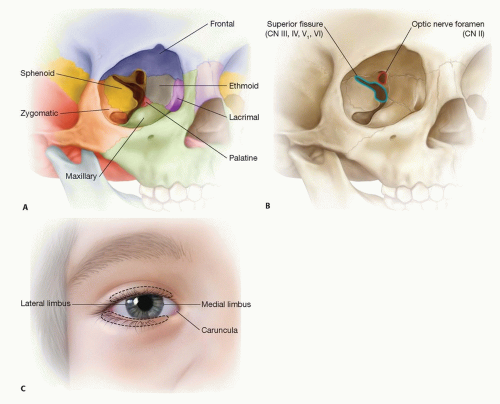
The orbit consists of seven bones; however, the ones that are involved are invariably the maxilla and ethmoid bones. Operative repair focuses on re-establishing the appropriate volume of these components (FIG 1A).
Other pertinent anatomy includes optic nerve and superior fissure, which contains CN III to CN VI. These structures are located in the superior medial aspect of the orbit (FIG 1B).
Soft tissue anatomy is relevant. This includes the palpebral fissure, gray lash line, septum, canthus, and caruncula (FIG 1C).
Usually, orbital growth is complete by 6 to 8 years of age.
PATHOGENESIS
Inferior orbital floor fractures occur with facial trauma, which entails a blow to the globe resulting in increased orbital pressure. This pressure fractures the thinner maxillary portion of the orbital floor causing a blow-out fracture into the maxillary sinus.
NATURAL HISTORY
Diplopia that is self-limiting
Enophthalmos can occur if the orbital volume is not corrected with floor reconstruction or soft tissue volume atrophy from trauma.
Entrapment results in muscle fibrosis and permanently impaired conjugate gaze.1
PATIENT HISTORY AND PHYSICAL FINDINGS
Because of immediate post-traumatic swelling, enophthalmos is usually not appreciated clinically until swelling has decreased, unless the orbital blow-out fracture is quite large. Then enophthalmos and dystopia may be immediately appreciated.
With blow-out fractures, extraocular movements are usually decreased due to the trauma and swelling, but there is usually some degree of movement.
With entrapment, there is no voluntary extraocular movement due to pain. Attempted upward gaze will result in intense pain, and nausea; bradycardia can also occur.
IMAGING
CT scan is the modality of choice. All three views are essential.
Axial views elucidate whether there is medial wall involvement, and the size.
Coronal views elucidate the width of floor fracture, medial wall, inferior rectus muscle involvement, and inferior orbital nerve involvement.
Sagittal views elucidate the length of the floor fracture and inferior rectus muscle involvement and helps delineate the depth of the dissection before encountering the posterior shelf.
DIFFERENTIAL DIAGNOSIS
Need to diagnose other concomitant facial fractures. Most commonly involved are
Medial wall
Zygomatic maxillary complex
Le Fort 2
Le Fort 3
NONOPERATIVE MANAGEMENT
Conservative treatment runs a higher risk of enophthalmos depending on the size of fracture. Amblyopia in pediatric population is generally self-limiting due to the adaptable plasticity of the brain.
SURGICAL MANAGEMENT
Preoperative Planning
Performing CT scan of axial, coronal, and sagittal planes will help clarify anatomy such as orbital content or inferior rectus entrapment (FIG 2).
Forced duction test under anesthesia if concerned about entrapment. This is difficult to do in an awake patient due to pain despite topical anesthetic drops. I usually defer to CT scan and clinical physical examination of pain and nausea with or without bradycardia upon upward gaze.
Types of Implants
Synthetic
Polyethylene
Pros: No donor site and easily cut to size
Cons: Does not “grow” with the child, extrusion if not secured adequately, can become infected, and does not have rigidity for adequate support required in extensive orbital floor fracture
Titanium
Pros: Easily obtainable, retains shape, and easily cut to size, excellent rigidity required for extensive orbital fractures
Cons: Does not grow with child, extrusion if not secured adequately, concerns of soft tissue tethering into the openings of the implant1,2
Mixed
Pros: Easily obtainable and has both rigidity and minimal risk of tethering at implant/soft tissue interface
Cons: Does not grow with child; risk of extrusion if not secured adequately
Autologous
Bone
Pros: Autologous; can be easily shaped
Cons: Donor-site morbidity; requires time for harvest
Cartilage
Pros: Autologous; can be easily shaped
Cons: Donor-site morbidity; requires time for harvest
Positioning
Need to be able to stand at head of bed allowing 270-degree access to the head. Usually turning the bed 90 degrees or 180 degrees provides this access (FIG 3A).
Shoulder roll extending the head to give better visualization of the orbital floor (FIG 3B,C).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree