Fig. 38.1
Tattoo machine (needle assembly)
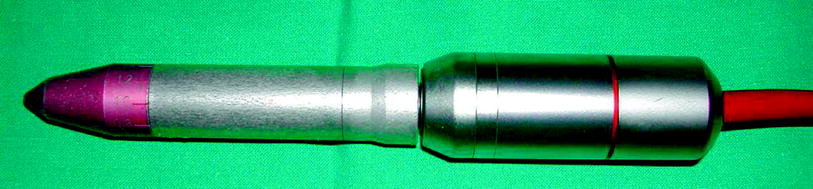
Fig. 38.2
Tattoo machine
Permanent and semipermanent sterile pigments are available, and they can be mixed together to achieve the desired tone. The selected color is typically one or two shadows darker than the native areola because the color tends to fade and discolor with time. The needles are dipped into the pigment and are applied in a radial and circular pattern.
Postoperative care of tattooing includes a dressing with non adhesive paraffin gauzes or fatty gauzes. The patient may remove her dressing after 1 week/10 days and shower. She is instructed to remove the dressing carefully and not to peel off scabs because this will remove the tattoo pigment. Use of sunscreens for 6 months after tattooing is suggested.
38.4.2 The Reconstruction of the Nipple
Different methods have been described for the reconstruction of the nipple, including the use of external prostheses, simple tattooing, and surgical reconstruction. Nowadays, the use of external prostheses has been abandoned completely because glue adhesion problems and allergy have been described [7–9]. Tattooing alone gives no projection and therefore gives unsatisfactory results. Surgical reconstruction is the most used method and involves the use of grafts or local flaps.
38.4.2.1 The Grafts
If the nipple of the contralateral breast is large enough, the method of choice is “nipple sharing,” which transfers part the opposite healthy nipple to the reconstructed breast. It is ideal in color and bulk, but it can be employed satisfactorily only when the native nipple is large. Sharing can be performed by “decapitation” (Fig. 38.3a). The decapitation method can also be performed with “starred resection” (Fig. 38.4b). Another possible method of harvesting the nipple is “vertical bipartition”, which is especially indicated if the diameter of the nipple exceeds its height. In all cases, the donor nipple is directly closed with a simple suture (Fig. 38.3b).
Fig. 38.3
Nipple sharing a decapitation, b vertical bipartition
Fig. 38.4
Nipple sharing (starred resection)
The perfect tissue matching with regard to color and texture between the two nipples is the main advantage of nipple grafting [10–13]. The disadvantages include the fact that any composite graft has an inherent risk of incomplete revascularization, which can lead to loss of tissue and projection. Structural distortion and lack of sensation of the nipple are also found as less frequent complications [14].
If patients are reluctant to disturb the healthy opposite nipple or if the native nipple is not large enough, other possible donor sites of composite grafts are the toe pulp and auricular tissue [15–18]. In both areas, there is a skeletal part similar to the fibrofatty nipple tissue but the color is much lighter. Even the skin graft from the labia minora was used in the past, but its use has been completely abandoned owing to the morbidity of the donor site and the very satisfactory result from the surgical reconstruction [19].
Cartilage graft is also harvested to obtain the projection of the nipple [20]. It can be positioned under a skin graft in the same surgical setting or afterward. However, the survival of the skin graft overlying cartilage cannot be secured and the ongoing skin graft contraction can gradually minimize the projection of the cartilage graft [21, 22].
38.4.2.2 The Local Flaps
More frequently, the nipple is reconstructed with local flaps. Different techniques have been described, but for all of them at least 50 % loss of the nipple projection has been observed within 1 year after surgery. For this reason, the new nipple should be planned to be larger and project more than the expected end point [23–33].
The flattening of the reconstructed nipple is due to the lack of the natural anatomical infrastructure of the normal nipple as well as the existence of centrifugal forces on the superficial surfaces on the reconstructed eminence. Projection is also influenced by local tissue characteristics, such as the thickness of the dermis and the amount of local scarring. Nipples created over previous scar have minimal loss of projection, whereas those created on an individual with a tightly expanded breast mound and a thin dermis lose the most projection.
Nipple reconstruction with local flaps depends on the local availability of soft tissue to achieve nipples of the desired size. Previous local scars (such as mastectomy and central quadrant scars) influence flap design and may interfere with flap vascularization.
The surgical techniques can be divided into two main groups: the “pull up techniques” [34–36], based on deep dermal and adipose flaps, and the “traction techniques” [37–39], based on a local skin advancement flap.
Pull-up techniques based on a central subcutaneous core require a deep dermal and adipose tissue dissection. They produce an irreducible hernia of the central core local flaps. They are preferably applicable to breast reconstruction using autologous tissue. For breast mounds with a thin subcutaneous layer, as commonly associated with the implanted breast, local flaps using a central subcutaneous core can be strongly advocated. The tripod flap, the mushroom flap, the Maltese cross flap, the quadrapod flap, and the H flap also belong to “pull up techniques”.
The double-opposing tabs, the Bell-flap, and the star flap belong to the “traction techniques” based on subdermal pedicled flaps.
38.4.2.3 The Quadrapod Flap
This is one of the central subcutaneous core pedicle techniques previously described by DiPirro [41] and later modified by Little [40]. After the position of the nipple and the diameter of the areola have been planned, four opposing skin flaps are dissected with preservation of the central fat core (Fig. 38.5). The radial length of the flap is according to the new nipple height projection. The dissection starts from the outer part toward the central core. The central fat core is then raised and covered by the four opposing flaps. However, the color of the new nipple does not match that of the contralateral one, so secondary tattooing is needed and the surrounding areolar area must be grafted. Despite the promising immediate result, there is still a loss of projection later.
Fig. 38.5
The Quadrapod Flap
38.4.2.4 The H flap
This has been described by Hallock and Altobelli [42] as a cylindrical nipple reconstruction with the similar principle of a central subcutaneous core pedicle technique. The design is based on maintaining the central core projection by wrapping with counteracting cylindrical flaps. The flap is designed with diameter the same as that of the areola. The lateral rectangular shape is designed as the “H” shape (Fig. 38.6). The width of each leg is according to the designed new nipple projection and the length of each side is matched to half the circumference of the new nipple. If there is scar present in the area, the flap can be designed in a different direction. The dissection is performed by preserving subdermal vessels. However, the long-term result is still disappointing because of scar contracture and the need for secondary nipple tattooing and grafting for areola reconstruction.
Fig. 38.6
The H flap
38.4.2.5 The Modified Star Flap
The modified star flap belongs to second group of flaps, based on the subdermal plexus, and it is very frequently used [43]. The flap can be based superiorly, laterally, or inferiorly as local scarring dictates, although a more natural projection and appearance for the patient are obtained by basing the flap superiorly. The “wings” of the flap will determine the nipple height (Fig. 38.7). The height should be bigger than the ultimate desired height, allowing a decrease in projection over time. The nipple flap is tattooed prior to flap elevation. The wings are raised containing dermis and subcutaneous fat, getting thicker toward the base. The donor incisions are closed directly around the base of the nipple. The wings are wrapped together, one wing being placed at the base of the nipple and one partially overlapping. Afterward, the areola diameter is remarked and the areola is tattooed. The commonest problem is the variable loss of projection of the nipple over time.
Fig. 38.7
The Modified Star Flap
38.4.2.6 The Modified Arrow Flap with Immediate Tattooing: Author’s Experiences
From the previous technique of Rubino et al. [45], we agree with the principles that nipple projection and volume are obtained by increasing the amount of dermis within the flap without enclosing any excess subcutaneous fat [ 43–45]. The dissection of the flap can be performed effectively with the preservation of the dermal plexus. However, the necessity of skin grafting is a drawback of the original technique. Therefore, we suggest immediate tattooing simultaneously with the arrow flap procedure.
The flap can be designed in any position—superior, inferior, lateral, or medial—depending on the previous scar, if one exists. The width of the flap wing is matched to the new projection of the nipple. We recommend designing it wider because the flap will shrink in 6 months. Pretattooing is recommended before flap harvesting. Finally, additional tattooing is required to adjust the shape of the areola to that of contralateral healthy one. We experienced no increased rate of local complications by combing the two procedures.
The advantages of pretattooing are
The reconstructed nipple has pigmentation that is more similar to that of the areola and it is not lighter than the native nipple.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








