CHAPTER 8 Muscle-Sparing and Free TRAM Flap Breast Reconstruction
Summary/Key Points
Introduction
Breast reconstruction with autologous tissue can generally achieve more durable and natural results than with the use of implants alone.1 When well designed and executed, the TRAM flap offers the advantage of being able to provide large soft tissue volume. In large breasted women undergoing unilateral reconstruction, this technique offers improved aesthetics over implant reconstruction (Fig. 8.1). In addition, complete restoration of the breast mound is often possible in a single stage. Of all the available donor sites for autologous breast reconstruction, the TRAM flap in both pedicled and free form is the most frequently used method.2 The evolution of the TRAM flap, from pedicled, to free TRAM, to muscle-sparing (MS) free TRAM, to perforator flap (DIEP) has occurred in an attempt to reduce the morbidity that results from the loss of the rectus muscle and anterior sheath associated with the pedicled TRAM flap.
The free TRAM flap is based upon the dominant deep inferior epigastric vascular pedicle which permits transfer of a larger volume of abdominal tissue than with the use of pedicled TRAM flaps. The muscle-sparing TRAM flap is a modification of the free TRAM flap which limits the amount of rectus muscle and anterior sheath harvested to only those encompassing the medial and lateral rows of musculocutaneous perforating vessels. The theoretical advantage of the muscle-sparing TRAM is the ability to minimize the violation of the abdominal wall integrity while ensuring equal blood supply to the flap as compared to a free TRAM flap. A more comprehensive understanding of the evolution of the MS TRAM to the DIEP flap is reflected in the classification of muscle-sparing TRAM described by Nahabedien3 (Table 8.1). The DIEP flap is the most refined form of MS TRAM in which no muscle or anterior rectus fascia is harvested with the abdominal flap.
Table 8.1 Classification of MS free TRAM
| Muscle-sparing technique | Definition (rectus abdominis) |
|---|---|
| MS0 | Full width, partial length harvested |
| MS1 | Preservation of lateral segment |
| MS2 | Preservation of medial and lateral segments |
| MS3 (DIEP) | Preservation of entire muscle |
From Nahabedian MY, Momen B, Galdino G, Manson PN. Breast reconstruction with the free TRAM or DIEP flap: patient selection, choice of flap, and outcome. Plast Reconstr Surg 2002;110(2):466.
Indications and Contraindications
Indications
A free or MS TRAM represents an excellent reconstructive option for women undergoing either immediate or delayed breast reconstruction who possess an adequate amount of abdominal fat to achieve the desired breast volume. Moreover, free TRAM or MS TRAM flaps are preferred over pedicled TRAM flaps in the immediate breast reconstruction setting because there is less risk of fat necrosis or partial flap loss in the breast flap. The more dominant blood supply to the free TRAM or MS TRAM can help minimize the problems with wound healing that can lead to delays in the delivery of adjuvant therapy as seen with pedicled TRAMs.4 While obesity and tobacco smoking are two relative contraindications to performing a pedicled TRAM flap, in these high risk patients who either require or strongly desire autologous tissue reconstruction, they generally have a lower complication rate in both the breast and abdomen following a free TRAM or MS TRAM flap.2,4 This is felt to be due to a more robust blood supply to the breast and less surgical insult to the abdominal wall integrity. Lastly, in a large-breasted patient who does not desire a reduction on the contralateral side, a free TRAM or MS TRAM will more reliably transfer a large amount of abdominal tissue onto the chest wall than a pedicled TRAM flap (Box 8.1).
Contraindications
Absolute contraindications to free TRAM or MS TRAM include:
Abdominal incisions that should arouse suspicion include those used for inguinal hernia repair and paramedian scars. Conversely, common scars that generally do not preclude the use of free TRAM flaps are lower transverse incisions such as a Pfannensteil incision or midline incisions. The potential lack of recipient vessels should be suspected in patients with both a heavily dissected axilla and radiation to both the chest wall and axilla. Other relative contraindications to free TRAM flaps include patients who are medically unfit, patients with a grave prognosis, and previous liposuction to the abdomen (Box 8.1).
Patient Selection
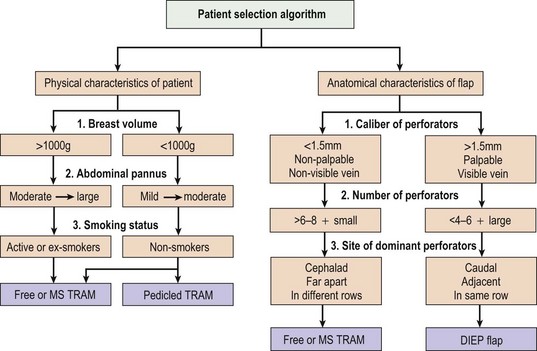
The choice of which technique of TRAM flap to use is based on the physical characteristics of the patient assessed both preoperative and intraoperatively. An algorithm to aid the decision-making process is outlined in Figure 8.2. Generally, whether the patient is a good candidate for pedicled versus free TRAM can be determined preoperatively based on the physical examination. On the other hand, the decision to use a free TRAM or MS TRAM or DIEP flap is made intraoperatively based on individual anatomical variations.
The role of rectus abdominis muscle within the abdominal flap is to carry and protect the epigastric vascular system.5 The muscle itself is not felt to contribute to volume, shape, or vascularity of the reconstructed breast. MS TRAM minimizes the amount of rectus abdominis muscle and anterior rectus sheath harvested, and thus lessens the insult to the abdominal wall. Though comparative studies examining the incidence of hernias and bulges following pedicled TRAM, free TRAM, and DIEP flaps have shown mixed results, evaluations of abdominal strength have demonstrated that free TRAM is superior to pedicled TRAM, and DIEP flap may be further superior to the free TRAM.6–9 More recently, Nahabedian et al observed a significantly higher incidence of lower abdominal bulges in bilateral breast reconstruction in the non-muscle-sparing than muscle-sparing group.5
The patient characteristics noted preoperatively are as follows:
The anatomical flap characteristics noted intraoperatively are as follows:
Operative Technique
Breast marking
For a patient undergoing skin-sparing mastectomy with a small or moderate sized breast, a simple elliptical or circular excision is marked over the central mound of the breast which includes the nipple–areolar complex (NAC). This allows closure of the reconstructed TRAM flap skin to the mastectomy skin either in an elliptical pattern or as a circular purse-string pattern to create a template for the future NAC (Figs 8.3 and 8.4). For a patient with large breasts or breasts with grade III ptosis, a Wise type pattern skin reduction can be used in the involved breast (Fig. 8.5). For patients with existing grade II ptosis in the involved breast who wish a future mastopexy on the opposite breast, a vertical mastopexy skin excision pattern can be applied.
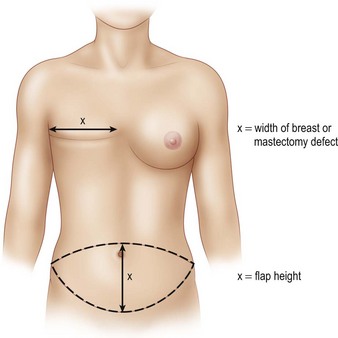
Abdominal marking
The transverse skin island of the TRAM flap is marked over the lower abdomen encompassing the lower abdominal redundant soft tissues. The superior incision lies just above the level of the umbilicus in order to capture as many periumbilical perforators as possible into the flap (Fig. 8.6). Ideally, the height of the abdominal flap should be equal or greater than the breast width of the mastectomy specimen (Fig. 8.7). This is because during the flap inset, the TRAM flap is inset vertically on the chest as to create the most natural ptotic shape for the reconstructed breast. In designing the inferior incision, care is taken to mark it at a location such that the abdomen can be closed with minimal tension. As well, the inferior incision is designed such that it is hidden in the natural suprapubic crease to camouflage its appearance. Lastly, the inferior incision should not be within the pubic hair-bearing region, as this may lead to problems with delayed wound healing. A midline mark is made just above the umbilicus and on the pubic region. These marks help place the midline of the upper abdominal flap to the midline of the pubic area when closing the abdominal donor site.