The importance and effectiveness of prevention efforts and strategies for skin cancers are reviewed. Topical sunscreens and their proper use are presented. Topical and ingested forms of natural, synthetic, or biologic chemical agents that are potentially efficacious for chemoprevention are listtdldted and discussed.
- •
Ultraviolet B (UVB) radiation is the main cause of photocarcinogenesis, sunburn, and immunosuppression.
- •
The amount of UVB is affected by geography (equatorial latitude, high altitude), season (spring, summer), meteorology (a sunny day without clouds), environment (ground reflections such as beach sand and sea), and time of day (midday between 10:00 am and 4:00 pm ).
Introduction
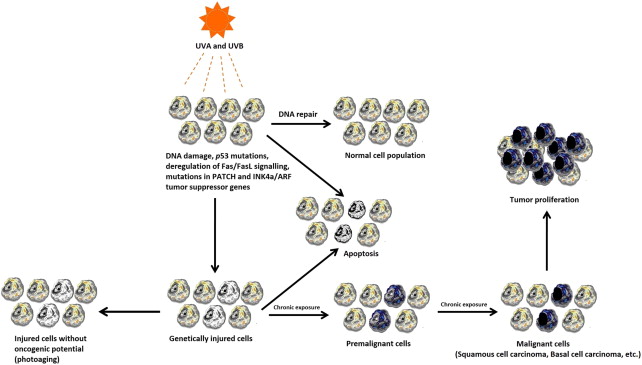
Nonmelanoma skin cancers (NMSCs) are the most commonly diagnosed cancers especially in the white race. The major etiologic factor for the development of NMSCs is the exposure to ultraviolet (UV) radiation (especially UVB and UVA radiation), which may cause DNA damage and genetic mutations in skin ( Fig. 1 ). Because of the detrimental effect of UV radiation, sun exposure is a high risk factor, especially for individuals who have phenotypic factors such as white or cream-white skin type, blue/green eyes, red or blond hair, or have freckles and moles. In addition, human papilloma virus, ionizing radiation, arsenic exposure, and genetic predisposition (such as xeroderma pigmentosum, albinism, or Muir-Torre syndrome) are the other important risk factors.
A recent epidemiologic review about NMSCs has demonstrated that the incidence of NMSCs is increasing, and NMSCs are becoming a health care problem worldwide. The investigators also highlighted that prevention and early detection are of paramount importance. The American Cancer Society emphasized that approximately 80% of all skin cancers are preventable. The prevention of skin cancers can be managed by primary, secondary, and tertiary prevention strategies.
Primary prevention strategies include all the personal, institutional, and governmental efforts that provide the protection of the healthy population from the development of skin cancers.
Secondary prevention strategies include the early detection of skin cancers by performing total-body skin examination and involves case finding (incidental detection of a skin cancer in individuals who were seen for another medical problem or during routine check-up), screening (regular examination of high-risk individuals or population), and surveillance (periodic examination of patients who have suspicious lesions).
In tertiary prevention, a regular and routine total-body skin examination is performed on patients who formerly had a diagnosis of skin cancer; thereby, a secondary skin cancer can be detected and treated instantaneously, when it develops.
In this article, the importance and effectiveness of prevention efforts and strategies for skin cancers are reviewed.
Primary prevention strategies
Primary prevention strategies aim to avoid the development of NMSCs in the population and mainly include knowledge, behaviors, and attitudes about sun protection, chemoprevention, and public education programs.
Sun-Protection Behaviors and Clothing
The evidence has indicated that “intermittent” exposure to the sun increases the risk of development of basal cell carcinoma (BCC); however, squamous cell carcinoma (SCC) is strongly associated with continuing, chronic sun exposure. As solar UV radiation is the major etiologic factor for NMSCs, avoiding exposure to sunlight may lead to a remarkable reduction in prevalence. Sunlight includes different wavelengths, such as infrared and UV. The latter is part of the nonionizing electromagnetic spectrum and is divided into 3 spatial regions according to their wavelengths :
- 1.
Long-wave: UVA; 320–400 nm
- 2.
Mid-wave: UVB; 290–320 nm
- 3.
Short-wave: UVC; 200–290 nm
UV C is mutagenic for human skin; however, it does not reach the surface of the earth.
UV A comprises 90% to 95% of solar UV radiation and has a role in photoaging and immunosuppression; its role in photocarcinogenesis is controversial.
UV B radiation is the main cause of photocarcinogenesis, sunburn, and immunosuppression. The amount of UVB is affected by the following:
- •
Geography: equatorial latitude, high altitude
- •
Season: spring, summer
- •
Meteorology: a sunny day without clouds
- •
Environment: ground reflections, such as beach sand and sea
- •
Time of day: midday between 10:00 am and 4:00 pm
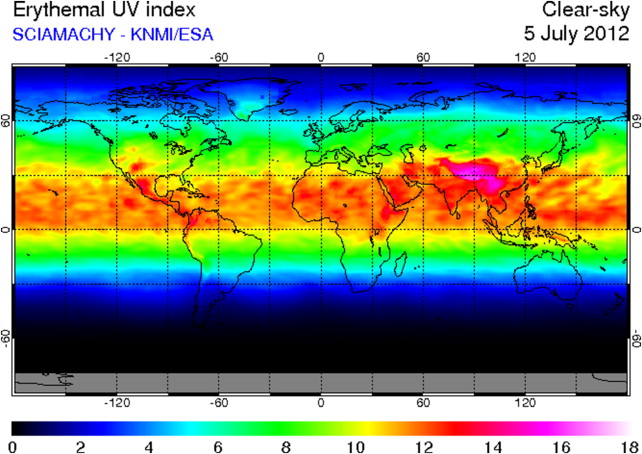
The intensity of UV radiation (also called UV index) is forecasted daily to the public to warn of the hazardous effect of sun ( Fig. 2 ). The UV index is an international standard measurement of the predicted UV radiation of a region and is presented on a scale between 1 and 11+ ( Fig. 3 ). A high number indicates a greater risk of sunburn, especially for high-risk individuals.
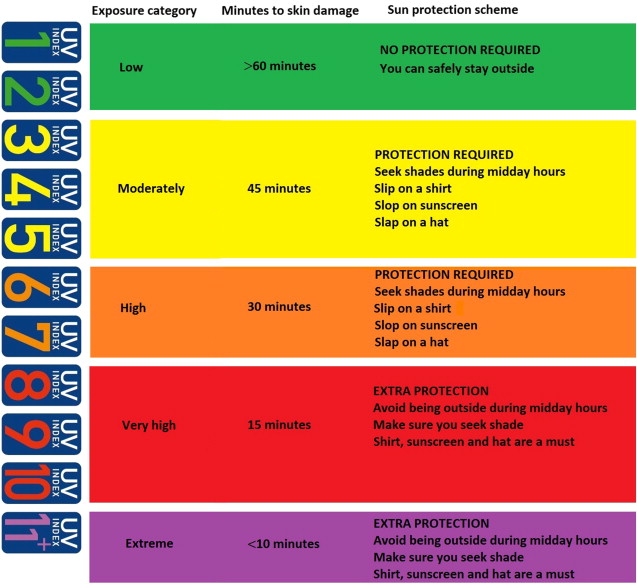
Sun-protection behaviors and attitudes play an important role in the prevention of skin cancer. The recommendations about prevention from sun exposure are briefly presented in Box 1 . Staying indoors to avoid midday sun, especially when the UV index is over 8, is very important for infants, children, adolescents, and even adults. In addition, seeking shade can be somewhat useful for sun protection; however, it does not provide adequate protection from reflected and scattered UV radiation. Clothing is a simple, practical, and effective method for sun protection; however, several studies have demonstrated that most summer garments cannot provide adequate protection against the hazards of sunlight. Therefore, the authors recommend the use of UV-protective clothing items. The UV-protection factor of a garment is a measure that demonstrates its ability to block solar UV radiation, and classified as:
Good: 15 to 24
Very good: 25 to 39
Excellent: 40 to 50 or greater
- •
Avoiding or minimizing exposure to the sun, especially between 10:00 am and 4:00 pm
- •
Watching the daily UV index reports, and staying indoors when the sun exposure category is very high or extreme.
- •
Staying in the shade or using an umbrella.
- •
Wearing sunglasses that block 99% of UVA and UVB radiation.
- •
Avoiding indoor and outdoor tanning.
- •
Wearing sun-protective clothing (preferably UV protection factor 50+):
- ○
A bucket hat with at least a 3-inch brim or legionnaire cap.
- ○
Long-sleeved shirts and long clothing to the ankles, preferably
- ▪
Dark-colored (such as black, navy blue) fabrics
- ▪
Made of synthetic (especially polyester), denim, and wool materials
- ▪
Tightly woven fibers
- ▪
Dry materials
- ▪
- ○
- •
Applying sunscreens with higher SPF (preferably 2 mg/cm 2 or 30 g for the whole body) at least 30 minutes before sun exposure; and reapplying after 90 to 120 minutes or after swimming, showering, toweling, or excessive sweating.
Various reasons may significantly influence the UV-protection factor of apparel textiles: fabric material and porosity, thickness, color, transparency, stretch, and presence of UV-protective absorbers. Therefore, UV-protective textile standards and guidelines have already been established for garment manufacturers and sun-aware consumers.
Topical Sunscreen
Sunscreen was initially marketed in the 1920s in the United States and in the 1930s in Europe, and has become a commercial product since then. To date, many sunscreen products have been manufactured with various combinations of sun-protective chemicals. Sunscreens can provide excellent protection against sunlight when applied appropriately and used responsibly; however, they are accepted as an adjunct technique to other types of sun-protection strategies. They are mainly designed to prevent acute sunburn and tanning. In addition, it has been demonstrated that sunscreens can reduce the formation of actinic damage, solar keratoses, and NMSCs.
An ideal topical sunscreen product should contain active sunscreen ingredients that are nontoxic and stable in the presence of light, water, and/or moisture, and provide good protection against sunlight, UVB and UVA radiation, scavenge-free radicals, and activate DNA repair systems to repair actinic damage. The efficacy of a sunscreen product is denoted by sun protection factor (SPF), which reflects the protection against erythema that is mainly induced by UVB exposure. Sun protection factor basically indicates the ratio of the UVB radiation dose that produces minimal erythema on sunscreen-protected (skin cream thickness of 2 mg/cm 2 ) skin to the UVB radiation dose that produces minimal erythema on unprotected skin. Therefore, the efficiency of photoprotection is greater when the SPF value of a sunscreen product is higher. However, the relationship between SPF value and UVB radiation protection is not linear, which means that a twofold increase in SPF will not cause a twofold increase in UVB radiation protection. For example: a sunscreen with an SPF value of 15 can provide 94% protection against UVB radiation, whereas a sunscreen with an SPF value of 30 can provide 97% protection against UVB radiation. The main drawback of SPF is the photoprotective efficacy of a sunscreen against UVA, which may cause photoaging, immunosuppression, or DNA damage, is not indicated in this grading system. The water resistance of a sunscreen product is labeled with “water resistant (40 minutes),” which indicates protection of up to 40 minutes in continuous water exposure, and “water resistant (80 minutes),” which indicates a protection of up to 80 minutes in continuous water exposure. In addition, most of the recently manufactured sunscreen products contain multiple chemicals and different ingredients to provide broad-spectrum (against UVB and UVA) photoprotection. Ultimately, the American Academy of Dermatology recommends particularly the application of a sunscreen that is broad spectrum, water resistant, and has an SPF value of at least 30 to all exposed regions, such as head, neck, and extremities.
The active ingredients of topical sunscreens are mainly classified as inorganic and organic chemical agents. Inorganic chemical agents act as a physical blocker by reflecting, scattering, and/or absorbing UV and infrared radiation. The major inorganic molecules that are used in sunscreens are zinc oxide and titanium dioxide. Although both titanium dioxide and zinc oxide have a photoprotective effect against UVB and UVA radiation; titanium dioxide is a better photoblocker for UVB, whereas zinc oxide provides better UVA protection. High-quality inorganic sunscreens are now manufactured by micronization and encapsulation; thereby, they are more cosmetically appealing and their protective efficacy against UV radiation increases remarkably. Organic chemical agents principally show their photoprotective effect by absorbing UV radiation, and thereby, prevent penetration to the skin. They mainly contain 3 groups according to their protective characteristics against UVB and UVA radiation :
- 1.
UVB-absorbing sunscreens: cinnamates, p-aminobenzoate (PABA) derivatives, and salicylates, ensulizole, octocrylene.
- 2.
UVA-absorbing sunscreens: avobenzone, ecamsule (terephthalylidene dicamphor sulfonic acid), meradimate (menthyl anthranilate).
- 3.
Dual UVB/UVA absorbing sunscreens: camphor derivatives, oxybenzone.
Most of the topical sunscreens with an SPF value over 30 contain an inorganic and at least 2 organic chemical agents. In addition, other chemicals, such as vitamin C and E, which act as antioxidants and neutralize radical oxygen species generated by UV radiation, and aloe, which decreases the hazardous effects of UV radiation, are also used in several sunscreens.
The protective effect of topical sunscreens against sunburn has been demonstrated in humans. In addition, Green and colleagues reported favorable results in the prevention of actinic keratoses and SCC of the skin when topical sunscreens were used regularly and properly during sun exposure. In this study, people who applied broad-spectrum sunscreen with SPF value of 15+ to their sun-exposed skin (head, neck, arms, and hands) at least 3 to 4 days a week were compared with those who did not apply or applied fewer than 2 days a week. They observed a 40% reduction in SCC after 4.5 years; however, no significant benefit for BCC was demonstrated. Similarly, Van der Pols and colleagues determined a decrease in the incidence of SCC without any significant difference in the incidence of BCC after regular application of sunscreens. Moreover, Vainio and colleagues reviewed all the deliberations about the sunscreen and skin cancer that were held at the meeting of the International Agency for Research on Cancer at Lyon, France, from April 10 to 18, 2000. They declared that there was inadequate evidence that supports the preventive effect of sunscreens on the formation of BCC; on the other hand, sunscreens can reduce the development of actinic keratoses, which are a precursor of SCC. To highlight the cancer-preventive efficacy of sunscreens, large population-based, multicenter, randomized, double-blind, placebo-controlled, prospective trials are required.
The behavioral and attitudinal changes, including sunscreen application, are generally easy to perform and life saving; nevertheless, they are not widely accepted and practiced even in developed countries. In 1997, Hall and colleagues aimed to examine the sun-protection behaviors in the US population and collected data from 10,048 white citizens. They determined that only 30% seek shade, 28% wear sun-protective clothes, and 32% apply sunscreen; therefore, they concluded that sun-protective behaviors are practiced in a limited percentage of the US population. In 2011, Buller and colleagues reviewed the collected national and statewide behavioral surveys about the sun-protection behaviors in the US population. They determined that a minority of adults (30%) routinely engaged in sun-protection behaviors. In addition, a high rate of sunburning (69%) and low rate of sun-protection behaviors (40%) were detected in adolescents. Unfortunately, both of these studies demonstrate that sun-protection behaviors have not changed significantly in the past 2 decades in the US population. In addition, Stanton and colleagues investigated the efficacy and practice of primary prevention of skin cancer in Australia. This study revealed that the most commonly practiced sun-protection behavior in children, adolescents, and adults was sunscreen application. On the other hand, sun-protection clothing and attitudes were inadequate. They emphasized that public education interventions did not change people’s sun behaviors and attitudes, and the relationships between sun protection and reduction in skin cancers, and tanning/sunbathing and increase in skin cancer were poorly understood, even with the awareness of the population about the potential risks of solar UV radiation was accomplished.
Chemoprevention
Sun-protection behaviors and regular application of sunscreen are recommended as a primary prevention method; however, additional preventive interventions, such as chemoprevention, are generally required, especially for high-risk patients. Chemoprevention is a promising strategy that may provide inhibition and/or reversal of the development of skin cancer. An ideal chemopreventive agent should be safe with or without minimal toxicity and have a significant efficacy in decreasing the incidence of skin cancer. Topical and oral forms of natural, synthetic, or biologic chemical agents are used for chemoprevention. The most popular chemical agents that have proven of potential efficacy for chemoprevention are the following:
- 1.
Retinol and retinoids
- 2.
Difluoromethylornithine
- 3.
Green tea polyphenols
- 4.
Cyclo-oxygenase-2 inhibitors
- 5.
T4 endonuclease V (Dimericine)
- 6.
Photolyase
- 7.
Lycopene
- 8.
Silymarin
- 9.
Genestein
- 10.
Vitamin D
All of the chemopreventive agents mentioned may influence and inhibit the process of photocarcinogenesis in different stages ; however, retinoids and retinol are the only chemical agents that have the proven to have a chemopreventive effect of NMSCs in humans. The mechanisms that may play a role in chemopreventive properties of retinoids are inhibition of cell growth, induction of apoptosis and differentiation, modification of extracellular adhesion molecules, and protooncogenes. The Southwest Skin Cancer Prevention Study Group examined the chemopreventive effect of retinol (a daily supplementation of 25,000 IU) in moderate-risk patients in a randomized, double-blind, controlled study. They demonstrated that retinol supplementation reduces the development of SCC; however, it is not beneficial for the prevention of BCC. In a different study, they also investigated the chemopreventive effect of retinol and isotretinoin in high-risk patients. Unfortunately, no beneficial chemopreventive effect was found with retinol and isotretionin. Similarly, a long-term (approximately 12 years), randomized, double-blind, placebo-controlled clinical trial indicated that beta carotene supplementation (50 mg/d) is not beneficial for the prevention of the development of an NMSC (both BCC and SCC) among healthy well-nourished men. In addition, Greenberg and colleagues did not find a significant reduction in the development of BCC and/or SCC in patients who had a history of previous NMSC after treatment with beta carotene (50 mg/d). On the other hand, Kraemer and colleagues investigated the chemopreventive effects of retinoids in 5 patients with xeroderma pigmentosum to whom oral isotretinoin at a dosage of 2 mg/kg/d was applied for 2 years. They observed a statistically significant difference when the mean number of NMSCs before (mean: 24) and after (mean: 5) treatment were compared. Moreover, the tumor frequency increased a mean of 8.5-fold after the discontinuation of the drug. Therefore, they concluded that high-dose oral isotretinoin is a beneficial drug for the chemoprophylaxis of skin cancers in patients with xeroderma pigmentosum; however, they also emphasized that this treatment may cause some side effects, such as mucocutaneous toxicities, and liver-function and skeletal abnormalities. Therefore, chemoprevention with systemic retinoid treatment is generally recommended when the benefits overshadow the potential risks and complications, and almost always applied in conjunction with another prevention intervention for NMSC. Ultimately, Prado and colleagues reviewed the indications of retinoids for NMSC chemoprophylaxis and signified the candidates for this treatment who are
- •
Patients who had chronic immunosuppression owing to organ transplantation, lymphoma, or leukemia, or are carriers of human immunodeficiency virus
- •
Patients with psoriasis
- •
Patients who have a history of previous NMSC or photochemotherapy (PUVA) treatment
- •
Patients with radiation-induced NMSC
- •
Patients with xeroderma pigmentosum, nevoid BCC syndrome, Bazex syndrome, Rombo syndrome, or epidermodysplasia syndrome
Other agents, difluoromethylornithine, T4 endonuclease V, curcumin, and isoflavone genestein, appear safe; however, clinical trials that would establish their efficacy in human beings have not been completed yet.
Lycopene, green tea (epigallocatechin gallate), grape seed extract, and silymarin have been shown to be effective in experimental studies.
Chemical agents that have been disproved for NMSC chemoprevention are the following :
- •
Vitamin E (oral alfa-tocopherol 400 IU/d)
- •
Selenium (oral selenium 200 μg/d)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




