17
Photodynamic Therapy for Scarless Removal of Multiple Facial Precanceroses and Superficial Carcinomas
Skin cancer is by far the most common human malignancy. It is estimated that basal cell carcinomas (BCCs) alone are as frequent as all other organ cancers taken together. Actinic keratoses (AKs) are classical precursor lesions for squamous cell carcinomas (SCCs). There is a strong link between ultraviolet light (UVL) exposure and skin cancers; this is a direct quantitative relationship of AKs with sun exposure whereas this relationship is not so clear concerning BCCs. All patients having had one skin cancer have a risk of at least 25% of developing another primary skin malignancy, often of the same type, and patients with two or more skin cancers have a risk of over 50% to develop more. In addition, most AK patients present with multiple lesions and are prone to continuously develop more of them because the noxious effect of chronic UVL exposure continues lifelong. Thus a fair-skinned Caucasian may develop hundreds of cutaneous precanceroses and invasive carcinomas during life. Over 80% of them will be localized in the head and neck region. Surgical removal is often no challenge in the beginning, but scarring and increasing lack of movable skin may finally pose a great problem. Treatment modalities avoiding tissue loss are therefore a great advantage in the management of patients with multiple facial precancers and superficial carcinomas.
 Patients and Methods
Patients and Methods
Twenty-five consecutive patients with superficial malignant skin lesions—AKs, Bowen’s disease, superficial BCCs—underwent photodynamic therapy (PDT) with 5-aminolevulinic acid (5-ALA) methyl ester 16% cream (Metvix). Metvix was generously applied for a minimum of 3 hours under occlusion and protected from light until treatment. The occlusive dressing was then removed, excess cream wiped off, and red light 75 J/cm2 applied to the lesion. To avoid painful heat sensation, the patient received a cold air blowing tube that could be adjusted according to heat development and individual sensitivity. Sensitive anatomic structures, such as the eye, immediately adjacent to the treatment area were protected. Irradiation time was generally 7 to 8 minutes per field. The treated lesions were left open and the patients informed that they might have a burning sensation within the first day after treatment and would probably develop a red area corresponding to the site of Metvix absorption.
AKs were treated with one PDT, Bowen’s disease and superficial BCCs with two PDT sessions. Lesions thicker than 2 mm were excluded from this treatment modality, as were nodular BCCs. Considerable hyperkeratoses were removed prior to treatment of AKs.
Patients were re-examined after 1, 2, 4, and 6 weeks, and after 6 and 12 months, as well as. Because all these patients have a great risk of developing more skin cancers consistent clinical follow-up once to twice a year was recommended.
 Results
Results
There were 11 women and 14 men; the mean age was 56 years. Twenty patients had AKs, four patients superficial BCCs, and one patient recurrent Bowen’s disease. Several AK patients had more than 10 AKs.
All 109 AKs treated reacted favorably and disappeared completely (Fig. 17-1A-C). A second treatment was applied for two lesions only. The patient with Bowen’s disease was initially treated once, but the lesion recurred after 8 months, so that another therapy cycle with two PDTs 4 weeks apart was instituted. Of the four BCC patients, one had a superficial recurrence on the tip of her nose after cryosurgery; she is free from recurrence 20 months after two PDTs. The other three patients together had seven superficial BCCs, which received two PDTs each.
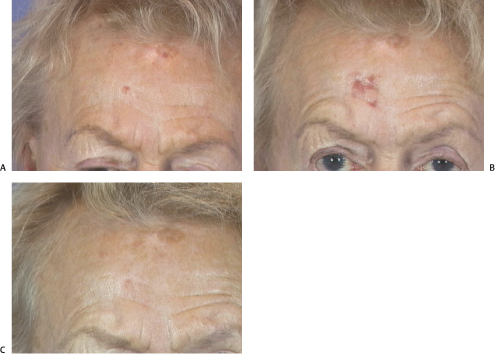
Figure 17-1 Actinic keratosis on the forehead (A) before photodynamic therapy (PDT). (B) One week after PDT, the erythema demonstrates the true extent of the lesion. (C) Six months after PDT.
PDT was generally tolerated very well. One patient-very fair-skinned, red-haired with freckles—reacted with very intense red spots after PDT that subsided within 2 weeks (Fig. 17-2A-C). Most patients developed mild to moderate erythema in the area of Metvix application.
 Discussion
Discussion
The need for skin-preserving treatment of multiple cutaneous cancers, particularly in the face, is growing because more and more patients present with multiple lesions after years of sun exposure abuse. Tangential (“shave”) excision heals fast by secondary intention, yields a specimen for histopathological confirmation of the diagnosis, and allows margin control; however, many patients with multiple skin cancers do not wish to have cold steel surgery. Curettage and dermabrasion also leave open wounds. Chemocautery causes a chemical burn that takes about 2 weeks to heal. Electro- and laser surgery cause slow-healing burn wounds. Radiotherapy is not indicated for most superficial cutaneous cancers. Cryosurgery is an established and simple method for superficial lesions; however, the resultant cryonecrosis takes weeks to heal and the scar is usually hypopigmented and loses its hair follicles. Topical cytotoxic treatment with 5% 5-fluorouracil requires a 1-month treatment and must be performed until the lesions are erosive, which is often quite painful. Topical immunotherapy with imiquimod requires 6 weeks of treatment with burning and itching being almost constant adverse effects. In contrast, PDT requires only one or two treatment sessions, and untoward effects both during and after treatment are minimal to moderate. Long-term observations have shown very good healing rates and excellent cosmetic results.1–9
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



