Eyebrow and upper eyelid aging occurs in all tissue planes, and manifests most commonly in skin quality, tissue volume loss (soft tissue and bone), and tissue descent. All these involutional changes are amenable to less-invasive (nonsurgical) interventions with natural and aesthetically pleasing results. It is critical for aesthetic facial surgeons to familiarize themselves with these procedures because they are in high demand by patients. This article outlines current concepts of nonsurgical management options for brow and upper eyelid aging. The anatomy and age-related changes in these structures are reviewed, and minimally invasive techniques to address these changes are detailed.
Key points
- •
Aging of the brow and upper eyelid occurs in all tissue planes and involves cutaneous changes, volume loss, and tissue descent.
- •
Volume restoration and neuromodulation have become an integral part of eyebrow/eyelid aesthetic rejuvenation.
- •
Surgical lifting techniques alone, without addressing volume loss, are insufficient to address aging of the brow/upper eyelid complex.
- •
Preservation and restoration of skin quality can have dramatic rejuvenating effects to the brow and upper eyelid.
Introduction
Appropriate aesthetic rejuvenation of the eyelids and periorbital soft tissues requires a detailed knowledge of relevant anatomy and normal aging changes, and techniques to comprehensively address the presenting deficits and attain natural results to treatment. It has long been accepted that changes in skin quality and appearance and tissue descent convey obvious signs of aging and are principal players in this process. Surgical procedures to elevate and remove excess tissue have traditionally been considered the preferred means to address tissue sagging. Chemical denervation (neuromodulation; Botox botulinum toxin A [BoNTA]) has allowed the addition of effacing hyperdynamic lines and has been shown to be an excellent adjunct to surgery. Over the past few decades, a paradigm shift has occurred, in which it has become clear that facial aging is a more complex, three-dimensional process, affecting all tissue planes (skin, muscle, fat, and bone). The importance of the role of volume loss in this intricate process has been particularly emphasized, especially in relation to the eyelids and periorbita. As facial aging has been evaluated from the perspective of both tissue descent and deflation, more acceptable outcomes to treatment, both surgical and nonsurgical, have emerged. As of 2011, statistics from the American Society of Plastic Surgery show that injection of BoNTA remains the single most performed cosmetic procedure in the United States (approximately 2.6 million procedures). Also, the potential for restoring a youthful shape and contour to a patient’s face has made fillers the fastest growing minimally invasive cosmetic procedure in the United States. In 2011, about 1.2 million facial filling procedures involving hyaluronic acid (HA) were performed, constituting 84% of all filler procedures, and BoNTA and HA together comprise 75% of all nonsurgical procedures performed. These data underscore the importance of contemporary minimally invasive methods of facial rejuvenation. Sundaram and Kiripolsky described their means of addressing facial aging with an outcome-based approach to treatment. They called this the 4 pillars of rejuvenation. This approach includes (1) replacement of tissue volume, (2) regeneration of tissue quality, (3) rebalancing of facial vectors and proportions, and (4) improvement of skin reflectance. Minimally invasive techniques designed to address these principles have become core adjuncts to modern aesthetic facial rejuvenation and have allowed practitioners a means of attaining natural outcomes while avoiding the stigma of volume loss and hollowing associated with older reductive surgical techniques. This article focuses on minimally invasive options to rejuvenate the brow and upper lid complex, with a review of the relevant anatomy and contemporary concepts in upper facial aging.
Introduction
Appropriate aesthetic rejuvenation of the eyelids and periorbital soft tissues requires a detailed knowledge of relevant anatomy and normal aging changes, and techniques to comprehensively address the presenting deficits and attain natural results to treatment. It has long been accepted that changes in skin quality and appearance and tissue descent convey obvious signs of aging and are principal players in this process. Surgical procedures to elevate and remove excess tissue have traditionally been considered the preferred means to address tissue sagging. Chemical denervation (neuromodulation; Botox botulinum toxin A [BoNTA]) has allowed the addition of effacing hyperdynamic lines and has been shown to be an excellent adjunct to surgery. Over the past few decades, a paradigm shift has occurred, in which it has become clear that facial aging is a more complex, three-dimensional process, affecting all tissue planes (skin, muscle, fat, and bone). The importance of the role of volume loss in this intricate process has been particularly emphasized, especially in relation to the eyelids and periorbita. As facial aging has been evaluated from the perspective of both tissue descent and deflation, more acceptable outcomes to treatment, both surgical and nonsurgical, have emerged. As of 2011, statistics from the American Society of Plastic Surgery show that injection of BoNTA remains the single most performed cosmetic procedure in the United States (approximately 2.6 million procedures). Also, the potential for restoring a youthful shape and contour to a patient’s face has made fillers the fastest growing minimally invasive cosmetic procedure in the United States. In 2011, about 1.2 million facial filling procedures involving hyaluronic acid (HA) were performed, constituting 84% of all filler procedures, and BoNTA and HA together comprise 75% of all nonsurgical procedures performed. These data underscore the importance of contemporary minimally invasive methods of facial rejuvenation. Sundaram and Kiripolsky described their means of addressing facial aging with an outcome-based approach to treatment. They called this the 4 pillars of rejuvenation. This approach includes (1) replacement of tissue volume, (2) regeneration of tissue quality, (3) rebalancing of facial vectors and proportions, and (4) improvement of skin reflectance. Minimally invasive techniques designed to address these principles have become core adjuncts to modern aesthetic facial rejuvenation and have allowed practitioners a means of attaining natural outcomes while avoiding the stigma of volume loss and hollowing associated with older reductive surgical techniques. This article focuses on minimally invasive options to rejuvenate the brow and upper lid complex, with a review of the relevant anatomy and contemporary concepts in upper facial aging.
Eyebrow/eyelid anatomy
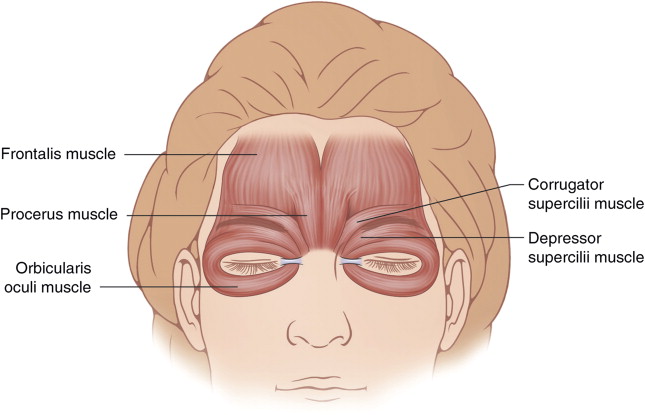
Although a detailed description of anatomic considerations of the eyebrow and eyelid is beyond the scope of this article, a general understanding of the relevant structures of significance and how they transition from the brow to the eyelid is important. The eyebrow is a multilayered structure composed of cilia, skin, muscle, fat, and connective tissue elements. The skin is thicker than that of the eyelid, which is important when manipulating the brow/lid transition. The paired frontalis muscles are the elevators of the eyebrow and originate from the galea aponeurotica, span the forehead from superior temporal line (STL) to STL, and insert on the skin (no bone insertion) at the superior brow after interdigitating with various muscle groups. These muscle include the orbital orbicularis oculi muscle laterally, and the orbicularis oculi, procerus, and corrugator supercilii muscle medially ( Fig. 1 ). Although the frontalis is the only elevator of the eyebrows, the orbital orbicularis, corrugator supercilii, and procerus muscles all depress the brow. There is no eyebrow elevator lateral to the STL, which makes this location especially prone to brow ptosis with age.
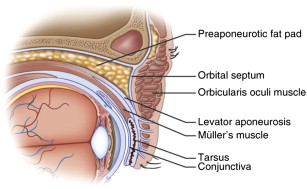
The frontalis muscle is positioned between the superficial and deep layers of the galea aponeurotica proper. Inferiorly, the deep layer of the galea splits into an anterior and posterior leaf that encase the retro-orbicularis oculi fat (ROOF) or brow fat pad. Posterior to the ROOF is the periosteum of the frontal bone. The orbicularis retaining ligament (ORL) is an oseocutaneous structure arising from just above the orbital rim and inserting into the dermis of the skin. Laterally the ORL contributes to the lateral orbital thickening. In combination, these structures lend a degree of support to the soft tissues of the eyebrows. At the superior orbital rim the periosteum of the frontal bone and orbit meet forming the arcus marginalis, which continues into the eyelid as the orbital septum. The ROOF transitions into the eyelid as the postorbicularis fascial plane in caucasian people and the preseptal fat layer in Asian people. The orbital orbicularis from above continues into the eyelid as the preseptal and then pretarsal segments of the muscle (named according the structures they overlie). Posterior to the orbital septum lie the nasal and central (preaponeurotic) fat compartments. The nasal fat pad is contiguous with the deeper orbital fat. The preaponeurotic fat is separated from the deeper orbit by the levator aponeurosis. The aponeurosis is an extension of the levator muscle, which is the primary upper eyelid retractor (elevator). The orbital septum overlies orbital fat and inserts onto the levator aponeurosis which then sends projections to the eyelid skin to form the eyelid crease. The crease typically measures 7 to 8 mm from the lid margin in men and 10 mm in women. Posterior to the aponeurosis is the second eyelid elevator, the Müller muscle. This muscle is an autonomically innervated muscle that arises from the undersurface of the levator muscle and inserts onto the superior border of the tarsus ( Fig. 2 ).
Relevant topography of the youthful and aged upper eyelid/brow complex
The topography of the brow and upper eyelid vary according to gender, age, and ethnicity. Common among all youthful brow/upper lid complexes is a three-dimensional structure with smooth curves and contours that transition well and reflect light in a natural way ( Fig. 3 ). With aging, changes in natural contour, related to tissue descent and deflation, cause these reflections to become interrupted, leading to associated shadowing ( Fig. 4 ). What underlies these involutional changes involves both static and dynamic components. The brow fat pad attenuates with age. In addition, there are equally significant involutional changes in bone, leading to loss of underlying support of the brow. This global loss of volume reduces the static support of the eyebrow, which often leads to secondary tissue descent. This concept of brow position and its relation to volume loss became obvious to one of us (GM) many years ago, because it was noted (also by many colleagues) that the injection of local anesthesia during facial surgery led to an immediate correction of some degree of tissue ptosis. These kinds of observations have led to the more contemporary approach of volume augmentation facial/eyelid restorative surgery, and nonsurgical interventions.


In addition to volume, resting muscle tone is a critical component of typical brow/eyelid aging changes. This muscle tone is the dynamic component characteristic of eyebrow aging. As stated earlier, the frontalis muscle is the elevator of the eyebrows, and it spans the forehead from STL to STL. Temporal to the STL (approximately the junction of the body and tail of the brow) there is no brow elevator. However, there is a depressor of the lateral brow, the orbital orbicularis muscle, lateral to the STL. Age and loss of static support shifts the dynamic equilibrium of brow position to unopposed descent. Consequently it is the lateral brow that tends to become ptotic with age, with the resultant characteristic lateral eyelid hooding for which so many patients seek correction (see Fig. 4 ). Although it is important to understand what underlies typical age-related outer brow ptosis, this should not be considered in isolation. Each patient is different and can present with different findings. The literature is not clear as to what happens to overall brow position with age, with data showing elevation, stability, or depression. Again, this is a static and dynamic process in which the clinical manifestations may be compensatory (ie, the brow may elevate with age as a compensatory response to lid ptosis).
The eyelids also show characteristic changes with age. The youthful lid is full and wide. Like the brow, it is devoid of depressions and contour irregularities. With age there are characteristic changes in volume, both of the underlying bone and of soft tissue. The orbit tends primarily to remodel superonasally and inferotemporally. This remodeling leads to loss of support in those areas and a rounder, more vertically oriented palpebral aperture. Canthal tendon laxity with medialization of the lateral canthus can exacerbate this change. As the eyelid loses soft tissue volume the upper eyelid skin becomes redundant, with both true and pseudoexcess, which leads to hanging skin and hollows. The hollows are most prominent centrally and nasally where the characteristic A-frame deformity occurs ( Fig. 5 ). In some patients with very devolumized orbits/eyelids, rather than skin sagging, the skin retracts into the upper sulcus, unmasking the pretarsal eyelid and giving a skeletonized appearance. When involutional ptosis is present this becomes even more obvious (see Fig. 5 ). In either instance the primary issue is loss of volume and support.

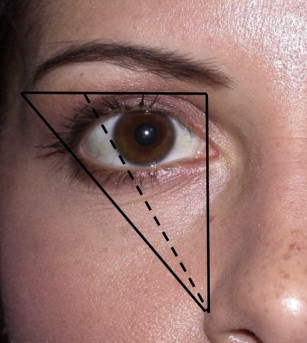
There are distinct differences between the appearance and topography of the male and female eyebrow. In both genders the brow begins medially in a line perpendicular to the medial canthus and nasal ala. It ends laterally in a line tangent to the nasal ala and lateral canthus. In addition, the medial and lateral brow lie vertically at the same level. The tail of the female brow is slightly higher, coursing above the orbital rim. The youthful female brow peaks at a point tangent to a line drawn from the nasal ala through the pupil or lateral limbus, and then tapers inferiorly ( Fig. 6 ). The youthful male brow is flatter and fuller, and runs over the orbital rim without the peak that is evident in women.
Cutaneous changes also play a pivotal role in eyelid and periorbital aging. As skin ages, the dermal collagen matrix becomes fragmented and weakened, with impaired fibroblast function. Instead of producing collagen and stabilizing the dermal matrix, damaged fibroblasts begin to create collagen-degrading enzymes, perpetuating the cycle. This degradation leads to the progressive loss of elasticity of the skin that, when paired with deflation, accentuates and deepens rhytids. In addition, laxity, pigmentary changes, and skin thinning occur.
Minimally invasive treatment of the periorbital skin
Various surgical options exist for the correction of skin laxity. In the upper eyelid and brow, upper eyelid blepharoplasty and a variety of surgical brow lifting techniques are used to reduce skin redundancy and bulk. However, these modalities do nothing to improve skin quality and are inadequate for qualitatively improving skin appearance and texture.
Excellent skin care is the most important aspect of maintaining a youthful facial appearance. Tissue quality and skin reflectance depend on a consistent and ongoing commitment to such a regimen. All patients should use a basic facial moisturization protocol as an integral part of their facial rejuvenation programs. This protocol should include direct application to the brows and upper lids. Daily sun protection with SPF (sun protection factor) 30 or greater is also integral to preventing the discoloration and degeneration of the upper eyelid and brow skin that results from ultraviolet light damage. Ultraviolet-blocking sunglasses and wide-brimmed hats are also important tools in preventing periocular photoaging.
Photoaging may be treated with several topical preparations, such as topical retinoids, hydroquinone, or alpha hydroxyl acids (AHAs). Topical retinoids enhance hyaluronic acid deposition and increase the compaction of the stratum corneum, and topical AHAs increase epidermal thickness by enhancing synthesis of glycosaminoglycans, collagen, and elastic fibers. Microdermabrasion and chemical peels, alone or in conjunction with retinoids, are also effective in reversing the signs of skin photoaging and in improving the appearance of scars and fine rhytids. They deliver selective injury at a depth dictated by the technique used, enhancing collagen synthesis during the healing process. Superficial chemical peels using glycolic acid (20%–70%) or trichloroacetic acid (15%–35%) are a commonly used method of addressing fine lines in the eyelids.
Deeper peels with higher acid concentrations or the use of phenol may be associated with longer recovery, risk of hypopigmentation, and scarring. Any peel technique has a risk of causing reactivation of cutaneous herpetic infection, and a careful history and clinical evaluation must be performed. Some patients require pretreatment with antiviral agents before peeling procedures to mitigate this risk. A comprehensive review of these treatments and techniques is beyond the scope of this article, but may be found in several recent reviews.
Laser resurfacing has also gained popularity in recent decades as a reliable method of improving skin quality and reducing fine lines. In particular, CO 2 and erbium:ytrium aluminum garnet (Er:YAG) lasers are commonly used in the periorbital region for these purposes. Lasers are able to target specific components of the skin, at specific depths to precisely deliver injury to the skin tissue. CO 2 lasers , initially introduced in the 1980s, provide aggressive ablative therapy to the skin, but are associated with significant downtime. The laser emits light at a wavelength of 10,600 nm, which selectively targets water and vaporizes the epidermis as well as a variable thickness of dermis. Fractionation of treatment decreases downtime and adverse effects. Overaggressive treatment with lasers may lead to adverse effects such as prolonged erythema, hyperpigmentation, milia, infections, hypersensitivity, scarring, and ectropion. The Er:YAG laser emits energy in the infrared spectrum at 2940 nm, a wavelength that is also highly absorbed by water but is associated with less residual thermal damage. Recovery is speedier with the Er:YAG versus the CO 2 laser, but the effect is also more subtle. Ablative therapy with the Er:YAG laser may also lead to the adverse effects listed earlier. Pigmentary anomalies are more likely in patients with dark skin.
For mild laxity and rhytids, radiofrequency devices may also be used. Radiofrequency devices deliver thermal injury to the skin in several ways, including fractional bipolar devices, multisource phase-controlled devices, monopolar devices, and combinations of these methods. The thermal energy introduced by the devices does not ablate tissue, but focally injures it with subsequent tissue regeneration. Its effect is not altered by the type of pigmentation of the patient’s skin. It has been shown to yield modest effects in reduction of rhytids.
Microfocused ultrasonography (MFU) is another modality that may be used in mild cases of periorbital aging, without concern for pigmentation anomalies. Transducers generate ultrasonography energy of 4 to 7 MHz, which create zones of thermal microcoagulation 1 to 1.5 mm apart. The energy may be delivered at a depth of 3 to 4.5 mm. Alam and colleagues reported that the lateral brow may be elevated by applying MFU energy to the skin just above the lateral two-thirds of the eyebrow, with a mean elevation of 1.7 mm after treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



