9
Minimally Invasive Eyelid Rejuvenation
Neuromodulation, filling agents, nonablative lasers, and therma-lifting can noninvasively rejuvenate the periorbital tissues. These techniques can be dramatic nonsurgical surgical alternatives for many patients. For other patients these techniques are an essential step to prepare them for laser-assisted surgical procedures. Eyelid skin redundancy and marked loss of elasticity, fatty prolapse, levator aponeurotic disinsertion, lacrimal gland prolapse, and lateral canthal tendon and lower lid margin laxity need to be addressed surgically. Carbon dioxide (CO2) laser techniques allow us to perform skin and skin-muscle resections, levator aponeurotic repairs, lacrimal gland suspensions, lateral canthal plications, lipovaporization, fat transposition, and eyelid skin resurfacing efficiently, with great accuracy and minimal downtime, in a virtually bloodless field.
 Patient Evaluation
Patient Evaluation
The best way to start with these patients is to sit down with them, listen to their comments, look in the mirror with them, and review their old photographs. At the same time you will be observing their face at rest and in animation. Obviously, individual patients have their own anatomic variations. But patients also have their own insights into what they do not like about their faces. We are directed by what the patients see. We listen. We examine them and analyze their faces. And then we make our recommendations, discussing each patient’s options and realistic expectations.
Gender and ethnic variations in blepharoplasty are essential considerations. Male upper eyelids are typically full and their eyebrows are low and flat (Fig. 9-1A,B) whereas female upper lids may have a more defined superior sulcus and a more accentuated brow arch. Oversculpting a male superior sulcus or creating an overly arched brow will feminize the man’s appearance and should be avoided. We discourage Asian patients from occidentalizing their eyelids. Redundant upper eyelid folds can be trimmed and reduced via a very low supraciliary incision, thus avoiding the creation of a double eyelid or elevating a low lid-crease-fold complex. Multiple eyelid creases can be eliminated and asymmetric lid-crease-fold complexes can be corrected (Fig. 9-2A,B).

Figure 9-1 (A) A low flat brow and heavy upper lid folds are male eyelid characteristics. Heavy lower facial musculature and lateral canthal laxity may predispose them to lower lid retraction following a transcutaneous approach. (B) Internal brow stabilization followed by cautious trimming of a male patient’s upper lid without oversculpting the preaponeurotic fat can give a more youthful appearance without feminizing. Transconjunctival carbon dioxide laser-assisted lipovaporization will improve the lower lid contours without risk of lower lid margin displacement.
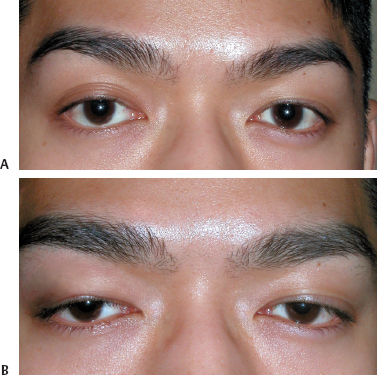
Figure 9-2 (A) An elevated right upper lid crease became evident after an inflammatory episode. (B) Lowering the crease required surgical lysis of the lid-crease-fold complex internal cutaneous adhesions and interpositioning of a layer of Restylane between the skin and orbicularis muscle.
 Anatomical Structure and Position
Anatomical Structure and Position
Facial structures cannot be examined in a vacuum (Fig. 9-3.). The upper lids are intimately related to the level and contour of the eyebrows (Fig. 9-4A,B), just as the lower lids are related to the lateral and medial canthi and the midface. The vertical height of the palpebral aperture may be diminished because of upper lid ptosis (Fig. 9-5A,B) or may be increased because of upper or lower eyelid retraction (Fig. 9-6A,B). Some surgeons use the marginal reflex distance (MRD) measurement to further qualify absolute measurements of the vertical palpebral aperture. In any case the relationship of the upper lid margin to the pupil and the lower lid margin to the inferior limbus must be noted.
Lower lid margin and/or lateral canthal laxity may be significant even in the absence of overt lower lid margin retraction and inferior scleral show (Fig. 9-7A,B). The snap test and the distraction test alone are not the only relevant factors in predicting lower lid margin displacement after a procedure. Granted, the amount of lid margin laxity (distraction test) that can be demonstrated by pulling the eyelid away from the globe (greater than 8 mm is deemed lax) and the rapidity of the lid margin returning to its normal anatomic position against the globe (snap test) will demonstrate the stability of the lower lid margin. But the amount of inferior scleral show, lower lid margin retraction, and prominence of the globe (whether secondary to high myopia and a large globe or shallow bony orbits) have a significant impact on the potential for postoperative lower lid margin displacement (Fig. 9-8A,B).
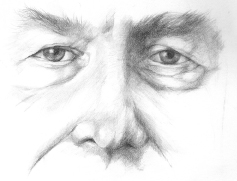
Figure 9-3 Male upper lid blepharoplasties may need internal brow fixation to stabilize the brow before upper lid fold resection. Male lower lid blepharoplasties may need lateral canthal suspension to stabilize the lower lid margin before cutaneous resurfacing.
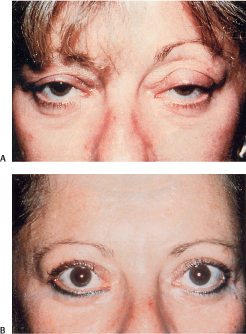
Figure 9-4 (A) This patient exhibited the hallmarks of blepharoptosis—narrowed palpebral apertures, elevated lid crease-fold complexes, and secondary compensatory brow elevation. (B) Marked bilateral upper lid blepharoptosis and lower lid retraction were improved with laser-assisted upper lid blepharoplasty, levator aponeurotic repair, recession of lower lid retractors, and lateral canthal plication.
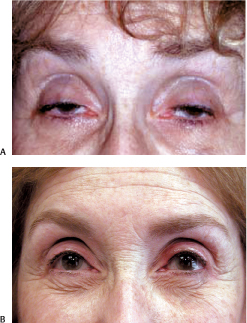
Figure 9-5 (A) When repairing prominent levator aponeurotic disinsertions that create marked blepharoptosis and deep superior sulci, old photographs may be helpful to determine placement of the lid crease incision and the depth of the reconstructed superior sulcus. (B) This patient’s final result after levator aponeurotic repair was enhanced with micropigmentation of her superior eyelid margin.
 Surgical Plan
Surgical Plan
We use carbon dioxide laser assisted techniques for all of our procedures. We use the 0.2 mm handpiece as a cutting tool and the Lumenis Ultra Pulse C5000 computer pattern generator (CPG) (Lumenis, Santa Clara, California) as a resurfacing tool. We also use the Lumenis Ultra Fine (Lumenis) erbium: yttrium-aluminum-garnet (Er:YAG) CPG as a resurfacing tool in selected patients.
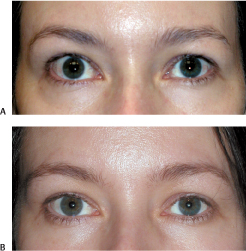
Figure 9-6 (A) Idiopathic retraction of this patient’s right upper lid (normal thryroid workup) exposes the superior limbus and enlarges the palpebral aperture. (B) Her apertures are symmetric following recession of her right upper lid retractors.
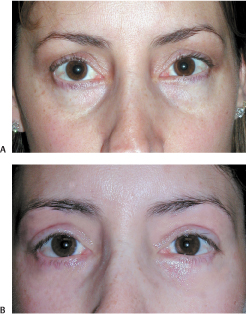
Figure 9-7 (A) A right lower lid retraction and a tear trough deformity following a transcutaneous lower lid blepharoplasty. (B) It was corrected with a right lateral canthal plication, bilateral transconjunctival fat transposition, and lower lid CO2 laser resurfacing (150 mJ, one pass, pattern 3, size 4, density 6).

Figure 9-8 (A) Shallow orbits create inferior scleral show. (B) Lateral canthal support is essential to stabilize the lower lid margins when performing a transconjunctival lower lid blepharoplasty.
For the comfort and safety of the patient and operating room staff, a high-power plume evacuator is utilized to remove the vapor plume from the surgical field. All personnel in the operating room suite wear protective goggles and filtration masks.
Topical tetracaine drops are applied to each eye. The patient is prepped and then draped in sterile heavy-duty tinfoil. Nonreflective, metallic corneal protectors are applied to each eye. After the preoperative decisions have been made for the surgical plan, the following is our customary order of surgical procedures:
- Demarcation of upper lid crease incision and cutaneous or myocutaneous resection
- Xylocaine infiltration of upper lid cutaneous incision, resection, and resurfacing sites (<1 mL per side is injected if levator aponeurotic adjustment is to be performed)
- Upper lid crease incision (Fig. 9-9.)
- Levator aponeurotic repair (Fig. 9-10)
- Infiltration of preaponeurotic fat, brow, lateral can-thus, lower lid
- Suspension of prolapsed lacrimal gland (Fig. 9-11)
- Vaporization of upper lid preaponeurotic fat
- Internal brow stabilization (Fig. 9-12)
- Lower lid transconjunctival lipovaporization and fat transposition (Fig. 9-7A,B)
- Lateral canthal plication
- Eyelid laser resurfacing (Fig. 9-13A,B)
- Wound closure

Figure 9-9 The CO2 laser (ultrapulse mode, 400 Hz, 5 mJ) is used to incise the upper lid skin.
Skin Texture Rhytidosis, Lesions, and Periorbital Veins
Patients often perceive eyelid wrinkling as excess skin. And indeed in the past our proposed surgical remedy encouraged this manner of thinking: skin resection. True skin excess may exist, but a loss of skin elasticity or a deterioration of skin texture can give the appearance of rhytidosis. When evaluating the upper eyelid, the patient and physician have to decide if they wish to reduce the size of the fold, to improve the texture of the skin, or both. Upper lid skin management requires a blending of resection and laser resurfacing. Lower lid skin management requires either or both chemical peeling or laser resurfacing with lateral canthal support when necessary (Fig. 9-14A,B). Resurfacing the pretarsal lower lid skin is avoided when possible, particularly medially anterior to the inferior punctum. Laser resurfacing in this area may predispose the lower lid to inferior retraction and punctal eversion.
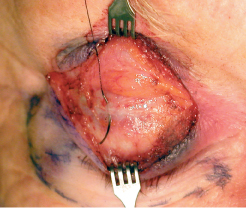
Figure 9-10 A 6–0 black silk suture is used to reapproximate a disinserted levator aponeurosis to the anterior tarsal surface.
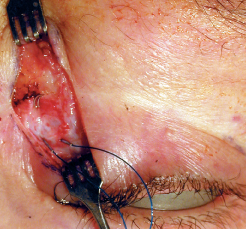
Figure 9-11 A double-armed 4–0 Prolene suture is used to suspend the orbital lobe of the lacrimal gland to the periosteum of the lacrimal fossa.
Intradermal nevi, adenomas, and keratoses are shaved with a radiosurgical loop (Ellman International, Hewlett, New York) to make them flush with the eyelid surface before laser resurfacing. Perioperatively periorbital veins that are apparent through translucent skin can be ablated with a 1064 nm laser utilizing 120 to 140 J/cm2 with a 3 mm spot (Cutera Cool Glide, Bristane, CA) (Fig. 9-15A,B).

Figure 9-12 Internal brow suspension. The Prolene suture is passed through the brow subcutaneous tissue and anchored to the periosteum 5 mm superior to the superior orbital rim.
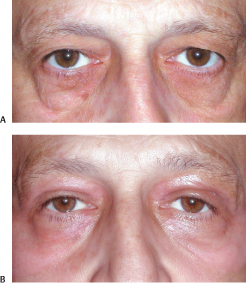
Figure 9-13 (A) Low, flat, masculine brows must be stabilized before upper lid skin redundancy can be addressed. (B) Pretreated with a “Botox browlift,” internal brow stabilization facilitated creation of a natural-appearing masculine upper lid following myocutaneous resection and laser resurfacing. Transconjunctival lipovaporization, lateral canthal plication, and carbon dioxide laser resurfacing were used to improve this patient’s lower lid and malar contours.
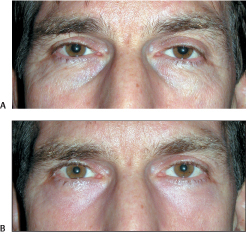
Figure 9-14 (A) Mild fatty prolapse and moderate lower lid skin rhytidosis were this patient’s complaints. (B) Transconjunctival lipovaporization and laser resurfacing provided a smoother lower eyelid contour for this patient.

Figure 9-15 (A) Lower eyelid veins may be visible through translucent skin. (B) Lower lid and periorbital varices were effectively treated with a 1064 nm laser (Cutera Cool Glide; 140 J/cm; 3 mm spot).
Stabilization of Brow Level and Contour
With the patient seated in an upright position, facing the surgeon, the brow arch and relation to the superior orbital rim are determined. Old photos are reviewed with the patient to determine if there has been any change in brow level and contour.
In males, a flat contour and a position at the level of the superior orbital are acceptable. A level inferior to the rim will cause excessive hooding and upper lid fold redundancy (Fig. 9-16). If the brow is mobile and easily elevated, the amount of elevation laterally (at the tail of the brow), and centrally (in line with the lateral limbus) is noted. If there is medial brow ptosis, it is noted.
Female patients who have always had a flat brow contour and want to maintain it are managed in the same fashion as male patients. In female patients who have lost their brow contour and want to re-create it, the amount of elevation laterally, centrally, and medially is noted.
Patients are pretreated with neuromodulation of the brow depressors to modify brow level and contour (see Chapter 5. This will give the patient a partial preview of the final result as well as enhancing the surgical result by relaxing the brow depressors during the postoperative period.
For brow stabilization and minimal elevation, in cases where only 1 or 2 mm of elevation are necessary, we prefer the transblepharoplasty approach, utilizing the CO2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



