CHAPTER 17 No Vertical Scar Breast Reduction and Mastopexy
Summary
The ‘no vertical scar’ reduction/mastopexy is another tool which is useful to correct the large or sagging breast with a lot of ptosis. This technique can produce a pleasing breast shape and a nice areola without the areolar distortion or the visibility of a vertical scar.1–3
Key Points
Patient Selection
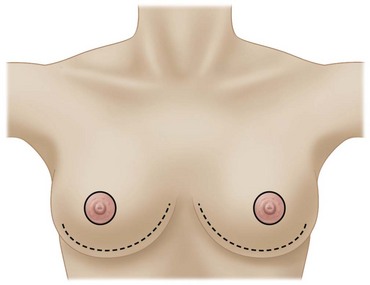
The ‘no vertical scar’ reduction/mastopexy is essentially the same reliable operation as the T scar inferior pedicle reduction except that it has one less scar: the vertical scar (see Figs 17.1–17.3). The most common cause of patient dissatisfaction after breast reduction is the scar.4 We believe that many patients can get the same nice breast shape achieved with the T scar without a vertical scar. If we can achieve good shape with one less scar than is achieved with a T scar reduction, then why not do it?
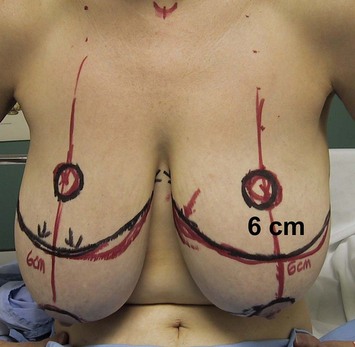
This is a good technique for a patient that has a lot of ptosis and a lot of excess skin. The ideal patient is one who has 5 or more cm of skin between the areola and the new areolar site (see Fig. 17.4).
Indications
The vertical scar reduction has the least amount of skin removal of the three techniques. We therefore prefer the medial pedicle vertical reduction/mastopexy5 for the patient who does not have very much skin to excise, and who does not have a great deal of ptosis (less than 5 cm of skin between the areola and the new areolar site). This is about 25% of the patients in our practice.
The ‘no vertical scar’ technique can be used for either reduction or mastopexy.1–3
The medial pedicle rotation advancement vertical scar operation (rotation of the medial pedicle superiorly and advancement of the lateral pillar beneath it) may give more projection than the T scar or ‘no vertical scar’ techniques. However breast shaping sutures do augment the projection obtained with the ‘no vertical scar’ and the T scar techniques.1
Operative Technique
The Plastic Surgery Video Archive has an excellent film showing preoperative markings and intraoperative technique.6
Preoperative preparation
Markings
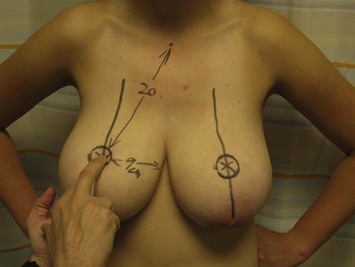
A line is drawn down the center of the breast meridian line where the areola will look best (see Fig. 17.4). If a large part of the lateral breast is to be removed, the nipple–areola axis line can be moved medially as will be appropriate to the final anticipated breast width. The axis of the breast is drawn as a continued straight line below the inframammary fold by keeping it as a straight line seen through two fingers holding up the breast mound (see Fig. 17.5).
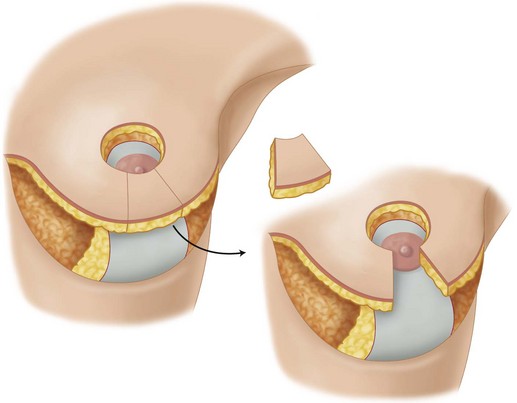
A finger on the breast is used to palpate another finger through the breast at the level of the inframammary fold, and this becomes the new nipple site (Fig. 17.4). The areolar recipient site skin excision is marked on the skin brassiere preoperatively with the patient sitting. It is drawn as a slightly horizontal oval (3.5 cm diameter horizontally, and 3.0 cm diameter vertically) as the oval will stretch to a circle when the skin brassiere flap is pulled down over the breast to the inframammary fold at the time of final closure. The areola is marked as a 4 cm diameter circle also with the patient sitting up. The area of the areolar recipient circle is deliberately marked to be a little smaller than the areola itself in order to achieve a tension free closure in the periareolar scar. The areolar recipient site is also marked smaller than the areola itself when the author uses the T scar or the vertical scar techniques.
A tension free areolar scar means a better appearing areolar scar. This scar is the most visible scar of the reduced breast (see Fig. 17.6). The areolar scar is the scar that the woman sees every day when she is naked. It is the showcase scar of the breast and should be treated as we treat the preauricular scar of the facelift; tension free and closed with care.

Fig. 17.6 Postoperatively ‘no vertical scar’ breast reduction with typical pleasing periareolar scar. The areolar opening is designed to have a slightly smaller diameter than the areola to avoid tension. There is no distortion of the inferior periareolar scar by a vertical scar, and no vertical scar on the visible breast mound. The inframammary scar is hidden in the inframammary fold below the breast mound. This is the same patient seen in Figure 17.14.
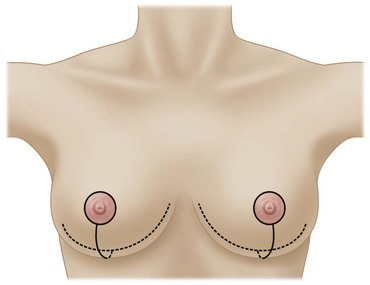
To avoid visible medial dog ears in the no vertical and T scar techniques, the medial end of the inframammary fold incision is marked to be hidden under the medial fold of the breast so that it will not be visible postoperatively (see Fig. 17.7). The lateral end of the inframammary fold incision is drawn 1 cm medial to its preoperative position because the smaller postoperative breast inframammary fold has moved medially. If the patient is overweight and has a lateral chest fat fold, the lateral scar should be kept in this fat fold crease to decrease its visibility.
After the marking of the inframammary fold incision, the lower incision of the skin brassiere flap is marked on the breast mound. The center of this incision is marked at 5–6 cm below the lower border of the areola recipient site. Nice smooth curves are then drawn from this point medially to reach the medial inframammary fold incision mark (see Fig. 17.8), and then laterally to reach the lateral inframammary incision mark.