8. Multimodal Analgesia for the Aesthetic Surgery Patient
Girish P. Joshi, Jeffrey E. Janis
UNDERSTANDING MULTIMODAL PAIN MANAGEMENT
■ “Prescription drug overdose is an epidemic in the United States. All too often, in far too many communities, the treatment is becoming the problem.”1
■ 80% of patients experience acute pain after surgery.
■ 75% of U.S. patients report surgical pain rated 7 or higher (scale of 1–10).
■ 59% of patients are concerned about postoperative pain.2
OPIOID EPIDEMIC
■ November 2016: U.S. Surgeon General declares epidemic of addiction—public health crisis3
■ United States contains 4.6% of the world’s total population, but consumes two thirds of the world opioid supply.
■ 12.5 million people, or 4.7% of the American population, aberrantly used prescription opioids in 2015.4
■ 1% of the U.S. population is addicted to opioids.
■ 2015: 28,647 people died in the United States due to prescription opioid overdose
■ Prescription opioid use disorder is estimated to cost the American economy $53.4 billion per year.
■ Resurgence of heroin
• Cheaper
• Inappropriate weaning strategies from prescription opioids
■ Four fifths of heroin users report their initial exposure to opioids was to prescription opioids.5
■ 2007: Prescription opioid overdose responsible for more deaths than heroin and cocaine combined 6
■ 1996–2006: Rate of prescription opioid use disorder increased by 167%7
• Rates continued to rise
PRESCRIBING PATTERNS AND DEATHS
■ In patients with opioid prescriptions that overdose, the mortality rate increases with escalating dose.8
■ Increases in opioid prescription rates have not resulted in improvement in patient disability or health outcome.9
STATISTICS
■ Accidental deaths per year in United States10:
• #1: Drug poisoning
► 40% of drug poisonings are due to opioid overdose.
• #2: Automobile accidents
• 2015: United States—5.4% of high school seniors aberrantly used prescription opioids within the last year11
► 40% stated that these drugs were easy to get.
• 2016: Canada—20.6% of grade 12 high school students aberrantly used opioid medication in the last year12
► 70% obtained the medication from their own homes.
• 44 Americans die every day of a prescription overdose.13
► For every death there are:
♦ 10 treatment admissions for abuse
♦ 32 Emergency Department visits for misuse or abuse
♦ 130 people who abuse or are dependent
♦ 825 nonmedical users
DIVERSION
■ Illicitly obtained prescription opioids are often obtained from friends or family.
■ 2006–2010: Street availability of prescription opioids increased
■ 2010: 40% of Medicaid patients with opioid prescriptions had indicators of aberrant use or diversion14
SURGEON’S ROLE
■ Surgeons responsible for 9.8% of the total opioid prescriptions in the United States15
■ Rates of opioid prescriptions to opioid naive patients after minor surgery increased between 2004 –2012.16
■ Surgeons may play a significant role in propagating the addiction crisis by exposing patients to potentially harmful and addictive opioid medications and contributing to the street supply of opioids.
■ Simple education interventions for patients to explain how to safely store and dispose of opioid medications can make a significant impact.
■ Led by the surgeon and a written handout or referral to a website which explains proper opioid storage and disposal
PROPER STORAGE AND DISPOSAL
■ Opioids should be stored in a locked cabinet.
■ All unused medication should be returned to the pharmacy or destroyed once postoperative pain has resolved.
SURGERY AND ADDICTION
■ Patients who were opioid naive before surgery shown to have a significant chance of persistent postoperative opioid use.17
■ Many patients continue to receive opioids chronically after initially receiving them for postoperative pain control.
■ Patients taking opioids chronically prior to surgery have an increased chance of still taking them 1 year later when compared with controls.
OPIOIDS AND SURGERY
■ A 2016 study of elective hand surgery patients showed 13% were still taking opioids 90 days after surgery.18
■ Another study found that 3.1% were still taking opioids at 90 days after major surgery.19
■ Total knee arthroplasty: 1.4% chance of still taking opioids one year after surgery20
• Odds ratio of 5:1 when compared to nonoperated controls
• Another study found that older patients (>66 years old) following low-risk surgery have a 44% increased likelihood of chronic use at 1 year compared with controls.21
CAUTION: Surgery is a risk factor! There is a risk of persistent opioid use following exposure to opioid medications in the perioperative period, even in opioid naive patients.
RISK FACTORS FOR OPIOID ABUSE
■ History of substance use disorder
■ Comorbid psychological health conditions (i.e., anxiety, depression)
■ Male sex
■ Low socioeconomic status
LEFTOVERS AND DISPOSAL
■ Elective hand surgery study (2012): 95% received opioids with average 30 doses22
■ 19 doses left over after acute pain resolution
■ Urology: 92% received no instructions on how to dispose of leftover opioids after surgery23
• 67% had leftover opioids
• 91% of the patients with leftovers went on to keep them in an unlocked medicine cabinet24
■ Oral surgery and pediatric surgery: similar to above
■ Thoracic and gynecological surgery: 83% had leftover opioid medication
► 71%–73% stored the leftovers unsafely
SENIOR AUTHOR TIP: Since most people with prescription opioid use disorder get them from friends and family, it is reasonable to conclude that our postoperative analgesia prescription practices are making a significant contribution to the supply of illicit opioids.
RECOMMENDATIONS FOR SURGEONS
■ Consider the risk that an individual patient may develop persistent opioid use and proceed to an opioid use disorder.
■ Consider the risk that medications prescribed postoperatively may end up diverted to nonmedical use and causing direct public health harm.
■ Identify risk factors:
• Psychiatric illness
• History of either aberrant substance use or diagnosed substance use disorder
• Communicate to the patient in a nonjudgmental way so that they can exercise caution in taking prescribed medications.
■ Patients with an established or suspected substance use disorder should be referred to an addiction specialist preoperatively if possible.25
■ Elective surgery in patients with established substance use disorders should not be performed until follow-up for substance use has been arranged.
■ Efforts should be made to explain and facilitate the use of nonopioid pain control.
■ Prescriptions should be limited to 20 doses of low potency, immediate release opioids unless circumstances clearly dictate otherwise.26,27
SENIOR AUTHOR TIP: We can make a major contribution by curbing opioid diversion in the perioperative period. We can partner with our anesthesia/pain colleagues to identify at-risk patients and prevent postoperative aberrant opioid use.
CAUTION: If an opioid naive patient develops an opioid use disorder after surgery, that is a surgical complication. Similarly, if members of our patient’s family (i.e., children, home care workers, etc.) aberrantly use the medications we prescribe, we hold a level of responsibility for this.
PROPER PAIN MANAGEMENT
Multiple organizations have urged a shift toward nonopioid options for pain management.
■ JCAHO27:
• “An individualized, multimodal treatment plan should be used to manage pain—upon assessment, the best approach may be to start with a non-narcotic”1
■ CDC28:
• “Health care providers should only use opioids in carefully screened and monitored patients when non-opioid treatments are insufficient to manage pain”2
■ ASA29:
• “A multimodal approach to pain management beginning with a local anesthetic where appropriate”3
IMPACT OF INADEQUATE PAIN MANAGEMENT30
■ Undesirable physiologic and immunologic effects
■ Associated with poor surgical outcomes
■ ↑ probability of hospital readmission
■ ↑ cost of care
■ ↓ patient satisfaction
■ Postsurgical pain intensity was associated with delayed wound healing.
APPROACH TO PAIN MANAGEMENT
■ Common pain management protocols are opioid based.
■ Lack understanding of current literature
■ Don’t differentiate between acute and chronic pain
■ Aren’t customized to patients or surgical procedures
OPIOID-RELATED ADVERSE EVENTS31
■ Primary component of most postoperative multimodal pain management strategies
■ Associated with unwanted and severe adverse events
• Nausea and vomiting
• Pruritus
• Sedation and cognitive impairment
• Urinary depression
• Sleep disturbances
• Respiratory depression
ANALGESIC OPTIONS FOR MULTIMODAL ANALGESIA
■ Regional analgesic techniques
• Wound infiltration
• Field blocks (TAP block)
• Peripheral nerve and plexus blocks
• Neuraxial blocks
■ IV lidocaine infusion
■ Acetaminophen
■ NSAIDs
■ COX-2 inhibitors
■ Dexamethasone
■ Ketamine
■ Gabapentin/pregabalin
■ Opioids (as rescue)
BENEFITS32,33
■ Improve postsurgical pain control
■ Permit use of lower analgesic doses
■ Reduce dependence on opioids for postsurgical pain management
■ Combines a variety of analgesic medication and techniques with nonpharmacological interventions34
• Uses drugs with complimentary mechanisms of action
• Targets multiple sites of the nociceptive pathway
• Allows for lower doses of medications and potentially provides greater pain relief
■ May result in fewer analgesic side effects
■ May address patient differences in analgesic metabolism and pain sensitivity
■ Avoid “shotgun” approach
■ Type and number of analgesics should be procedure- and patient-specific
■ Emphasis on function NOT pain scores
ACETAMINOPHEN, NSAIDs, AND COX-2 INHIBITORS COMBINATION
■ Meta-analysis of opioid-sparing effects of acetaminophen, NSAIDs, and COX-2 inhibitors
■ All analgesics resulted in lower 24-hour morphine requirement (6–10 mg).
■ No clinically significant advantages shown for one group over the others
■ NSAIDs associated with more bleeding
• NSAIDs versus Coxibs
► No difference in analgesic efficacy between nonselective-NSAIDs and COX-2 selective inhibitors at equipotent doses
► COX-2 inhibitors lack of platelet inhibition and do not influence perioperative blood loss
► No difference in other adverse effects (cardiovascular, renal, gastrointestinal)
PERIOPERATIVE DEXAMETHASONE AND PAIN
■ Systematic review of published literature that involved 45 studies, involving 5796 patients
■ Benefits (as per systematic review):
• Reduced pain scores at 2 hours and 24 hours postoperatively
• Reduced opioid requirements
• Reduced need for rescue analgesia for intolerable pain
• Allowed longer time to first rescue analgesic
• Allowed shorter PACU stay
■ No increase in infection or delayed wound healing
■ No dose response with regards opioid sparing
GABAPENTIN/PREGABALIN FOR POSTOPERATIVE PAIN35,36
■ Reduces postoperative pain and opioid requirements
■ Limitations: Studies have small sample size and short duration of follow-up
■ Side effects: Sedation, dizziness may delay discharge home
■ Selective use in surgical procedures with high incidence of persistent postoperative pain
• Patients with fibromyalgia, chronic pain
INTRAVENOUS KETAMINE
■ Systematic review placebo-controlled, RCTs (n = 47) IV ketamine (bolus or infusion)
■ Heterogeneity among studies was significant
■ Reduced total opioid consumption and increase in time to first analgesic observed in all studies
■ Reduced pain scores
■ Reduced PONV only when pain scores decreased
■ Not beneficial for surgery with mild pain (VAS <4)
■ Hallucinations and nightmares significantly high when ketamine was efficacious
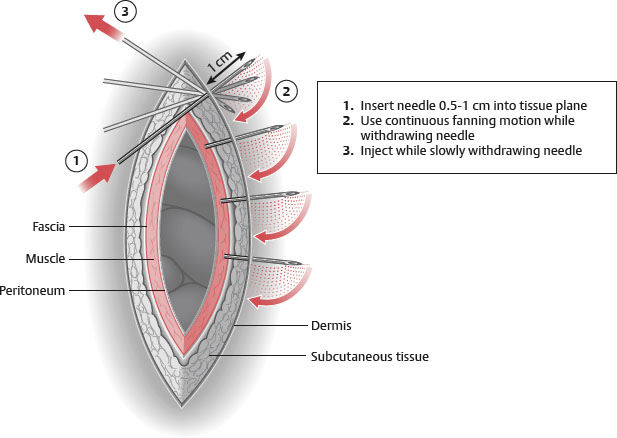
INFILTRATION OF LOCAL ANESTHETICS
TIMING
■ Timing of the block (preincision versus postincision) does not appear to be clinically significant.
■ Nerve blocks improve postoperative analgesia.
■ Total dose, but not volume and concentration, of local anesthetics affects the efficiency.