(1)
Klinik für Plastische Gesichtschirurgie, Marienhospital Stuttgart, Stuttgart, Germany
Electronic supplementary material
The online version of this chapter (doi:10.1007/978-3-662-49706-7_9) contains supplementary material, which is available to authorized users.
Keywords
OsteotomyPercutaneous osteotomyNasal pyramidBroad noseDeviated nosePowered instruments9.1 Surgical Principles
Surgical alteration of the bony pyramid is often anxiety-provoking for the prospective rhinoplasty patient. Just talking about “breaking” the bone in the middle of the face creates fear and apprehension. However, contemporary techniques, combined with sophisticated cutting instruments, intraoperative ice-water cooling, and postoperative mechanical cooling devices to minimize swelling and bruising, have greatly improved surgery of the bony vault. Yet despite technical advances, the most important factor is still a well-conceived and individualized treatment plan executed with meticulous precision and extreme care.
Our treatment philosophy seeks to create bone fragments that are as large as possible and to mobilize them completely so that it becomes much easier to mold a new bony pyramid. Typically this is done using parasagittal medial osteotomies, percutaneous transverse osteotomies, and percutaneous low-to-low lateral osteotomies (Fig. 9.1). By using a 2- or 3-mm osteotomies and the percutaneous technique for the transverse and lateral osteotomies, the blunt force energy is applied at right angles to the bone for more precise bone cut placement, and by using a mallet made from Teflon, the blunt force energy is dissipated like a shock absorber for less tissue trauma. Using this approach, we feel that we can avoid many of the complications resulting from unwanted bony comminution or misplaced bone cuts. We also use a single-access incision for each percutaneous osteotomy (Fig. 9.2). For the lateral osteotomy, the skin incision is placed at the junction of the caudal and medial thirds, and for the transverse osteotomy, the incision is placed at the junction of the central and middle thirds (Fig. 9.3). After inserting the osteotome, we also score the periosteum along the fracture line to displace blood vessels and minimize bleeding and to get a glas cutter effect (Fig. 9.4). Finally, in our practice we have not observed medial displacement of the inferior turbinate head with the low-to-low lateral osteotomy, and therefore we are not using a high-to-low-to-low technique for preserving Webster’s triangle.





Fig. 9.1
Options for osteotomy configurations. Straight osteotomy lines produced by parasagittal medial, transverse, and percutaneous low-to-low lateral osteotomies. Curved osteotomy lines produced by conventional high-to-low-to-high lateral and medial oblique osteotomies

Fig. 9.2
Stab incision for percutaneous transverse osteotomy

Fig. 9.3
Percutaneous transverse and low-to-low lateral osteotomy. Lindemann fraise for parasagittal medial osteotomies. Making the percutaneous stab incision for the transverse and lateral osteotomies

Fig. 9.4
Pushing away the vessels by scratching on the bone. Placement of the percutaneous access incisions
When performing the parasagittal medial osteotomy (which is always performed first), we are occasionally confronted with the challenge of achieving straight and symmetrical osteotomy lines when the bony vault is asymmetrical (Fig. 9.5). When a large hump is first removed, a large open roof is produced, and medial osteotomies are unnecessary. But in cases with a small dorsal hump and thick dorsal bone, or in those without a dorsal hump, creation of symmetrical medial osteotomies is best achieved using the Lindemann fraise (Fig. 9.6). Using a power-driven Lindemann fraise, the parasagittal cuts are performed from the inside out and extend cephalically near the intercanthal line. In addition to parallel and straight bone cuts, the Lindemann osteotomies also remove the excess bone (Fig. 9.5) that prevents adequate narrowing of the bony vault. Low-to-low lateral osteotomies are performed next, and the procedure is then completed with transverse osteotomies to fully mobilize the bone fragments. Only in few cases do we perform an oblique osteotomy, which can also be performed with a Lindemann fraise (Fig. 9.7). Ice-water irrigation is then used to prevent bleeding and reduce swelling.
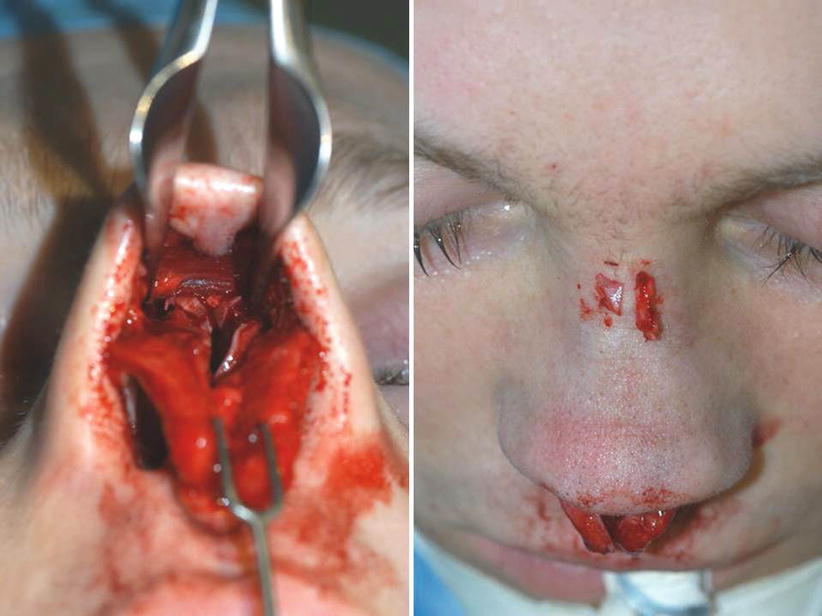


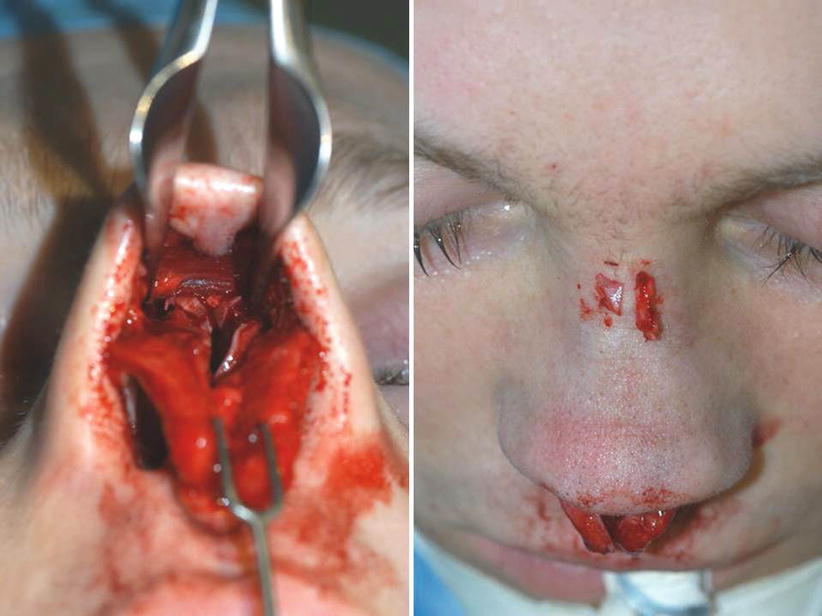
Fig. 9.5
Intraoperative photograph showing enlarged open roof and excised unequal bone fragments after parasagittal medial osteotomy with a 5-mm chisel

Fig. 9.6
Paramedian osteotomy with a Lindemann fraise

Fig. 9.7
Oblique osteotomy with a Lindemann fraise
We apply ice water for some minutes, which helps to reduce bleeding and swelling. These techniques help to mobilize the nasal pyramid best, and from our point of view, this is the prerequisite for straightening or narrowing any disfiguration of the nasal pyramid.
Complete mobilization of the bony vault is a prerequisite for straightening and/or narrowing a misshapen bony nasal pyramid. However, aggressive skeletal mobilization also necessitates prolonged external splinting for a favorable surgical outcome. For most noses, 2 weeks of postoperative splinting is adequate, but for a very wide bony vault, we prefer 3 weeks of immobilization using a plaster of Paris splint extending onto the forehead and reinforced by a circular bandage to minimize movement from the mimetic musculature. Removal of the splint after 2 weeks in these cases may result in recurrence of a wide nose (Fig. 9.8).


Fig. 9.8
Plaster of Paris splint extending onto the forehead and reinforced by a circular bandage
9.2 Case Studies: Primary Nasal Pyramid Correction
9.2.1 Case 1: Wide Nasal Bridge
A 20-year-old female presented with a low and very wide nasal dorsum and a wide and bulky nasal tip. Endonasal examination also revealed a severe deformity of the anterior septum.
An extracorporeal septoplasty was needed to thin the widened bony septum and to reconstruct the anterior segment. After thinning the bony septum, a large piece of quadrangular cartilage was added to serve as a new caudal septum, and spreader grafts were added for support. The bony vault was then narrowed using parasagittal medial osteotomies created with the Lindemann fraise, including removal of a strip of bone followed by percutaneous low-to-low lateral and transverse osteotomies. Using the low-to-low lateral osteotomy also helped to increase dorsal height.
The wide nasal tip was contoured by resecting the cephalic margin of the overly stiff lower later cartilages (LLCs) and by using both transdomal and spanning sutures. The septi depressor muscle was partially resected, allowing the columellar pedestal to be narrowed with transfixion sutures. Further contouring was achieved with alar rim graft placement and with morselized cartilage grafts to augment both soft-tissue facets. A tip suspension suture was also used to maintain tip position (Fig. 9.9).











