Orthognathic Surgery
Stephen B. Baker
INTRODUCTION
Orthognathic surgery is the term used to describe surgical movement of the tooth-bearing segments of the jaws. Patients with dentofacial deformities that cannot be treated with orthodontics alone are candidates for jaw surgery. These malocclusions are typically associated with skeletal discrepancies secondary to congenital anomalies, congenital syndromes, nonsyndromic dentofacial abnormalities, or trauma. Approximately 2.5% of the American population has occlusal discrepancies severe enough to require surgical correction.1 Regardless of the etiology, patient examination and treatment planning principles are the same. The goal of orthognathic surgery is to establish ideal dental occlusion with the jaws in a position that optimizes facial aesthetics.
BASIC DENTAL TERMINOLOGY
Apertognathia—Vertical separation of the maxillary and mandibular anterior teeth, frequently described as anterior open bite.
Articulator—A mechanical device that simulates the temporomandibular joints and jaws to which the maxillary and mandibular casts may be attached.
Buccal—Pertaining to or adjacent to the cheek.
Cast—A plaster replica of the teeth and surrounding tissues.
Centric occlusion—The relation of opposing occlusal surfaces that provides the maximum planned contact or intercuspation.
Centric relation—The relationship of the mandible to the maxilla when the condyles are in their most posterosuperior unstrained positions in the glenoid fossa.
Cephalometric radiograph—A radiograph of the head made with precise reproducible relationships between X-ray source, subject, and film.
Class I occlusion—The mesiobuccal cusp of the first permanent maxillary molar occludes in the buccal groove of the permanent mandibular first molar.
Class II malocclusion—The mesiobuccal cusp of the first permanent maxillary molar occludes mesial to the buccal groove of the permanent mandibular first molar.
Class III malocclusion—The mesiobuccal cusp of the first permanent maxillary molar occludes distal to the buccal groove of the permanent mandibular first molar.
Distal—Away from the median sagittal plane of the face and following the curvature of the arch
Labial—Pertaining to the lip, especially in reference to the surface of a tooth.
Lingual—Pertaining to the tongue, especially in reference to the surface of a tooth.
Mesial—Situated toward the midline of the dental arch.
Overjet—Degree to which the upper incisors extend beyond the lower incisors labially. Normal overjet is 2 mm.
Overlap—The amount maxillary incisal edges vertically overlap the mandibular incisor edges with the mouth closed. Normal incisal overlap is 2 mm.
Palatal—Pertaining to the palate, especially in reference to the surface of a tooth.
Proclination—Anterior angulation of the anterior teeth.
Prognathic—A forward position of the mandible in relation to the cranial base.
Retroclination—Posterior angulation of the anterior teeth.
Retrognathic—The condition of a mandible that is posteriorly positioned in relation to the cranial base.
ESTABLISHING THE DIAGNOSIS
History
An accurate understanding of the chief complaint is essential in developing a treatment plan. Systemic diseases, such as juvenile rheumatoid arthritis, diabetes, and scleroderma, may affect treatment planning. With jaw asymmetries, a history of hyperplasia or hypoplasia secondary to a syndrome, traumatic accident, or neoplasm will affect treatment considerations. Each patient should be questioned regarding symptoms of temporomandibular joint (TMJ) disease or myofascial pain. Motivation and realistic expectations are extremely important to ensure an optimal outcome. It is important for the patient to have a clear understanding of the procedure, the recovery, and the anticipated result prior to surgery. Orthognathic surgery is a major undertaking, frequently lasting 2 to 3 years, and the patient must be appropriately motivated to undergo all necessary perioperative orthodontic treatment and rehabilitation to achieve the desired result. When it comes to jaw surgery, the patient is a particularly important member of the orthognathic surgery team.
Physical Examination
Good oral hygiene and periodontal health is necessary prior to orthodontics and surgery. The occlusal classification is determined, and the degree of incisor overlap and overjet is quantified. Often, the clinician can get a sense of the degree of dental compensation (see below) on physical examination, but radiographic analysis is necessary to quantify dental compensation. The surgeon should assess the transverse dimension of the maxilla. If a crossbite is present, models are obtained to differentiate a relative crossbite from a true crossbite. An absolute crossbite is due to maxillary constriction and will require either orthopedic (orthodontic appliance) or surgical expansion to correct (see below). If the mandibular third molars are present, they will require extraction 6 months before performing a sagittal split osteotomy. Any missing teeth and periapical pathology are noted. Any signs or symptoms of TMJ dysfunction are evaluated before proceeding with surgery.
The frontal facial evaluation consists of assessing the vertical facial thirds: trichion to glabella, glabella to subnasale, and subnasale to menton. Each of these facial thirds should be about equal. If the lower two-thirds of the face are short, they can be increased by inferiorly repositioning the maxilla, which will result in increasing the distance from the glabella to pogonion. In contrast, a long lower face may benefit from a maxillary impaction, which would have the opposite effect. The most important factor in determining the ideal vertical height of the maxilla is the amount of incisor showing while the patient’s lips are in repose. A man should show at least 2 to 3 mm while as much as 4 to 5 mm is considered attractive in a woman. If the patient shows the correct degree of incisor in repose but shows excessive gingiva in full smile, the maxilla must not be impacted. It is more important to show the correct degree of incisor in repose than it is to be concerned about excess gingiva in full smile. The surgeon certainly would not want to bury the incisors in repose just to reduce
the degree of gingiva in a full smile. If lip incompetence or mentalis strain is present, it is usually an indicator of vertical maxillary excess.
the degree of gingiva in a full smile. If lip incompetence or mentalis strain is present, it is usually an indicator of vertical maxillary excess.
The sagittal facial fifths are also evaluated. The intercanthal distance should be about the same as the distance between the medial and lateral canthus of each eye. If the lateral fifths are deficient, augmentation can be performed with bone grafts or implants. The inferior orbital rims, malar eminence, and piriform areas are evaluated for the degree of projection. If these regions appear deficient, maxillary advancement is indicated; if they are excessively prominent, the maxilla may benefit from posterior repositioning. The alar base width should also be assessed prior to surgery since orthognathic surgery may alter the width (Chapter 48). Asymmetries of the maxilla and mandible should be documented on physical examination, and the degree of deviation from the facial midline noted. The soft tissue envelope of the upper face is evaluated for descent of the malar fat pads, the severity of the nasolabial creases, and folds. Skeletal movements of the maxilla will affect these areas. It is important for the surgeon to realize that skeletal expansion (anterior or inferior repositioning of the jaws) will attenuate the creases and folds, while skeletal contraction (posterior or superior movements of the jaws) will accentuate these problems.2 The surgeon certainly does not want to give the patient a prematurely aged appearance as a result of the procedure. However, as will be discussed later, the surgeon can take advantage of skeletal expansion to reduce some of these soft tissue creases giving the patient a youthful appearance and reducing the signs of aging. In evaluating the chin, the clinician assesses the labiomental angle (Chapter 51). An acute angle indicates a short or prominent chin, while effacement of the crease suggests excessive vertical length or insufficient anterior projection.
The profile evaluation focuses on the projection of the forehead, the malar region, the upper and lower jaws, the nose, the chin, and the neck. The assessment can be verified through cephalometric analysis, but an experienced clinician can usually determine whether the deformity is due to the maxilla, mandible, or both. Frequently, the optimal aesthetic result is achieved by ignoring the cephalometric norms and treatment planning the jaw movements based on the patient’s facial form as determined by the surgeon’s physical examination. If the jaws appear to be aligned but the chin projection is either pronounced or deficient, a genioplasty may be all that is necessary (Chapter 51). The proper position of the nose relates to the upper lip, which is supported by the maxillary incisors, and the chin. Because both of these structures may be altered by orthognathic surgery, it is important to predict how the dimensions of the nose will fit into the new facial proportions (Chapter 48). A rhinoplasty may be necessary to maintain proper facial proportions. The soft tissues of the neck should also be assessed. The patient with submental laxity will not benefit aesthetically from posterior positioning of the mandible. Mandibular advancement, however, will improve the laxity and the cervicomental angle. In a patient with prominent submental fat in whom mandibular advancement is contraindicated, suction-assisted lipectomy is helpful in removing the adipose deposits (Chapter 65). Redundant skin will require direct excision.
The maxillary and mandibular dental midlines are assessed to determine if they are congruent with each other and the true facial midline. Any deviations are noted and quantified. The presence of mandibular third molars is noted because if a sagittal split osteotomy is planned, it is recommended that they be removed 6 months before surgery so the screw fixation has adequate bone. The presence and degree of dental compensation is also recorded. The term “dental compensation” is used to describe the tendency of teeth to tilt in a direction that minimizes the dental malocclusion. For example, in a patient with an overbite (class II malocclusion), the upper incisors will retrocline while the lower incisors will procline. The opposite will occur in a patient who has dental compensation for an underbite (class III malocclusion). Thus, dental compensation will mask the true degree of skeletal discrepancy. Precise analysis of the dental compensation is done on the lateral cephalometric radiograph.
If the patient desires surgical correction of the deformity, presurgical orthodontics will decompensate the occlusion, thereby reversing the compensation that has occurred. Decompensation has the effect of exaggerating the malocclusion but allows the surgeon to maximize skeletal movements. If the patient is ambivalent or not interested in surgery, mild cases of malocclusion may be treated by further dental compensation. Compensation will camouflage the deformity and restore proper overjet and overlap. The dental movements for decompensation and compensation are in opposite directions, making a decision regarding surgery and communication between surgeon, orthodontist, and patient extremely important.3
Cephalometric Analysis and Dental Models
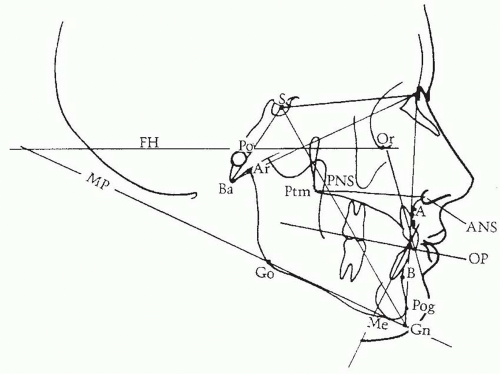
A lateral cephalometric radiograph is performed under reproducible conditions so that serial images can be compared. This film is usually taken in the orthodontist’s office utilizing a cephalostat, an apparatus specifically designed for this purpose, and head frame to maintain consistent head position. It is important to be certain that the surgeon can visualize bony as well as soft tissue features on the image to facilitate tracing all the landmarks. A piece of transparent acetate tracing paper is secured with tape over the radiograph and the following landmarks are traced: sella, inferior orbital rim, nasion, frontal bone, nasal bones, maxilla, maxillary first molar and central incisor, external auditory meatus, the condylar head and mandible, and the mandibular first molar and incisor. The soft tissue of the forehead, nose, lips, and chin is also traced. Once the normal structures are traced, several planes and angles are determined (Figure 25.1).
The maxillary plane is represented by a line drawn between the anterior nasal spine (ANS) and posterior nasal spine (PNS). The occlusal plane is drawn between the occlusal surfaces of the teeth. The mandibular plane is drawn between menton and gonion, and the Frankfort horizontal plane is delineated between the superior portion of the external auditory meatus (porion) and the inferior orbital rim (orbitale). Analysis of these planes aids in establishing an accurate diagnosis. A steep mandibular plane is usually associated with a class II malocclusion, anterior open bite, and a short mandible. A shallow mandibular plane is associated with a deep bite, class III malocclusion, and a long mandible.
The SNA and SNB are the two most important angles in determining the positions of the maxilla and mandible relative to each other as well as to the cranial base. These angles are determined by drawing lines from sella to nasion to point A or point B, respectively. By forming an angle with the sella and nasion, this position is related to the cranial base. The maxilla will be considered first. Point “A” represents the anteroposterior position of the maxilla. If the SNA angle is excessive, the maxilla exhibits abnormal anterior position relative to the cranium. If SNA is less than normal, the maxilla is posteriorly positioned relative to the cranial base. The same principle applies to the mandible; the only difference is that point “B” is used to relate mandibular position to the cranial base. The importance of the cranial base as a reference is that it allows the clinician to determine if one or both jaws contribute to the deformity. For example, a patient’s class III malocclusion (underbite) could develop from several different etiologies: a retrognathic maxilla and normal mandible, a normal maxilla and a prognathic mandible, a retrognathic mandible and a more severely retrognathic maxilla, or a prognathic maxilla and a more severely prognathic mandible.
All of these conditions yield a class III malocclusion, yet each requires a different treatment approach. The surgeon can delineate the true etiology of the deformity by relating the maxilla and mandible independently to a stable reference point, the cranial base.
All of these conditions yield a class III malocclusion, yet each requires a different treatment approach. The surgeon can delineate the true etiology of the deformity by relating the maxilla and mandible independently to a stable reference point, the cranial base.
Plaster dental casts are obtained during the treatment planning process. Casts are useful because they allow the surgeon to evaluate the occlusion when the casts are articulated into the proper position. Analysis of the new occlusion gives the clinician an idea of how intensive the presurgical orthodontic treatment plan will be. Casts also allow the clinician to distinguish between absolute and relative transverse maxillary deficiencies. Absolute transverse maxillary deficiency presents as a posterior crossbite with the jaws in a class I relationship. A relative maxillary transverse deficiency is commonly seen in a patient with a class III malocclusion. As the maxilla is advanced or the mandible retruded, the crossbite is eliminated. Articulation of the casts into a class I occlusion allows the surgeon to easily distinguish between relative and absolute maxillary constriction.
DEVELOPING A TREATMENT PLAN
Once the data are obtained, the surgeon can determine which abnormalities the patient exhibits and the extent to which these features deviate from the norm. However, the treatment plan is the application of this data to give the patient the best aesthetic result while establishing a class I occlusion. The goal is not to “treat the numbers” in an attempt to “normalize” every patient. The appearance of the soft tissue envelope surrounding the facial skeleton is the most crucial factor in determining the aesthetic success of orthognathic procedures, and the jaws should be positioned so that they provide optimal soft tissue support.
Historically, skeletal movements that expanded the soft tissue of the face were less stable, so posterior and superior movements were preferred. Although more stable, these movements resulted in contraction of the facial skeleton with the associated redundancy of soft tissue characteristic of premature aging. Since the introduction of rigid fixation, osteotomies that result in skeletal expansion have been achieved with predictability. It is important that the surgeon develop a treatment plan that will expand or maintain the preoperative volume of the face.2 If a superior or posterior (contraction) movement of one of the jaws is planned, an attempt should be made to neutralize the skeletal contraction with an advancement or inferior movement of the other jaw or the chin. It is important to avoid a net contraction of the facial skeleton as this may result in a prematurely aged appearance.
As skeletal expansion is increased, soft tissue laxity is reduced and facial creases are softened. These effects increase the definition of the face, creating a more attractive appearance. It has been shown that skeletal expansion is aesthetically pleasing even if facial disproportion is necessary to achieve the expansion.4 Fashion models often exhibit slight degrees of facial disproportion and are considered beautiful. The aesthetic benefits the patient receives by expanding the facial envelope frequently justify the small degree of disproportion necessary to achieve them. Even in young adolescent patients that do not show signs of aging, one must not ignore these principles. A successful surgeon will incorporate these principles into the treatment plan of every patient so that as the patient ages, the signs of aging will be minimized and a youthful appearance will be maintained as long as possible (Figure 25.2).
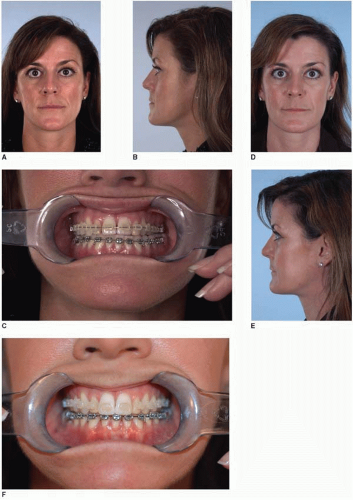
An example demonstrating these principles is an adult woman who presents for surgery with a slightly prognathic mandible, submental laxity, jowl descent, and deep nasolabial creases. If a treatment plan were developed based solely on cephalometric values, a mandibular setback would be the appropriate procedure. This procedure would do nothing for the upper face and would accentuate the submental laxity and jowl descent. In contrast, if one were to accept the slight prognathism and advance the maxilla to a class I relationship, the nasolabial crease and jowl descent would be improved, and the submental laxity would not be made worse. Thus, moving the normal maxilla into a class I occlusion with a prognathic mandible establishes a normal occlusion and achieves excellent aesthetics despite being slightly disproportionate (Figure 25.3).
A class I occlusion can be achieved with the jaws in a variety of different positions. The goal in treatment planning is to use the data from the patient’s examination to predict the location of the jaws that will optimize the soft tissue features of the face. Reducing the emphasis on normal values and increasing the awareness of the soft tissue effects of skeletal movements, a skeletal “disproportion” may be chosen intentionally, leading to a more favorable result. However, it is the discretion of the surgeon to incorporate these principles into a treatment plan pleasing to the patient and understood by the patient.4
BASIC APPROACHES TO COMMONLY ENCOUNTERED PROBLEMS
The basic treatment principles in commonly encountered dentofacial deformities will be presented. The surgeon must recognize there are multiple solutions to a single problem; this is where the proper application of the previously discussed principles is crucial to achieving the best aesthetic result.
 FIGURE 25.3. Ignoring cephalometric norms and expanding soft tissue. This is a patient whose cephalometric analysis demonstrated a normal SNA and a high SNB (A-C). Correcting to cephalometric norms would indicate a mandibular setback procedure. In order to optimize the facial soft tissue envelope while restoring a class I occlusion, a decision was made to perform a Le Fort I maxillary advancement. Additionally, her incisal show was deficient so the maxilla was moved inferiorly to restore normal incisal show. The inferior positioning of the maxilla resulted in a clockwise rotation of the mandible reducing the patient’s chin projection as well (D-F).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|