Nummular Eczema, Lichen Simplex Chronicus, and Prurigo Nodularis: Introduction
|
Nummular eczema is predominantly a disease of adulthood. Men are more frequently affected than women. The peak incidence in both males and females is around 50–65 years of age. There is a second peak in women around 15–25 years of age. Nummular eczema is rare in infancy and childhood. The peak age of onset in childhood is 5 years.1
The pathogenesis of nummular eczema is still unknown. The vast majority of patients with nummular eczema do not have a personal or family history of atopy,2,3 although nummular plaques may be seen in atopic eczema. Numerous factors have been implicated as causal. The state of hydration of the skin in elderly patients has been shown to be decreased.4 The role of infection previously received much attention in the literature. An internal focus of infection, including teeth, upper respiratory tract, and lower respiratory tract, was found in 68% of patients in one study.5 Eleven of thirteen patients without a history of atopic eczema improved after odontogenic infections were treated.6 A role for environmental allergens, such as the house dust mite and Candida albicans has also been touted.4 Nummular eczema has been reported during therapy with isotretinoin and gold.7,8 Generalized nummular eczema is seen in patients with hepatitis C undergoing combination therapy with interferon α-2b and ribavirin.9,10 Mercury amalgam was implicated as a cause in two patients.11
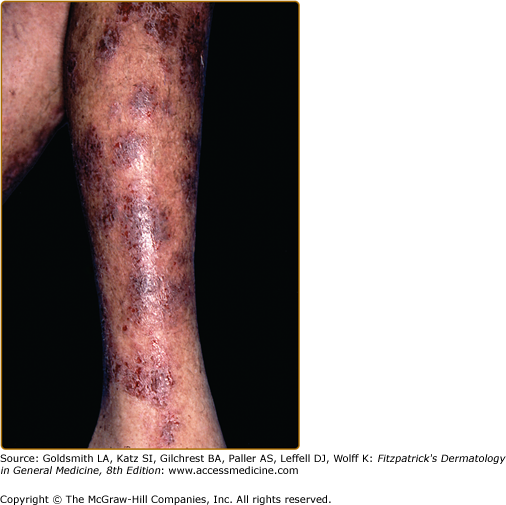
Well-demarcated coin-shaped plaques form from coalescing papules and papulovesicles. Pinpoint oozing and crusting eventuate, and are distinctive (Figs. 15-1 and 15-2). Crust may however cover the entire surface (Fig. 15-3). Plaques range from 1 to 3 cm in size. The surrounding skin is generally normal but may be xerotic. Pruritus varies from minimal to severe. Central resolution may occur, leading to annular forms. Chronic plaques are dry, scaly, and lichenified. The classic distribution of lesions is the extensor aspects of the extremities. In women, the upper extremities, including the dorsal aspects of the hands, are more frequently affected than the lower extremities.2 Exudative discoid and lichenoid dermatitis of Sulzberger-Garbe may represent a variant of nummular dermatitis.12
Patch testing may be useful in chronic recalcitrant cases to rule out a superimposed contact dermatitis. In a series from India, just under half of 50 patients were patch-test positive to colophony, nitrofurazone, neomycin sulfate, and nickel sulfate.13 Serum IgE levels are normal.
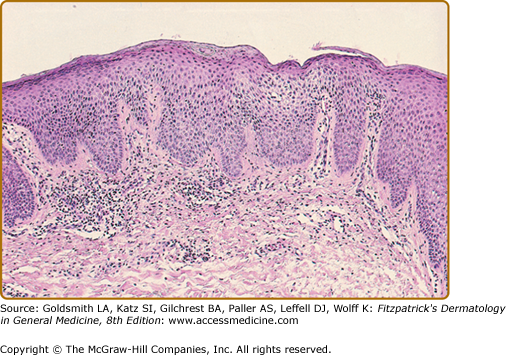
Histopathologic changes are reflective of the stage at which the biopsy is performed. Acutely, there is spongiosis, with or without spongiotic microvesicles. In subacute plaques, there is parakeratosis, scale-crust, epidermal hyperplasia, and spongiosis of the epidermis (Fig. 15-4). There is a mixed cell infiltrate in the dermis. Chronic lesions may resemble lichen simplex chronicus microscopically.
See Box 15-1.
Most Likely
|
Consider
|
Always Rule Out
|
The course is usually chronic. Recurrence at prior sites of involvement is a feature of the disease.5
Topical steroids in the mid- to high-potency range are the mainstay of treatment. The calcineurin inhibitors, tacrolimus and pimecrolimus, and tar preparations are also effective. Emollients can be added adjunctively if there is accompanying xerosis. Oral antihistamines are useful if pruritus is severe. Oral antibiotics are indicated when secondary infection is present. For widespread involvement, phototherapy with broad- or narrow-band ultraviolet B may be beneficial.
Lichen Simplex Chronicus/Prurigo Nodularis
|
|