ANATOMY OF PERIPHERAL NERVES 
 What are the basic elements of the peripheral nerves?
What are the basic elements of the peripheral nerves?
Internal epineurium
External epineurium
Perineurium
Endoneurium
 What are the functions of the internal and external epineurium?
What are the functions of the internal and external epineurium?
The external epineurium surrounds the entire nerve and the internal epineurium surrounds groups of fascicles.
 Which layer is an extension of the blood–brain barrier?
Which layer is an extension of the blood–brain barrier?
The perineurium. This layer has closely packed cells and surrounds individual fascicle that functions to block the spread of infection and to maintain a positive intrafascicular pressure.
 The layer that surrounds individual axons is termed?
The layer that surrounds individual axons is termed?
The endoneurium.
 What is a fascicular plexus?
What is a fascicular plexus?
A region of interconnections between fascicles.
 Name three blood supply sources for peripheral nerves.
Name three blood supply sources for peripheral nerves.
1. Arteriae nervosum (vaso nervosus) (epineurium)
2. Extrinsic blood vessels (perineurium)
3. Capillary plexus (endoneurium)
 How is the nerve potential propagated down the nerve?
How is the nerve potential propagated down the nerve?
Depolarizing current achieving the threshold membrane potential leads to activation of voltage-gated sodium channels.
 What is a node of Ranvier?
What is a node of Ranvier?
A gap that represents a space between adjacent Schwann cells along the length of the axon.
 What is saltatory conduction?
What is saltatory conduction?
Propagation of the action potential via depolarization at the nodes of Ranvier (myelinated fibers 3–150 m/s).
 What is Wallerian degeneration?
What is Wallerian degeneration?
A process by which axoplasm and myelin are degraded and removed by phagocytosis.
 What are the key features of Wallerian degeneration?
What are the key features of Wallerian degeneration?
1. Granular disintegration of axoplasmic microtubules and neurofilaments.
2. Disappearance of myelin sheath and axons distal to a nerve lesion.
3. Loss of neural conductance within 48 to 96 hours.
4. Axonotmesis (Sunderland second degree).
 After laceration or injury to the nerve, Wallerian degeneration occurs in which segment?
After laceration or injury to the nerve, Wallerian degeneration occurs in which segment?
Distal segment.
 What are the bands of Büngner?
What are the bands of Büngner?
Collapsed columns of Schwann cells in the distal segment of a complete nerve injury.
 What is neurotrophism?
What is neurotrophism?
The ability of appropriate distal receptors to enhance the maturation of nerve fibers, which includes the production of a gradient of diffusible substances that direct axonal growth during regeneration.
 NERVE REPAIR CLASSIFICATION AND ASSESSMENT
NERVE REPAIR CLASSIFICATION AND ASSESSMENT 
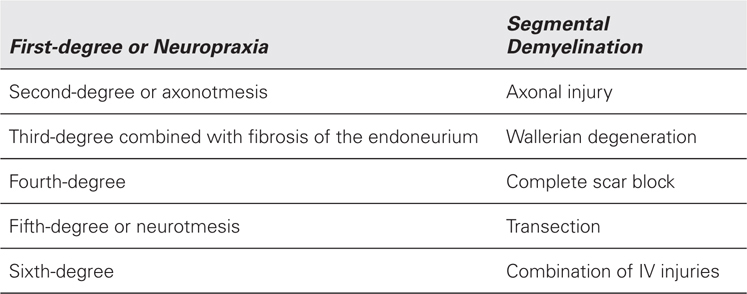
 How are nerve injuries classified (Sunderland based)?
How are nerve injuries classified (Sunderland based)?
 How is fibrosis resulting from nerve injuries classified (Millesi)?
How is fibrosis resulting from nerve injuries classified (Millesi)?
Type I: fibrosis of the epineurium
Type II: interfascicular fibrosis
Type III: intrafascicular fibrosis
 Which types of injuries can be expected to have complete recovery?
Which types of injuries can be expected to have complete recovery?
Neuropraxia and axonotmesis.
 Nerve fiber regeneration occurs at what rate?
Nerve fiber regeneration occurs at what rate?
1 mm/day or 1 in/month.
 What are clinical measurements of motor nerve injury?
What are clinical measurements of motor nerve injury?
Weakness, loss of function, and atrophy.
 What are clinical measurements of sensory nerve injury?
What are clinical measurements of sensory nerve injury?
Moving and static two-point discrimination for innervation density and number of fibers.
Semmes–Weinstein monofilaments and vibration instruments as threshold tests for performance levels.
 Describe and classify the six levels of motor recovery following motor nerve injury.
Describe and classify the six levels of motor recovery following motor nerve injury.
M0: no contraction
M1: contraction in proximal muscles
M2: contraction in distal muscles
M3: contraction sufficient to resist gravity
M4: contraction against strong resistance
M5: return to full muscle strength
 Describe and classify the six levels of sensory recovery following sensory nerve injury.
Describe and classify the six levels of sensory recovery following sensory nerve injury.
S0: absence of sensibility
S1: deep-pain sensibility
S2: superficial sensibility
S3: full recovery of pain and touch (moving 2PD >15 mm)
S3+: localization of stimulus (moving and static 2PD 7–15 mm)
S4: complete recovery (2PD 3–6 mm)
 What does an “advancing Tinel sign” after nerve injury signify?
What does an “advancing Tinel sign” after nerve injury signify?
Effect of triggered electric-current–like pain represents outgrowing axon sprout ends.
 What is the most sensitive test for eliciting nerve compression syndromes with demyelination?
What is the most sensitive test for eliciting nerve compression syndromes with demyelination?
Nerve conduction velocity (NCV) tests.
 What is the most helpful test for eliciting a denervation with axonal loss?
What is the most helpful test for eliciting a denervation with axonal loss?
Electromyography (EMG)
 What is the earliest that EM studies will be helpful to evaluate a patient for a suspected peripheral nerve injury?
What is the earliest that EM studies will be helpful to evaluate a patient for a suspected peripheral nerve injury?
3 weeks.
 Which imaging study is helpful in diagnosing injuries to peripheral nerves?
Which imaging study is helpful in diagnosing injuries to peripheral nerves?
Magnetic resonance imaging (MRI) neurograms.
 Which test is useful in helping to distinguish proximal and distal injuries?
Which test is useful in helping to distinguish proximal and distal injuries?
Somatosensory evoked potentials (SSEP).
 What are the normal values for static and moving two-point discrimination?
What are the normal values for static and moving two-point discrimination?
1. Static 2PD: up to 6 mm
2. Moving 2PD: 2 to 3 mm
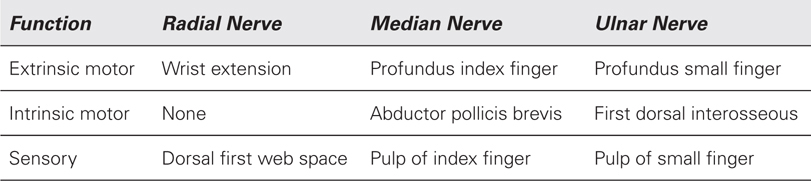
 Clinical tests for nerve function
Clinical tests for nerve function
 TREATMENT OF NERVE INJURIES
TREATMENT OF NERVE INJURIES 
 What repair method is used when a nerve is partially transected and landmarks are preserved?
What repair method is used when a nerve is partially transected and landmarks are preserved?
Epineural repair.
 What repair method is generally used when a nerve injury includes a crushing component?
What repair method is generally used when a nerve injury includes a crushing component?
Group fascicular repair.
 What repair method is generally used when there is a delayed repair requiring trimming of the nerve ends?
What repair method is generally used when there is a delayed repair requiring trimming of the nerve ends?
Group fascicular repair.
 In an acute crush injury setting with evidence of transection and contusion of a peripheral nerve, what is the recommended treatment?
In an acute crush injury setting with evidence of transection and contusion of a peripheral nerve, what is the recommended treatment?
Tagging the proximal and distal nerve endings followed by delayed repair after 3 weeks or until the wound permits.
 What is the advantage of early secondary nerve repair?
What is the advantage of early secondary nerve repair?
Allows for terminated scar reaction along the nerve which the surgeon can estimate and graft.
 Have clinical studies demonstrated that fascicular repair is superior to epineural repair?
Have clinical studies demonstrated that fascicular repair is superior to epineural repair?
No.
 Nerve elongation in secondary nerve repairs can provide how much additional length?
Nerve elongation in secondary nerve repairs can provide how much additional length?
Approximately 10%.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


