© Springer International Publishing Switzerland 2016
Alberto Di Giuseppe and Melvin A. Shiffman (eds.)Aesthetic Plastic Surgery of the Abdomen10.1007/978-3-319-20004-0_4545. Outcomes of Traditional Cosmetic Abdominoplasty in a Community Setting
(1)
Department of Plastic Surgery and Reconstructive Surgery Department, Campus Bio-Medico University of Rome, School of Medicine, V. Alvaro del Portillo, 200, Rome, 00128, Italy
45.1 Introduction
Abdominoplasty was first described in 1990 [1]. The technique mainly aimed to correct both body contouring abnormalities of the anterior trunk, from the lower border of the rib cage to the inguinal and pubic areas, and symptoms associated with abdominal tissue excess. Since its first description, abdominoplasty has become one of the top five most commonly performed cosmetic surgery procedures, and it may be associated with other ancillary procedures, such as liposuction [2]. Initially, it consisted of simple wedge excision, addressing lower abdominal tissue excess. Later modifications of the technique included a vertical elliptical resection introduced by Babcock [3] and the low transverse incision, which was described by Pitanguy in 1967 [4], both with wide undermining of the abdominal wall. Grazer [5] later modified the Pitanguy technique by adding plication of the rectus muscle aponeurosis without incising the anterior rectus fascia. Several attempts at classifying abdominoplasty procedures have been made [6, 7] so that plastic surgeons now have a much wider range of choices for operative correction of abdominal deformities. The surgical technique is selected according to preoperative patients’ characteristics and expectations including localized fat deposits, obesity, muscle and skin laxity, fitness, scars from previous surgery, age, pregnancies, hormone replacement therapy, menopause, and genetics. Because of the variability and variety of factors associated with this operation, surgeons must be well cognizant of potential complications and outcomes.
45.2 Patient Preoperative Assessment
An accurate assessment of medical history, psychological profile, and deformities is an essential component of successful body contour patient selection. As previously anticipated, significant medical problems that may affect the outcome of surgery include hypertension and/or deep venous thrombosis, coronary artery disease and/or other blood disorders, intake of drugs that may affect coagulation, chronic obstructive pulmonary disease, obesity, diabetes, HIV infection, previous miscarriages, age older than 40 years, and a history of abdominal hernia. An additional factor is a history of intra-abdominal operations. The location of pre-existing scars is fundamental in determining the surgical technique. Although most infraumbilical scars are removed during abdominoplasty, supra- or paraumbilical scars may involve problems, such as impaired blood supply to skin flaps or difficult dissection in the scar tissue.
Permanent abdominal tissue excess mainly derives from massive weight loss, resulting from diet, surgery, and pregnancies. This condition can cause functional and psychological disorders, which may severely affect a normal life. In the more severe cases, the tissue excess is associated with musculoaponeurotic laxity of the abdominal wall, which has been demonstrated to cause back pain and respiratory impairment [8–10]. Furthermore, the number of patients suffering from an oversized apron of excess skin after massive weight loss is dramatically increasing within western society, mainly due to the increasing number of obese people undergoing bariatric surgery. The later includes a variety of procedures performed on people with extreme obesity.
45.3 Restrictive and Malabsorptive Operations
Restrictive operations aim only to restrict food intake and do not interfere with the normal digestive process. The surgeon isolates a small pouch at the top of the stomach, so that most people lose the ability to eat large amounts of food at one time. Restrictive operations for obesity include adjustable gastric banding (AGB), vertical banded gastroplasty (VBG), sleeve gastrectomy, gastric balloon, and gastric plication. Restrictive operations are less effective than malabsorptive operations in achieving substantial, long-term weight loss. Furthermore, successful results depend on the patient’s willingness to adopt a long-term plan of healthy eating and regular physical activity. Body contouring surgery has to be planned at least 1 year after weight loss is stabilized.
Restrictive procedures combined with decreased absorptive operations are the most common gastrointestinal surgeries for weight loss. They restrict both food intake and the amount of calories and nutrients the body absorbs. The principal malabsorptive techniques are the following:
1.
Roux-en-Y gastric bypass (RGB). This operation has become the most common and successful bypass surgery. First, a small stomach pouch is created to restrict food intake. Next, a Y-shaped section of the small intestine is attached to the pouch to allow food to bypass the lower stomach, the duodenum, and the first portion of the jejunum. This bypass reduces the amount of calories and nutrients the body absorbs.
2.
Biliopancreatic diversion (BPD). In this procedure, portions of the stomach are removed. The small pouch that remains is connected directly to the final segment of the small intestine, completely bypassing the duodenum and the jejunum. Although this procedure successfully promotes weight loss, it is used less frequently than other types of surgery because of the high risk for nutritional deficiencies.
3.
Duodenal switch. A variation of BPD includes a “duodenal switch,” which leaves a larger portion of the stomach intact, including the pyloric valve. It also keeps a small part of the duodenum in the digestive pathway. This procedure is more commonly performed than the BPD but far less than the bypass or the band.
Malabsorptive operations with gastric restriction are regularly effective in reversing the health problems associated with severe obesity. These patients generally lose two thirds of their excess weight within 2 years. The long list of comorbidities is corrected or at least greatly relieved. Malabsorptive operations do increase the risk for nutritional deficiencies because of duodenum and jejunum bypass, where most iron and calcium are absorbed. Menstruating women may develop anemia because not enough vitamin B12 and iron are absorbed. Decreased absorption of calcium may also bring on osteoporosis and metabolic bone disease. Patients need nutritional supplements such as iron, calcium, and vitamins A, B 12, D, E, and K.
RGB and BPD operations cause unpleasant dumping syndrome, due to rapid movement of stomach contents through the mid-small intestine. Highly refined sugars and fats are most likely to cause immediate profound nausea, weakness, sweating, faintness, and diarrhea [11].
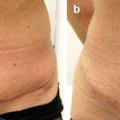
45.4 Outcomes
Abdominoplasty has become a well-established surgical procedure; nevertheless, complication rates are quite high. However, patients’ benefits from this operation are nowadays incompletely studied, and the actual complication rate remains elusive because of the paucity of large studies. The documentation is almost exclusively based on clinical experience and retrospective case series.
According to their severity, complications could be designated as major and minor. Major complications are generally defined as seromas requiring aspiration, hematomas requiring evacuation, deep venous thrombosis/pulmonary embolism, and infections requiring antibiotics. Minor complications are instead defined as seromas and hematomas not requiring intervention, stitch abscess, fat necrosis, wound dehiscence, umbilical necrosis, and hypertrophic scarring. Hensel et al. [12] reported an overall complication rate of 32 % with only a 1.4 % major complication rate.
Furthermore, a retrospective review stratified complications according to “early” and “late” onset. In this series, the “early” complications (18 %) included seroma, hematoma, infection, venous embolism, skin or fat necrosis, and delayed wound healing [13, 14]. In the same study, 25 % of patients experienced “late” complications, which were largely aesthetic-related issues, including dog ears, localized fatty excess, and unsatisfactory scars.
However, complications depend on several factors, including the type and number of procedures performed, the patients’ risk factors, and the modality of weight loss [15], as described previously. In fact, it has been proved that there is a significant increase in minor complication rates in smokers and patients with diabetes and/or hypertension. Patients suffering from morbid obesity (BMI ≥ 40) are instead more likely to develop major complications. Some studies demonstrated that men are more at risk of developing major and minor complications [16].