58. Brachioplasty
Indications
Excess skin and/or subcutaneous tissue of the arm refractory to conservative treatment such as diet and exercise
Contraindications
Absolute
Neurological or vascular disorders of the upper extremity
Collagen-vascular disorders (Ehlers-Danlos syndrome, progeria, elastoderma)
Lymphedema of the arms
Unrealistic patient expectations
Relative
Severe comorbid conditions (including heart disease, thromboembolic disease, diabetes)
Unstable weight gain or loss
Expecting future pregnancy
Active smoker
Patients with a history of keloids or hypertrophic scars
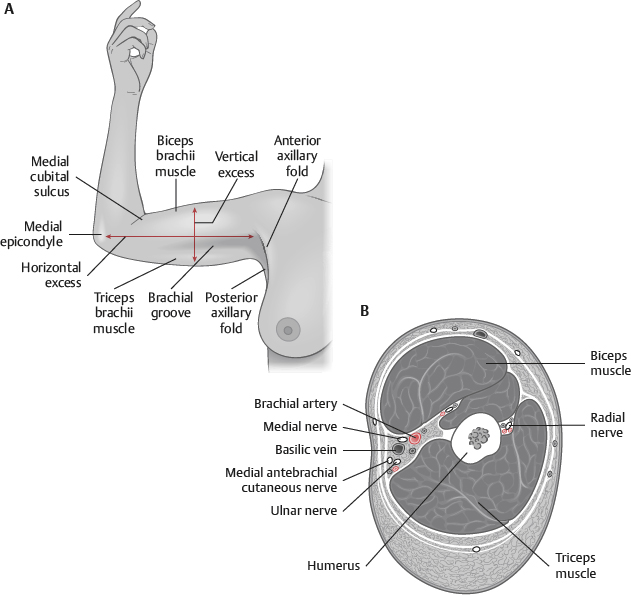
Anatomy
Skin: The skin covering the shoulder and arm is smooth and very mobile over the underlying structures.
It is thin on medial aspect and progressively thicker laterally.
Subcutaneous tissue: Fat accumulates on the inferoposterior aspect of the arm, with a minimal amount medially.
Superficial fascia: The superficial fascia both circumferentially and longitudinally encases the fat of the arm from the axilla to the elbow.
This fascia weakens with age and weight gain, causing ptosis of the posteromedial arm.
Deep fascia: The deep fascia invests all muscles and important neurovascular structures.
This layer should never be violated during brachioplasty or suction-assisted lipectomy.
Tip:
Along the distal third of the arm and in the region of the medial elbow, the basilic vein and medial antebrachial cutaneous nerve run together and are superficial to the deep fascia and vulnerable to injury, especially where they pierce the deep fascia an average of 14 cm proximal to the medial epicondyle. 1
Tip:
The only nerves found superficial to the deep investing fascia are branches of the medial brachial cutaneous nerve and the intercostobrachial nerve. All other important neurovascular structures are deep to the investing fascia
Preoperative Evaluation
Obtain a complete medical history, paying specific attention to weight gain/loss, weight stability, tobacco use, and scarring.
Physical examination should focus on the amount of excess skin, excess subcutaneous tissue, and degree of ptosis present in the arm.
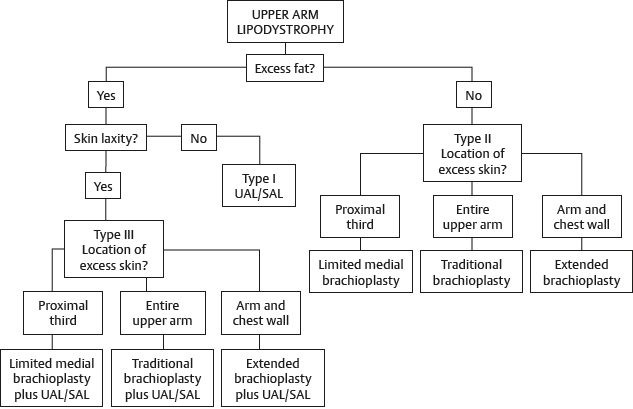
Patients can then be stratified into one of three groups (Table 58-1).
An algorithm (Fig. 58-2) can then be used to help guide surgeons to the procedure that is best suited to achieve optimal results. 2
Tip:
Weight should be stable for 6-12 months before performing any body contouring procedure on a massive-weight-loss patient
Skin Excess | Fat Excess | Location of Skin Excess | |
I | Minimal | Moderate | n/a |
IIA | Moderate | Minimal | Proximal |
IIB | Moderate | Minimal | Entire arm |
IIC | Moderate | Minimal | Arm and chest |
IIIA | Moderate | Moderate | Proximal |
IIIB | Moderate | Moderate | Entire arm |
IIIC | Moderate | Moderate | Arm and chest |
Informed Consent
Patients need to be informed that, with a brachioplasty, they are trading a more pleasing shape and contour of the arm for a scar.
The scar is not inconsequential and will be visible depending on the type of clothing worn.
Scars may stay thick and heavy for a prolonged period of time.
The brachioplasty scar is likely the most noticeable scar in all of aesthetic surgery.
Senior Author Tip:
In the preoperative consult, use a skin marker to draw the potential scar on the patient’s arms to help them understand the procedure and to align their expectations with reality. Document this in their medical record
Tip:
Photographs are imperative when discussing brachioplasty outcomes
Common brachioplasty complications include widened hypertrophic scar, wound dehiscence, seroma, infection, paresthesias/numbness, scar tethering across the axilla, and recurrent skin laxity.
Equipment
No special equipment is needed to perform a brachioplasty unless concomitant liposuction is performed.
In this case, wetting solution and liposuction equipment are required.
Technique
Markings
An area of debate for surgeons performing brachioplasty is where to place the arm scar.
Many place the scar within the brachial groove, whereas others prefer a posteriorly positioned scar.
A survey of plastic surgeons and the general public showed that a medial, straight brachioplasty scar is more acceptable than a posterior straight scar. 3
Brachioplasty markings depend on the type of brachioplasty performed.
The type of brachioplasty performed depends on the location of the excess skin (see Table 58-1).
Type I: Minimal skin excess, moderate fat excess
If skin tone is good, this is best treated with suction-assisted lipectomy alone.
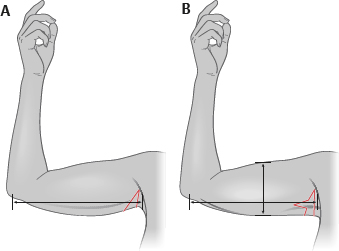
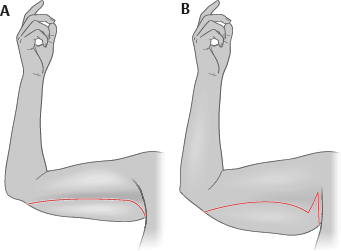
Type IIA: Moderate proximal skin excess, minimal fat excess
A minibrachioplasty 4 is used, which is isolated to the axillary fold.
If the skin excess is purely horizontal, then a vertically oriented wedge or ellipse is placed in the axillary fold (Fig. 58-3, A).
If skin excess is horizontal and vertical, a T-shaped excision is used (Fig. 58-3, B).
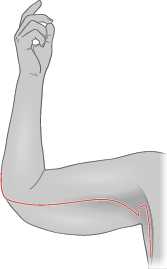
Type IIB: Moderate skin excess of the entire arm (axilla to elbow), minimal fat excess
A traditional brachioplasty is used placing the scar in the brachial groove.
If there is vertical skin excess only, then use a linear horizontal incision (Fig. 58-4, A).
If there is vertical and horizontal skin excess, add an L-shaped extension to the linear horizontal incision in the axilla (Fig. 58-4, B).
Type IIC: Moderate skin excess of the arm and chest, minimal fat excess
An extended brachioplasty is needed, which extends the excision onto the chest wall.
These are typically massive-weight-loss patients.
A horizontal incision is made in the brachial groove and carried through the axilla down onto the chest wall.
This excision often passes distal to the elbow (Fig. 58-5).
Type IIIA: Moderate proximal skin excess, moderate fat excess
Type IIIB: Moderate skin excess of the entire arm, moderate fat excess
Type IIIC: Moderate skin excess of the arm and chest, moderate fat excess
In these cases (type III), fat excess is moderate and skin excess is moderate.
Options for treatment include further weight loss before surgery, staged liposuction followed by skin resection, or concomitant liposuction and brachioplasty.
Skin-resection brachioplasty patterns are the same as for type II subtypes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree