(a–f) Preoperative photography for VAL contouring of the trunk

Preoperative buttocks view
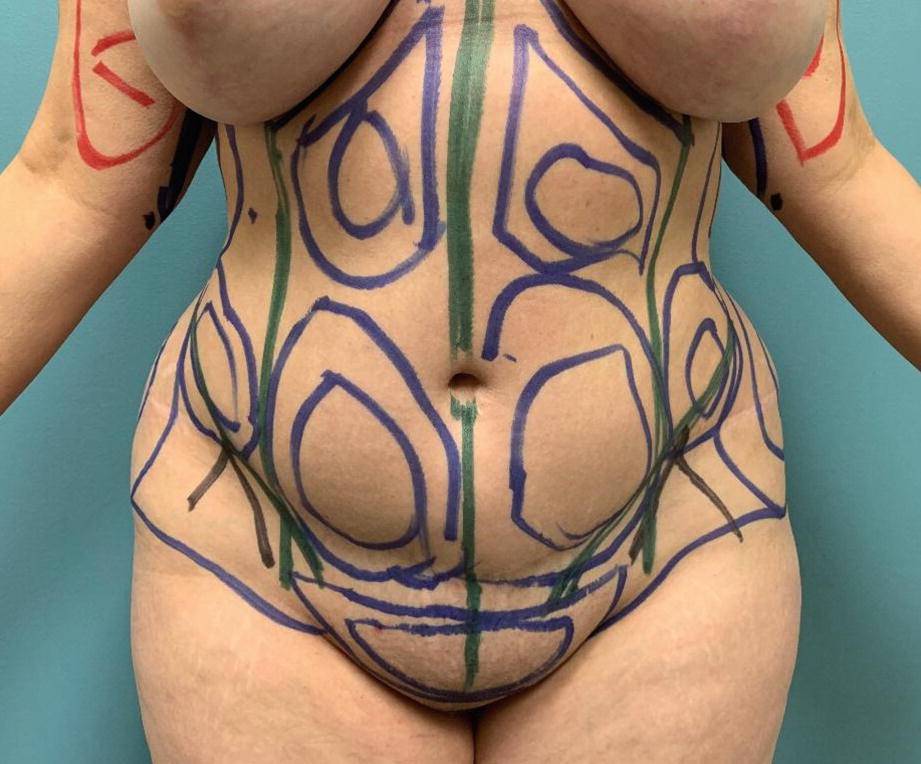
Preoperative markings for VAL contouring of the abdomen
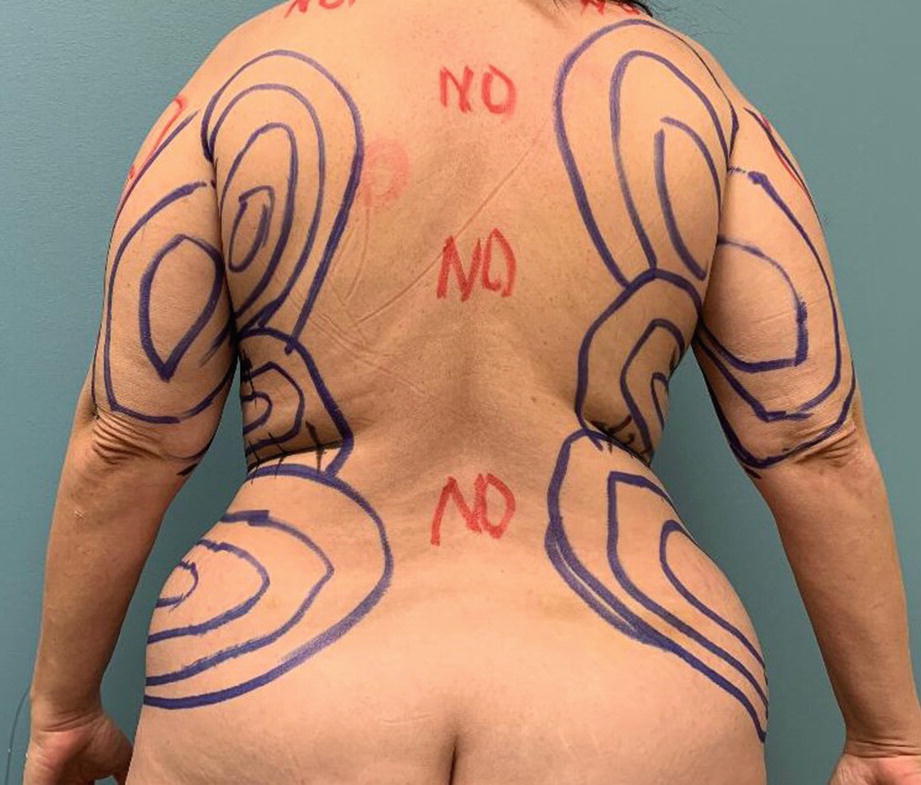
Preoperative markings for VAL contouring of the posterior trunk
Surgical Technique
I typically begin circumferential contouring of the trunk with the back and flanks. There are two options for positioning the patient on the operating table and both have pros and cons. The prone position requires meticulous padding of all pressure points from bony prominences and proper protection of the face and breasts. When starting out in this position under general anesthesia, it is useful to perform the anesthesia induction and endotracheal intubation on the stretcher adjacent to the operating table and then transferring the patient directly to the table in the prone position over the hip rolls and axillary rolls. The operating table is then flexed slightly to provide better lineal access for the VAL probes and avoid torqueing them over the curved anatomical areas of the back and flanks. The prone position provides fairly good access to the back and flanks and the position makes it easier to access symmetry since the surgeon is visualizing both sides simultaneously during the surgery. Another advantage of the prone position in circumferential contouring is that it requires only one additional patient repositioning to the supine position in order to complete the abdominal areas. In spite of these advantages, many experienced body contouring surgeons, including the author, prefer contouring of the posterior trunk in the lateral decubitus position. This position also requires an axillary roll and padding of the bony prominences. Although this position for liposuction requires an additional repositioning (side-side-supine versus prone-supine), many including the author feel that the lateral decubitus position provides better access for UAL cases with less trauma. The position is extremely helpful when evacuating large volumes from the back and flanks and in the creation of small aesthetic waistlines. Once both sides of the posterior trunk are completed, the patient is then turned to the supine position for completion of the abdominal contouring.
It was once common to perform the surgical prepping for circumferential liposuction prior to induction of anesthesia. The patient in the standing position would be sprayed in a circumferential manner using povidone-iodine (Betadine) solution. The operating table would be draped with the sterile sheets and the prepped patient would lay down on the sterile sheets after which the sterile draping would be completed. This prepping and draping method has been abandoned by many including the author who now prefers to prep and drape an anesthetized patient in the surgical position on the operating table using povidone-iodine (Betadine) gel. Access incisions for abdominal VAL are typically placed in the upper pubic area (below the bikini line) on each side and in the midline. Another access incision is placed in the superior internal aspect of the umbilicus for access to the upper abdomen. The author usually performs liposuction surgery of large surface areas under general anesthesia and only small-volume aspirations under local. The “superwet” guidelines call for an approximate 1:1 ratio of fluid infiltrate to expected aspirate volume; however this is not nearly enough wetting solution for VAL surgery. In the author’s experience these cases require a minimum of 3:1 ratio of wetting solution to expected aspirate volume. The idea is to create a blanched and turgid treatment area. The high volume of fluid in the tissues during VAL cases promotes fat fragmentation and offers a measure of thermal protection. Furthermore, high-volume infiltration is associated with cleaner aspirate since the high hydrostatic pressure aids in hemostasis. For most areas of the trunk, the wetting solution is infiltrated by means of an infiltration pump at a rate of 400 ml/minute until the fluid is evenly dispersed throughout the tissues. There are a number of wetting solution formulas described in the literature [6–8]. For major VAL cases under general anesthesia, the author employs Garcia’s formula [9], which consists of 1 ml of epinephrine 1:1000 in 1 liter of Ringer’s lactate at room temperature. Formulas that advocate warming the wetting solution are not recommended for ultrasonic liposuction surgeries. For smaller cases under local anesthesia, 30 ml of 1% xylocaine is added to a liter of the wetting solution. At any rate, if xylocaine is used in the wetting solution, the author does exceed a total dose of 35 mg/kg even though some authors claim to use doses exceeding 50 mg/kg while maintaining a safety margin [10, 11]. Smaller surface area liposuctions performed under local do not require such high volumes of wetting solutions, and large surface area cases under general anesthesia do not require the use of xylocaine, so there is really no good reason to push the limits of lidocaine toxicity in these patients. Following the infiltration of the wetting solution, it can take approximately 15 minutes for the patient to experience the full vasoconstrictive effect of the epinephrine; however unlike aspiration cannulas, gently passing VASER ultrasound probes through the tissues is not associated with bleeding so the ultrasound delivery phase is begun immediately after the wetting solution is infused. Prior to aspirating the ultrasound treated area, the next area in line for treatment undergoes infusion of the wetting solution. Employing this infusion protocol, the author has on occasions used cumulative epinephrine doses of up to 14 mg without untoward effects.
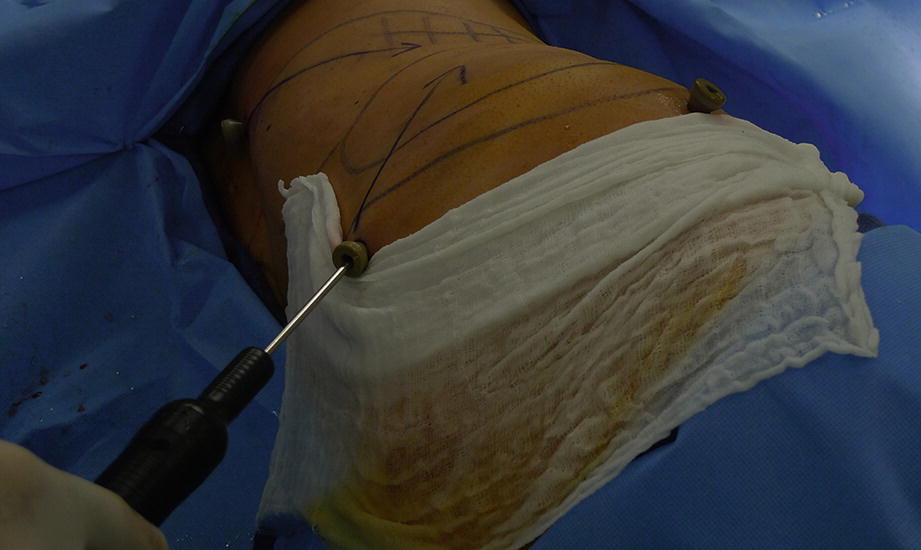
A wet sponge is placed directly behind the skin protectors to protect the skin from the ultrasound probe during the VASER phase of the procedure

Bloodless appearance of typical VASER aspirate

(a–c) TopiFoam silicone-backed foam pads are place in direct contact with the skin of the VAL areas. A compression garment is worn over the TopiFoam
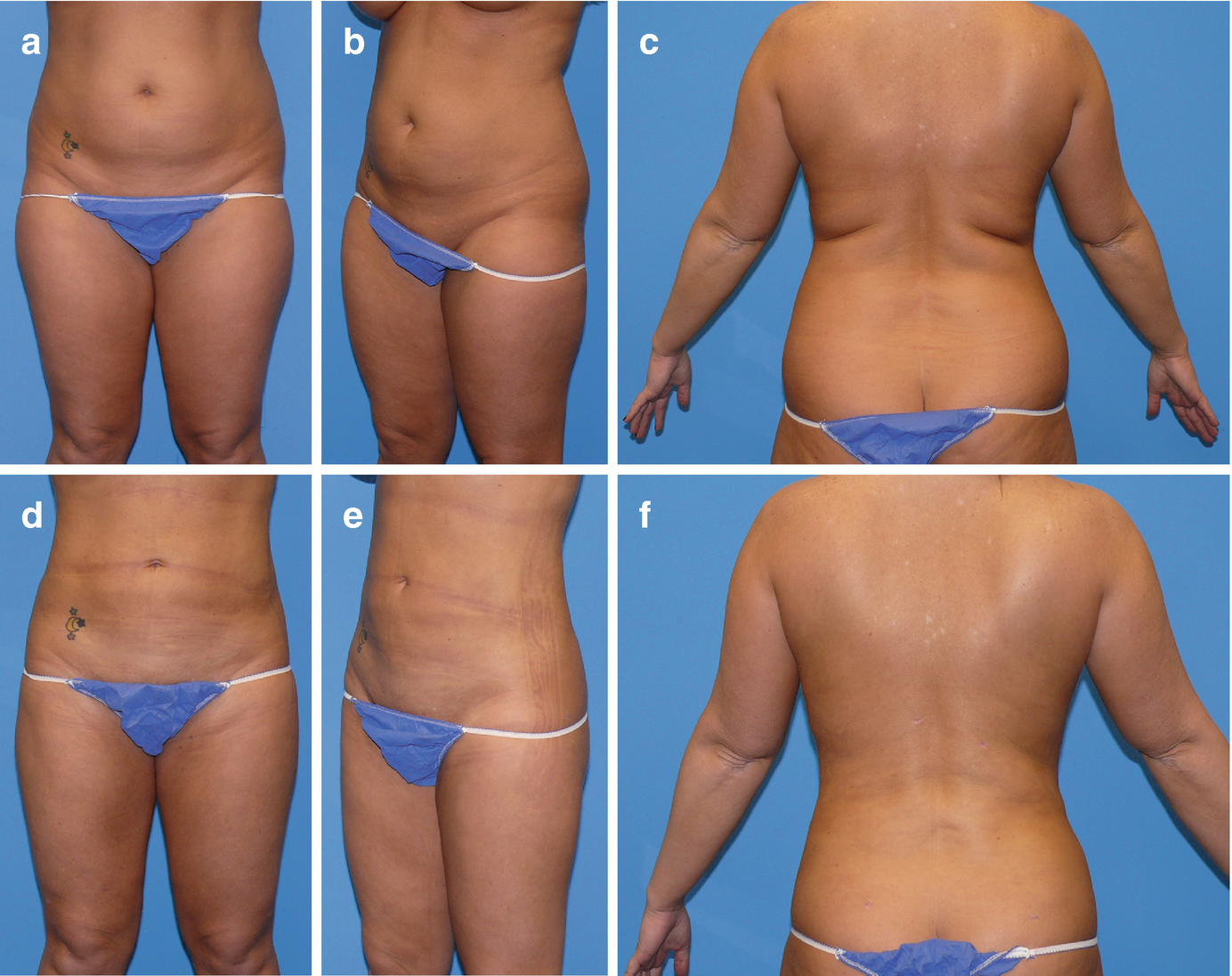
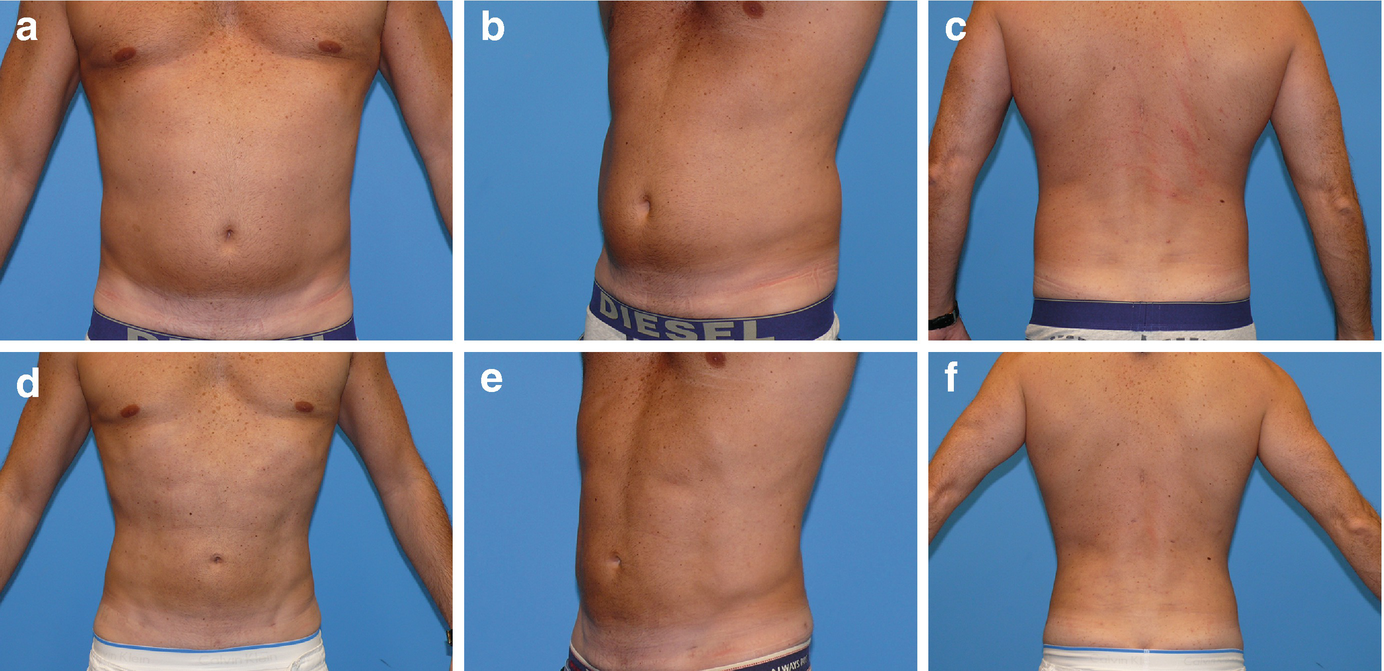
(a–f) A 31-year-old woman 1 year post circumferential VAL of the trunk with extraction of 6400 ml of total aspirate
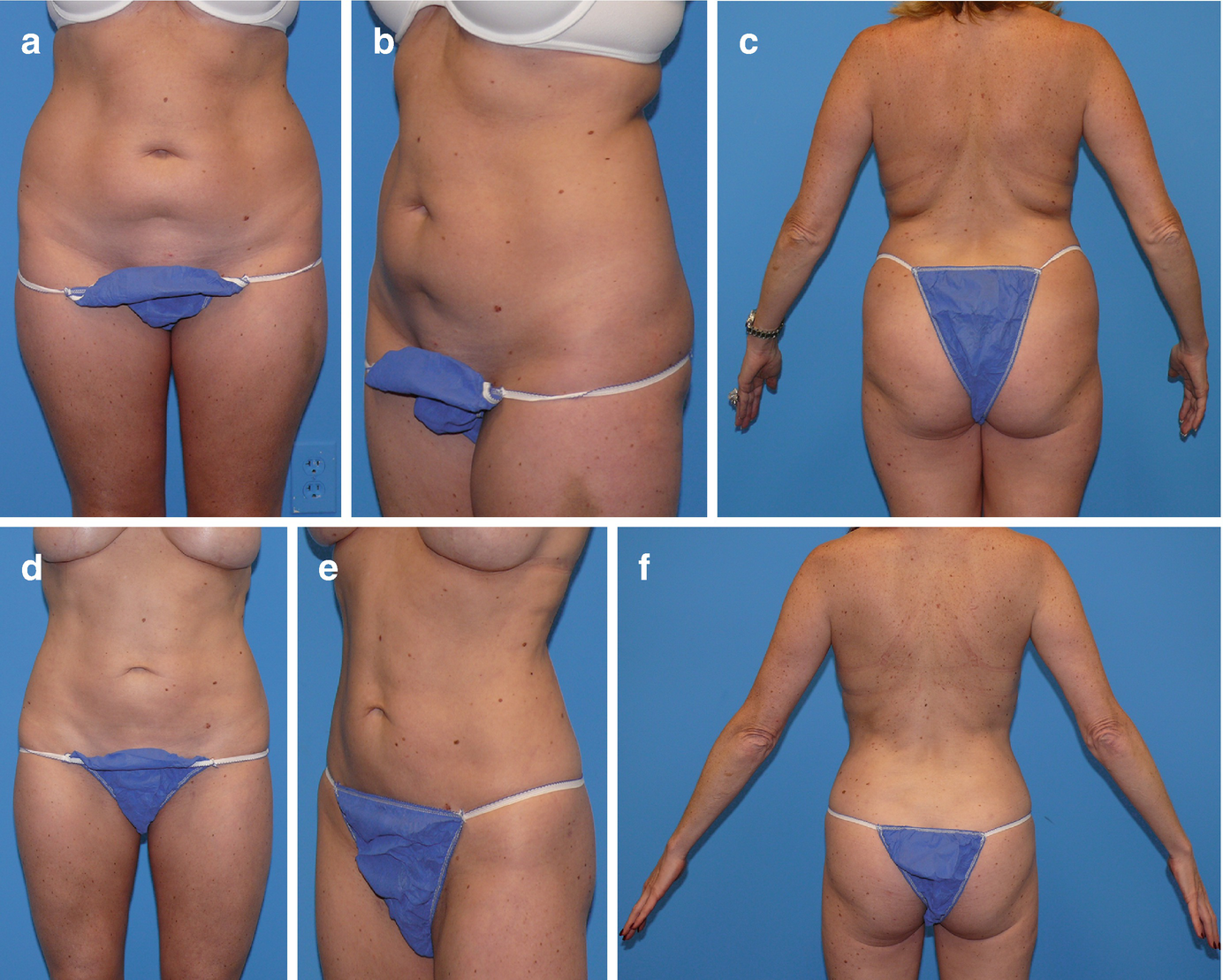
(a–f) A 38-year-old woman 6 months post circumferential VAL of the trunk with correction of lower abdominal contour deformity. Volume extracted was 6800 ml of total aspirate

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








