4 Functional and Aesthetic Genital Surgery in the Female
4.1 Fundamentals
4.1.1 Anatomy
The external female genitals include the following structures:
Mons pubis.
Labia majora and labia minora.
Vaginal vestibule.
Vestibular erectile tissue.
Clitoris.
Vestibular glands.
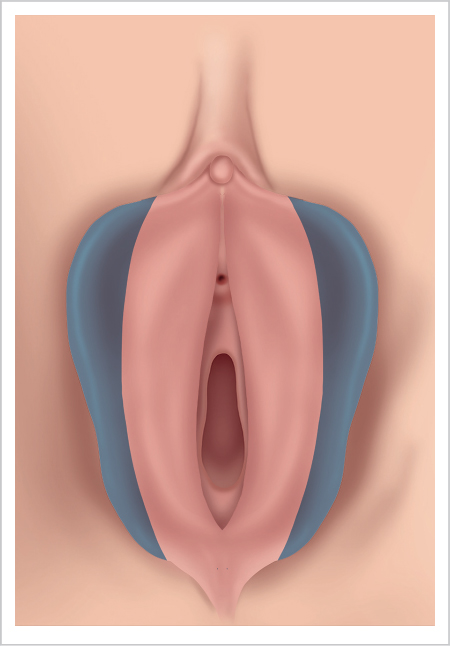
The labia majora are hair-covered folds of soft tissue extending from the mons pubis to the perineum. The pudendal cleft lies between the anterior commissure and posterior commissure. The projection of this cleft, together with the labia minora, covers the clitoris, urethral meatus, and vaginal introitus.
The labia minora are paired skin folds that lie adjacent to the medial aspects of the labia majora. They form the lateral demarcations of the vaginal vestibule and introitus. They are hairless and are covered on the outside by a stratified keratinized squamous epithelium and on the inside by a nonkeratinized squamous epithelium with numerous sebaceous glands. The pigmentation is more pronounced on the outside than on the inside. The labia minora diverge anteriorly into two folds each. The two outer folds together form the prepuce of the clitoris that surrounds the glans of the clitoris and joins the anterior commissure of the labia. The two inner folds merge to form the frenulum of the clitoris. Posteriorly, the two labia minora join the labia majora at the posterior commissure or fourchette.
The orifices of the paired greater vestibular or Bartholin glands are located on the inner surface of the labia minora. Together with the lesser vestibular glands they produce a secretion that lubricates the vaginal vestibule. The hymen separates the external and internal female genitals.
The posterior genital region receives its blood supply from the posterior labial branches of the perineal artery arising from the internal pudendal artery. The anterior genital region is supplied by branches of the femoral artery (anterior labial branch arising from the external pudendal artery). Venous drainage follows an analogous pattern via the internal pudendal vein, several external pudendal veins, and the vesicular venous plexus.
4.1.2 Physiologic Norms
The outward appearance of the vulva changes over the course of a woman’s life. The first significant changes occur during puberty, and secondary sex characteristics develop during this period. Marshall and Tanner 22 divide the development of the outward appearance of the genital region during puberty into five phases (▶Fig. 4.1):
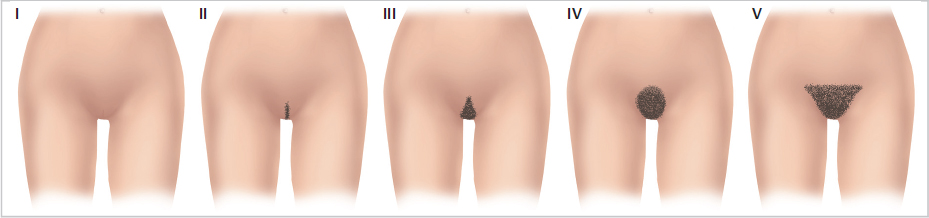
Phase I is characterized by complete absence of pubic hair.
In phase II sparse hair appears along the midline on the labia majora and mons pubis.
In phase III hair coverage increases. Hair now covers the labia majora and also spreads laterally on the mons pubis.
In phase IV hair coverage continues to spread to the upper outer corners until it forms a triangle.
In phase V, the final phase, a complete triangle of hair coverage is exhibited.
Phase V is characterized by a pattern of hair coverage with its horizontal border just superior to the end of the genitofemoral sulcus in the groin. Lateral to the labia majora, hair coverage can extend onto the thighs.
In a sexually mature woman, pregnancies and births result in other changes due to changes in perfusion, stretching of connective tissue, or birth trauma. In postmenopausal women, the fatty cushions of the labia majora atrophy. The elasticity of the skin decreases, and the thickness and coloration of the pubic hair decreases. The genital region is more exposed and changes to it are more readily apparent.
Many factors influence the outward appearance of the vulva, and the broad range of variation in the color and shape of the external genitals between individuals renders it difficult to define physiologic norms. For example, Lloyd et al 19 describe lengths of the labia minora ranging from 2.0 to 10.0 cm based on measurements obtained in 50 premenopausal women. The width of the labia minora was equally variable, ranging from 0.7 to 5.0 cm, with an average width of 2.1 cm.
The present data can only provide general orientation for an initial estimation of findings. Findings should always be assessed individually and should be evaluated for hormonal or chromosomal disorders (▶Fig. 4.2, ▶Table 4.1).
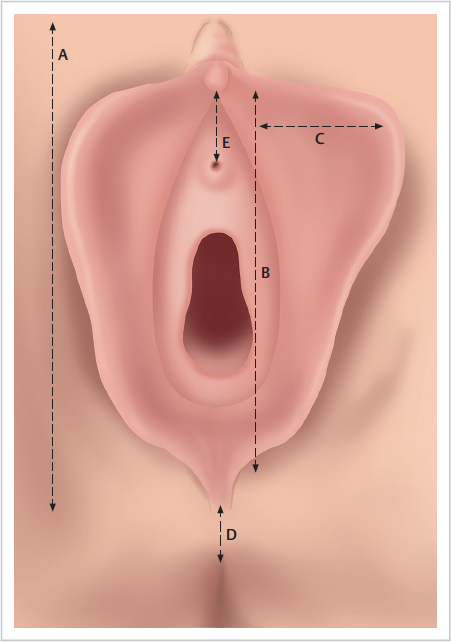
Classification | External genitals | Measured values |
A | Length of labia majora | 9.3 ± 1.3 cm |
B | Length of labia minora | 6.0 ± 1.7 cm |
C | Width of labia minora | 2.1 ± 0.9 cm |
D | Length of perineum | 3.1 ± 0.8 cm |
E | Distance of clitoris to urethra | 2.8 ± 0.7 cm |
According to Basaran et al, except for an atrophic decrease in the width of the labia minora, significant changes do not occur in postmenopausal women.
4.1.3 History and Preoperative Preparations
The desire for corrections to the external genitals is becoming increasingly common. Although aesthetic considerations remain the primary motivation, functional impairments may also be a reason for women to undergo surgical correction. Considerations include congenital, hormonal, age-related, and postpartum changes, yet can also include changes due to trauma, tumor resection, or previous surgery. Both patients with functional complaints as well as those seeking treatment for purely aesthetic reasons are questioned in detail about their motives for undergoing genital surgery.
Note
Patients’ expectations and the possible results must be discussed in detail prior to surgery.
After obtaining a patient’s general and gynecologic history, it is recommended to obtain a sexual medical history. This will provide information about the symptoms, the degree of suffering, the influence of the partnership, and the motivation for seeking treatment. The female sexual function index (FSFI) questionnaire is a suitable additional means of identifying sexual impairments.
The physician and the patient must ascertain in a constructive dialog whether a possible intervention will be able to solve these problems identified during examination. As a high proportion of patients may be expected to have a slightly to moderately impaired body image, it is essential to exercise care in determining whether surgery is indicated. Slight surgical corrections can be made to improve body image. It is advisable to have the patient follow the examination with a hand-held mirror. Patient education regarding surgical techniques and risks is provided. It also needs to be pointed out that sufficient scientific data are not yet available as to whether these interventions lead to lasting emotional or functional improvements. Additionally, the patient is informed that studies utilizing the FSFI questionnaire have failed to demonstrate any general improvements with respect to sexual function and how sex is experienced following genital surgery.
4.2 Labiaplasty
4.2.1 Labia Majora
Hypertrophy of the Labia Majora
The size and shape of the labia majora are decisively influenced by their cushion of fatty tissue. Minor asymmetry is physiologic. Hypertrophy due to severe obesity or in conjunction with lipodystrophy must be differentiated from genital edema, which can occur in conjunction with lymphedema or Crohn’s disease. Hypertrophy of the labia majora can also develop where there is a decrease in the cushion of fatty tissue secondary to massive weight loss. Here, the hypertrophy results from residual lipomatosis in the excess skin. This can also take the form of visible asymmetry.
Etiology
Simple increases and decreases in the volume of fatty tissue are usually associated with massive fluctuations in body weight. Hypertrophy, in which excess skin left from the atrophy of fatty tissue causes functional or aesthetic impairments, occurs more often with increasing age. It also occurs secondary to surgical interventions (lymphedema).
Surgical Techniques
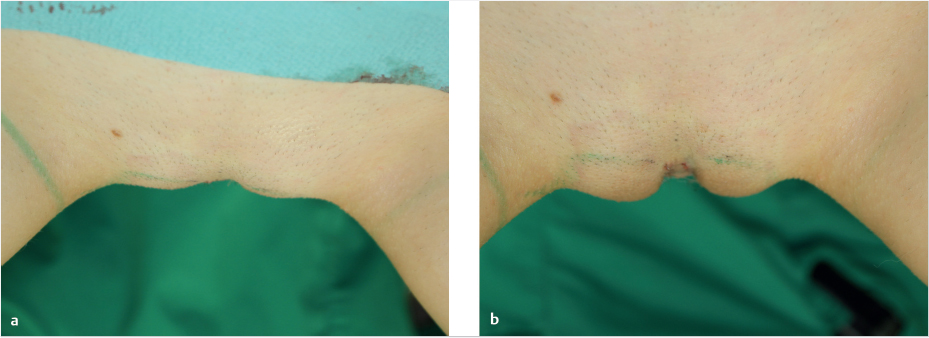
Slight asymmetry and moderate excesses of fatty tissue in the labia majora can be successfully treated by liposuction, especially in persons of normal weight with elastic skin. After instilling a tumescent solution, the surgeon removes the excess fatty tissue with suction through one or two stab incisions and contours the labia.
If liposuction leaves behind a severe excess of skin or if there is too much fatty tissue to remove by suction, then one must consider dermolipectomy. The borders of such a tissue resection are demarcated medially by the hairline or the fold at the junction with the labia minora. The lateral demarcation is approximately 1 cm medial to the genitofemoral sulcus. The excision can be continued anteriorly and posteriorly to include the entire extent of the labia majora.
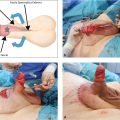
The extent of the tissue to be resected is marked on the standing patient preoperatively. With the patient in the lithotomy position with the legs abducted, the surgeon controls whether it would be possible to close the wound without tension and without obliterating the labia minora. If the tension is too great, the width of the resection must be reduced. Instilling 50 to 100 mL of a tumescent solution (with epinephrine) on each side is also recommended preoperatively. This will reduce the risk of bleeding complications. The actual skin resection (in the form of a spindle or sickle and tacking along the subcutaneous fatty tissue) is performed depending on the findings. The resection is made so that the closing suture line runs parallel to the genitofemoral sulcus. The dissection should not extend any deeper than the general body fascia (▶Fig. 4.3, ▶Fig. 4.4a–d, ▶Fig. 4.5a–c).


Atrophy of the Labia Majora
Autologous fat grafts (lipofilling) can be used effectively to treat congenital or acquired asymmetry of the labia majora, age-related atrophy, and labia majora defects too small to warrant flap reconstruction. Fatty tissue obtained by liposuction from the medial thighs or abdomen is processed as specifically required and then injected subcutaneously through small stab incisions in the anterior labia majora.
Caution
Make sure that the injection remains strictly subcutaneous and does not deviate into the blood vessel containing deeper layers.
Regular follow-up examinations are performed even after the swelling subsides because a possible loss of volume may necessitate repeating the procedure. Alternatives to autologous fat grafts include many synthetic filler substances (such as hyaluronic acid preparations) of varying degrees of cohesiveness. These, too, must be applied using a strictly subcutaneous technique. Even with these substances, a volume loss due to absorption may be observed after 6 to 12 months, which may necessitate a second procedure (▶Fig. 4.6, ▶Fig. 4.7, ▶Fig. 4.8).

4.2.2 Labia Minora
Hypertrophy of the Labia Minora
The appearance of the labia minora can vary greatly. Asymmetry and labia widths ranging from 0.7 to 5.0 cm may be regarded as physiologically normal. Yet functional symptoms and aesthetic limitations can occur not only beyond this range but within it. Such problems can be sufficient cause for the patient to opt for a corrective intervention.
Many patients regard the size and position of the labia minora relative to the labia majora as decisive. Queried about their aesthetic ideal, 97.8% (n = 550) of the patients surveyed in a study by Miklos et al 24 responded that they would prefer labia minora whose edges lie below or flush with the level of the labia majora. Defined in these terms, clinically relevant hypertrophy may be present as soon as the labia minora project beyond the level of the labia majora.
Women with hypertrophic or asymmetrical labia minora often describe discomfort and impairments in sports, when wearing certain clothing, when urinating, or during sexual intercourse (dyspareunia). This latter case may involve impaired sexual sensation or be caused by introversion (invagination) of projecting tissue. Microinjuries to the enlarged labia minora can lead to a strong burning sensation that persists for days. Patients often report chronic local inflammation and problems with feminine hygiene.
Note
Affected patients often suffer intensely from an aesthetic impairment, making it crucial for the surgeon to obtain a comprehensive patient history.
Etiology
Hypertrophy of the labia minora can be due to the following causes:
Idiopathic.
Congenital.
Medically induced (such as from androgens, estrogens).
In connection with a myelodysplasia syndrome.
As a vulvar lymphedema.
Due to dermatitis.
Postpartum or secondary to birth trauma.
Secondary to tumor surgery.
Posttraumatic.
In a postbariatric patient (usually relative hypertrophy due to volume loss in the labia majora).
Age related (due to loss of skin elasticity and fat deposits in the mons pubis).
Due to volume loss in the labia majora (relative hypertrophy).
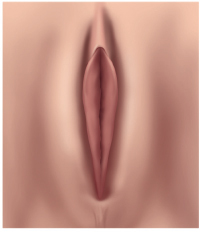
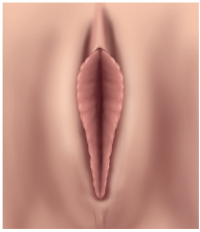
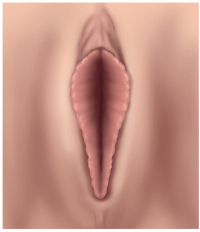
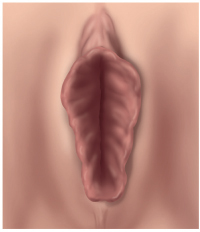
Classifications
The classification systems that have commonly been used to date essentially focus on the size of the labia minora. The classification described by Franco 10 (▶Table 4.2) uses only the width of the labia minora (the distance from the base of the labia to the edge of the labia) without any clinical context. The classification described by Chang et al 3 (▶Table 4.3) is more extensive and includes the relation of the labia minora to the labia majora and to the anterior commissure (prepuce of the clitoris) and posterior commissure.
Type | Labial width in cm |
1 | < 2 |
2 | 2–4 |
3 | 4–6 |
4 | > 6 |
However, clinical practice has shown that the size of the labia minora is only of secondary importance to the subsequent result of therapy. A clinical classification based on the nature of the clitoral hood and the distance between the tip of the clitoris and the urethral meatus would appear to be more useful (▶Table 4.4).
Choice of Surgical Technique
Labioplasty was first described as a linear resection of the margin of the labium. This has been followed by numerous descriptions of various surgical techniques. The shared element of these techniques is their exclusive suitability for treating isolated hypertrophy of the labia minora. For a long time, coexisting hypertrophy of the clitoral hood was not taken into consideration. None of these techniques can be used to sufficiently correct it. The classifications according to Franco et al 10 and Chang et al 3 show that until recently little thought was given to regarding the labia minora and the clitoral hood as an integral aesthetic whole despite the importance for the postoperative result.
In contrast, the clinical classification (▶Table 4.4) considers the labia minora and the clitoral hood as an aesthetic whole that forms the basis for deriving an algorithm and a therapy recommendation. The three types of hypertrophy of the labia minora outlined in the classification and therapy scheme are assigned to three, from the many techniques previously described in the literature, proven surgical principles. 35 , 36 , 37 , 38 , 39 ,40,41,42,43
According to this algorithm, the choice of surgical procedure is based first and foremost on observation of the clitoral hood. If it does not exhibit a surplus of skin (type 1), then an isolated reduction of the labia minora will suffice. However, if it does exhibit a surplus of skin, then the distance between the tip of the clitoris and the urethra should be taken into consideration. If this distance is relatively short (≤ 1.5 cm) (type 2), then no correction will be necessary. However, the lateral prepuce will be slightly narrowed. Yet in most cases hypertrophy of the prepuce is present as well, with a distance of 2 to 5 cm (type 3) between the tip of the clitoris and the urethra. Here a technique is applied which can simultaneously be used to correct protrusion of the clitoris. Thus, from a large number of surgical techniques, some of which already have a long history, three surgical techniques have been proven effective with which the desired results can be achieved in nearly every case.
In rare cases the prepuce is greatly enlarged vertically yet the distance between the tip of the clitoris and the urethra is too short for correction. In such a situation, the prepuce is shortened (see Chapter 4.3, Clitoral Hood Reduction).
Principles of Labiaplasty
Most patients who opt for a labia correction have simultaneous hypertrophy of the labia minora and the clitoral hood (class III according to Chang et al and type 2 according to von Lukowicz). Regardless of the surgical technique, it must be ensured that the neurovascular supply to the labia minora and the covering of the vaginal introitus and urethral meatus remains intact postoperatively, even after wound healing is complete.
For this reason the width of the labia minora after resection should be at least 0.8 to 1 cm. Additionally, to avoid scarring with adhesions, the posterior commissure (fourchette) should only be included in the resection in class IV hypertrophy according to Chang et al. 3
The tissue resection itself can be performed with a scalpel, monopolar electrocautery needle (high-frequency surgery), or by means of Nd:YAG laser (10 W). The electrocautery needle and Nd:YAG laser have the advantage of less blood loss compared to resection with a scalpel. An additional advantage of these techniques is that the incisions can be made with greater precision. USP 5–0 or 6–0 absorbable monofilament suture is recommended for the skin suture. A running suture is preferable to interrupted sutures because it is less likely to cause compression necrosis and it avoids the typical serrated appearance of the edges of the labia.
Preoperative Marking
The variation in the shape and size of the labia minora dictates a corresponding variation in the amount and shape of tissue to be resected. With all interventions, it is best to perform all preoperative marking before injecting the local anesthetic. To do this, the labia are first stretched out medially. The fold between the labium minus and the labium majus provides a landmark. The medial incision line is marked starting at this point. The medial and lateral marking lines should be superimposed because otherwise the alignment of the labium can change. Anatomic forceps can be used to facilitate transferring the marking from lateral to medial; one arm is placed on the outside of the labium and the other arm on the inside at the same level. By changing the direction of pull and then stretching the labium anteriorly, posteriorly, and medially, the surgeon can evaluate the level of the incision line and the symmetry and can draw any additional lines necessary. After application of local anesthesia, the labia are grasped with surgical forceps to facilitate handling during the procedure.
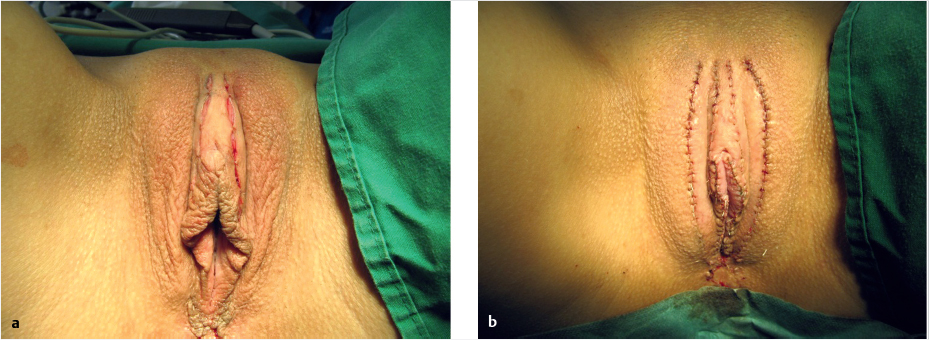
Anesthesia
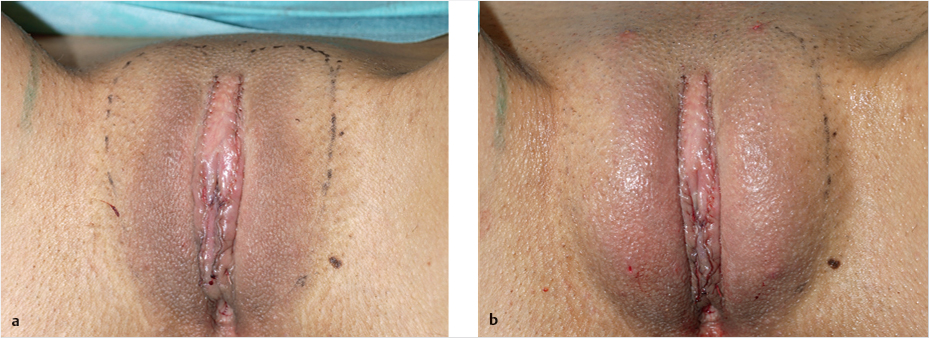
Labioplasty can be performed under local anesthesia in almost all cases. Prior topical anesthesia with an ointment containing a local anesthetic significantly reduces the pain from the injection of the local anesthetic. After disinfection with an antiseptic and precise marking of the incision line, the site is infiltrated with an anesthetic such as xylocaine 2% with epinephrine 1:100,000. A nerve block is not used; field block anesthesia is used instead to locally create a nearly bloodless field (▶Fig. 4.9a, b).

Surgical Techniques
Treatment of Labia Minora Hypertrophy (Chang Class II/von Lukowicz Type 1)
Linear Resection
▶Indication. Technique of first choice for Chang class II/von Lukowicz type 1 hypertrophy, defined as isolated hypertrophy of the labia minora without excess tissue in the region of the prepuce.
▶Advantages. Simple procedure with minimal complications.
▶Disadvantages. Suitable exclusively for isolated hypertrophy of the labia minora. Not suitable for excess tissue in the prepuce. Cannot alter the length of the labia. Long exposed wound edge. Possible loss of physiologic contour and color. Result may appear unnatural due to scarring or pigmentation problems at the edges of the resection. Hypersensitivity or hyposensitivity of the labia in the region of the frenulum.
▶Principle. This technique is used for contouring. By removing the usually dark pigmented and irregular outer edges of the labia, it achieves more uniform shape and a lighter color.
▶Procedure. The markings are drawn laterally and medially, maintaining a minimum distance to the fold of 1 to 1.5 cm. After spreading and stretching the labia, a slightly curved or S-shaped incision is made to produce a postoperative labial width of approximately 1 to 2 cm. The incision begins at the level of the clitoris on the lateral end of the prepuce in the labia minora and courses posteriorly along the inside or outside, respectively. The resection of the excess tissue spares the posterior commissure. After the excess tissue is removed, the wound is closed first with some single buried sutures with an USP 4-0 or 5-0 absorbable braided suture material to close the dermis and subcutaneous tissue. The edges of the wound can be optimally adapted by using a running subcuticular (intracutaneous) suture with USP 5-0 absorbable monofilament suture material monofilament suture (▶Fig. 4.10, ▶Fig. 4.11a–d).

Caution
Care should be taken to ensure that the wound edges fit well, especially in the region of the prepuce. If this technique is used despite the presence of hypertrophy of the clitoral hood, the postoperative result is an unnatural appearance with the hypertrophic prepuce imitating a micropenis.
Wedge Resection
An alternative to the linear resection is a wedge resection. However, clinical studies have shown that the rate of postoperative complications is lowest with the linear resection. Nonetheless, in certain selected cases, good results can also be achieved with a wedge resection.
▶Indication. Chang class II / von Lukowicz type 1 hypertrophy.
▶Principle. The wedge resection method spares the outer margin and its neurovascular supply while allowing alteration of the length and width of the labia.
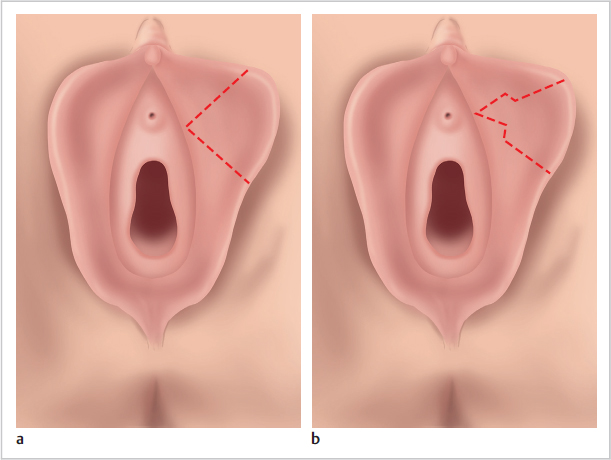
▶Procedure. The central wedge resection is a suitable treatment when isolated labial hypertrophy occurs in the middle third around the vaginal introitus, as is usually the case. The external urethral meatus provides a landmark for the tip of the V-shaped resection figure. A risk of excessive tension on the scar or the vaginal introitus can be addressed by modifying the technique to include an interposed 90-degree Z-plasty. This is done by replacing the two linear incisions of the V-shaped resection figure with one Z-shaped incision line each in the opposite direction (▶Fig. 4.12a, b).
▶Advantages. The natural margin and pigmentation are preserved, and the scar is barely visible. Labial length is readily correctable with the opportunity to resect tissue without creating a scar along the margin of the labium.
▶Disadvantages and Complications. Only moderate alterations of labial width are possible. Sensitivity is lost in the anterior labia minora. The correction produces a high-contrast pigment transition between the anterior and posterior portions of the labia. The vaginal introitus is narrowed. Flap necrosis can occur due to impaired postoperative perfusion. Postoperative problems when sitting can persist for about 2 weeks. Scarring can cause pain during intercourse.
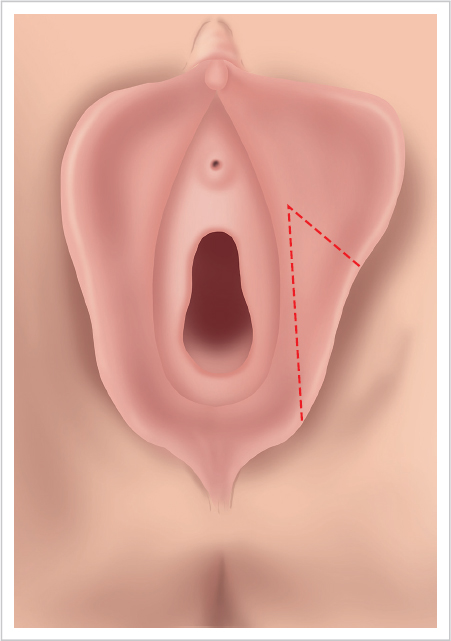
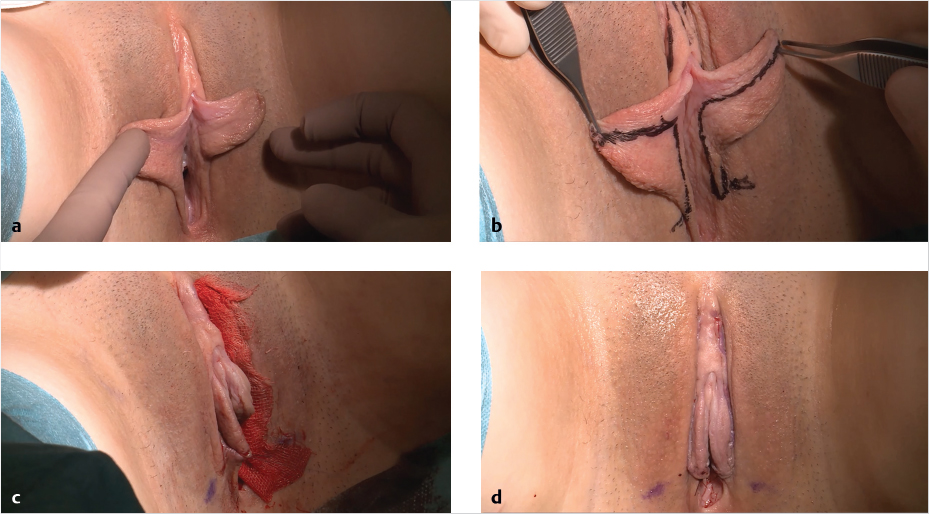
Posterior Wedge Resection
The posterior wedge resection is recommended where the excess tissue occurs in the posterior third or where a greater lift effect in the labial margin is desired.
However, this technique is particularly suitable if the posterior third of the labia is not well developed and the excess tissue is located primarily in the anterior and middle thirds. In that case, after the posterior wedge resection, a wound bed can be created in the posterior portion and the tissue fixated in this region, thus forming a labium of uniform width over its entire course. Beginning at the posterior commissure on the inside of the labium, a resection line is marked at a distance of about 1 cm parallel to the base of the labium as far as the region between the urethral meatus and the vaginal introitus. From here, the line is continued toward the labial margin at an angle of up to 90 degrees depending on the planned amount of tissue to be resected. Note that a base-to-height ratio of 1:3 for this anteriorly pedicled labial flap must not be exceeded. Otherwise impaired wound healing would result. After the marked resection figure has been excised, the anterior portion of the labium is sutured into the defect created, forming the new labial margin.
▶Advantages. Particularly suitable for long and loose labia minora. The scar is barely visible.
▶Disadvantages and Complications. The posterior edge of the wound is located close to the vaginal introitus and can become symptomatic, particularly if scarring occurs. Partial loss of the posterior gland exit ducts can lead to impaired lubrication (▶Fig. 4.13, ▶Fig. 4.14a-d).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree