Aging of the midface and lower eyelid represents one of the earliest clinically detectable areas of aging on the face. These senile changes include laxity of eyelid skin, pseudoherniation of orbital fat, ptosis of the suborbicularis oculi and malar fat pads, and loss of facial volume. Several approaches, including surgical and nonsurgical procedures, have been developed to counter the effects of aging on the midface and lower eyelid. This article reviews the techniques used by the authors to rejuvenate the midface and lower eyelid, and illustrates a comprehensive approach to management of this complex facial region.
Rejuvenation of the aging face has undergone significant transformation over the past 20 years. Collective understanding of the physiologic forces of aging on skin, soft tissue, and facial bony structures has permitted the development of various surgical and nonsurgical treatments to correct or limit these effects. Further, increased understanding of the importance of volume restoration in facial rejuvenation has improved the results of interventions and addressed a critical component of aging that was previously ignored. Although almost all aspects of facial plastic surgery have significantly evolved during this time, restoration of the aging midface has been particularly rewarding for most surgeons and patients. This article seeks to describe the importance of midface restoration, the evolution of various treatments that have been developed, a synopsis of the authors’ current approach to rejuvenation of the midface complex, and the role of midface restoration in the management of the aging lower lid.
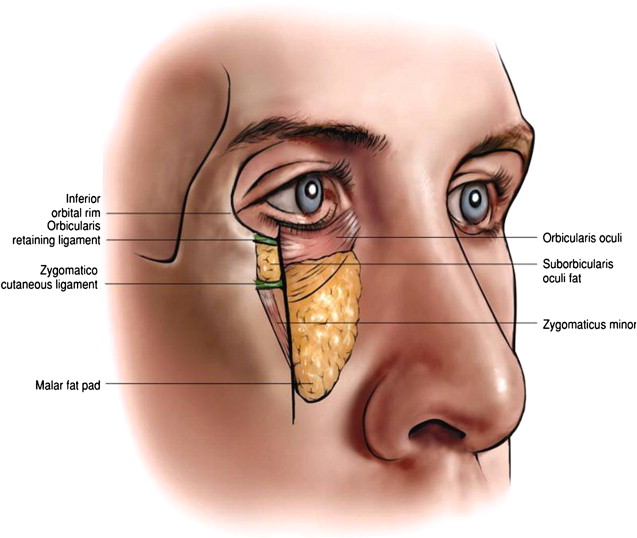
The anatomy of the midface has been well described by many investigators but often lacks clearly described anatomic boundaries. To simplify discussion on this topic, the midface is defined as an inverted triangular volume of tissue bordered laterally by a line drawn from the lateral canthus to the oral commissure and medially by a line drawn through the nasolabial fold from the medial canthus. Anatomically, this complex contains the lower sling of the orbicularis oculi muscle, orbicularis and zygomaticocutaneous retaining ligaments, the suborbicularis oculi fat (SOOF) pad, and the malar fat pad. One of the most challenging aspects encountered in the study of the midface is a thorough understanding of the relationship of the midface to the lower lid. It is difficult to know precisely where the lower lid ends and where the midface begins. Even so, the authors have found that a precise anatomic separation between these 2 structures is often unnecessary, because it is the combined rejuvenation of the midface and lower lid complex that results in optimal aesthetic rejuvenation. For the authors, this concept of zonal rejuvenation has become a key driving force to obtaining natural results, and has resulted in improved midface restoration.
Aging of the midface and lower lid complex is a continual process that involves changes to the skin, soft tissue, and bony facial structures. Many women and men show clinical signs of aging to the midface and lower lid in their late 30s, making this one of the earliest detectable areas of facial aging and, consequently, one of the initial areas of patient concern. Aging of the midface and lower eyelid skin is largely exacerbated by environmental effects that include solar damage, as well as the formation of rhytids caused by repeated muscular contractions. Soft-tissue changes to the midface and lower lid include a weakening of the orbital retaining ligaments and an inferior displacement of the zygomaticocutaneous ligament ( Fig. 1 ). These changes are thought to be largely caused by the gravitational effect on facial soft tissue. A direct result of this effect is vertical displacement of the lower eyelid and the loss of a youthful-appearing, short, and full eyelid. A youthful eyelid should be free of tarsal ligament laxity, with strong tone and an adequate septum that resists pseudoherniation of the orbital fat, whereas a youthful midface should demonstrate adequate vertical height of the SOOF and malar fat pads, providing support to the malar area.
One of the most important and previously overlooked features of an aged midface and lower lid is the loss of facial volume. This process is thought to be secondary to atrophy of the SOOF and malar fat pads. As a result of these changes, the midface and lower lid appears deflated, flat, and hollow, exacerbating the underlying bony facial structure. The periorbital changes described above are observed in continuity with deepening of the nasolabial fold and ptosis of the midface with vertical descent of the SOOF and malar fat pad. The combined result of these aging changes creates a loss of facial width in the malar region, a tear trough deformity, and the projection of a tired appearance ( Fig. 2 ).

One of the earliest interventions in countering the effects of midface aging was a surgical approach to specifically address the ptotic fat pads and soft tissue. A historical review of surgical midface lifts has recently been published. The senior author (E.F.W.) employed an endoscopic subperiosteal approach to the midface in the mid 1990s after careful consideration of the physiologic effects of aging as well as of the safety of the technique. As described by Ramirez, the endoscopic midface lift involves careful elevation of the SOOF pad with the underlying periosteum along the inferior orbital rim and malar areas by creating a dissection plane between the malar-zygomatic arch and the temporal pocket. The experience gained from endoscopic brow lifting and from the management of bony facial trauma in a subperiosteal plane has made this approach familiar to many facial plastic surgeons. Additional considerations such as the importance of maintaining a safe lower lid and attaining adequate visualization of the midface were paramount in the development of this particular technique.
Subperiosteal midface lift
A complete description of subperiosteal midface lift has already been published, and a summary is given here. The patient is administered anesthesia either via intravenous sedation or general anesthesia. Appropriate preparation consists of securing the patient’s hair tufts with brown paper tape and the marking of standard endoscopic incisions. If a brow lift is to be performed at the same time, endoscopic brow lift incisions are marked with a 2-cm incision in the midline, 2 2-cm incisions located lateral to the midline in a paramedian position (approximately at the lateral canthus) just posterior to the hairline, and 2 additional 3- to 4-cm incisions located over the temporal region and extending over a 4-cm distance above the helical crus and over the temporalis muscle and fascia ( Fig. 3 ). After infiltration of local anesthetic (1% lidocaine with 1:100,000 epinephrine) to the incision sites and midface, surgical incision is performed along the marked incisions, and an endoscopic brow lift, if planned, is performed by subperiosteal release of the brow through the midline and paramedian incisions with suture resuspension through cortical bone tunnels. For the midface, the planned temporal incision is made down to the level of the temporoparietal fascia (TPF), and dissection is performed with a blunt elevator over the true temporalis fascia. Dissection is performed downward to the orbital rim and the arcus marginalis is released from the superolateral orbital rim near the lateral canthus with the periosteal elevator. Further dissection is then made inferiorly toward the midface by entering the temporal fat pad and releasing the periosteal attachments over the zygomatic arch itself, with careful attention paid to avoid injury to the overlying frontal branch of the facial nerve. The subperiosteal dissection is then continued inferiorly over the malar eminence to release the zygomaticus major and minor muscular attachments and malar fat pad from the underlying malar bone ( Fig. 4 ). This dissection is performed until the midfacial structures are adequately released, but unintended masseteric elevation is unnecessary because it can lead to trismus and spasm. Suture suspension of the midface soft tissue is then performed to the temporalis fascia with a vertically oriented vector to minimize distortion of the lateral canthus ( Fig. 5 ). Redundant temporalis soft tissue is pulled superolaterally by suturing the TPF just anterior to the temporoparietal incision to the temporalis fascia, and closure is performed with surgical staples.



A review of the authors’ experience with subperiosteal midface lifting was performed, which involved a retrospective review of 325 charts for complications as well as determination of a facial aesthetic rating for various facial zones postoperatively. In this study, zone I included the malar complex, zone II included the nasolabial sulcus, and zone III included the jaw line. Results from this study indicated significant improvement in zone I (70% marked, 30% mild) and zone III (30% marked, 50% mild), with less than optimal results for zone II (60% mild, 36% no improvement). The study also confirmed the rarity of complications following subperiosteal midface lift, which included subperiosteal abscess, neuropraxia of the facial nerve, and prolonged edema of the midface. In addition, lateral canthal distortion after subperiosteal midface lift, a valid concern among many surgeons, was found to be insignificant in this study population.
Advantages of the subperiosteal midface approach include safety, with avoidance of direct injury to neurovascular structures over the temple and midface. As described, the approach can be readily adapted to address the midface, temporal area, and brow simultaneously, thereby achieving rejuvenation of the upper two-thirds of the face. The subperiosteal midface lift results in the tightening of the orbicularis sling with a resultant shortened lower eyelid ( Fig. 6 ). In addition, this approach directly repositions the malar fat pad and has also been shown to result in some improvement of the ptotic tissue of the upper jowl ( Fig. 7 ). Limitations of this procedure include the possibility of temporary lateral canthal overtightening, but unlike the direct transconjunctival approach, a lateral canthopexy is not required and permanent lateral canthal distortion with rounding or various degrees of ectropion can be avoided. Other limitations include dimpling of the skin at the sites of suture suspension if placed too superficially, limited results in patients with poor bony structure and thick, round faces, and the possibility of subtle postoperative results.










