Microvascular Free Transfer of A Compound Deep Circumflex Groin and Iliac Crest Flap to The Mandible
G. I. TAYLOR
R. J. CORLETT
EDITORIAL COMMENT
This is an outstanding, now classic description of the compound transfer of bone and soft tissue for facial bone reconstruction. The results are spectacular and speak for themselves. The problems associated with this flap are obviously the need to be expert in microvascular surgery and, specifically, the need to transfer a bulky flap with very little free mobility of the overlying skin. This may present some problems in planning the reconstruction.
The vascular territory of the deep circumflex iliac artery encompasses a large amount of skin and bone that can be used for one-stage transfer with reliability. The bone graft is well vascularized and provides excellent contour for the mandible, and the donor site has minimal morbidity (1, 2). In addition to skin, other soft-tissue elements can be harvested with a common blood supply to provide a functional as well as an aesthetic result. This composite graft is best suited for the difficult problems encountered in head and neck reconstruction (3, 4, 5).
INDICATIONS
There have been many significant advances in the past 20 years in reconstruction of major defects of the mandible and the associated soft tissues (6, 7, 8, 9). Initially, the forehead and deltopectoral flaps improved soft-tissue repair. They provided better coverage for nonvascularized bone grafts, taken usually from the iliac crest or the rib. Their reliability fell dramatically, however, if the area was heavily irradiated. The musculocutaneous flap provides additional bulk, as well as vascularized muscle, to cover the carotid vessels; however, the supply to associated bone segments has not proved to be reliable.
Although a number of donor sites have been used for this purpose, we believe that the iliac crest flap, designed initially on the superficial circumflex iliac artery and, more recently, on the deep circumflex iliac artery, has a number of advantages, especially when the bone gap is considerable. Large amounts of both iliac bone and groin skin are available from an area that has minimal donor-site morbidity, both cosmetic and functional.
The vessels for anastomosis are large, ranging from 1.5 to 3.0 mm in diameter, permitting reliable anastomoses. The pedicle is long, from 5.0 to 9.0 cm. The anatomy is familiar to most surgeons. Not only is the iliac crest the ideal shape for mandibular reconstruction, but sufficient bone is available in an adult to reconstruct an entire mandible with a vascularized graft from one hip.
The bone can be contoured or split, or appropriate osteotomies can be performed to obtain an exact replica of the jaw. Also, soft tissue other than skin may be included in the graft design to reconstruct muscle and ligamentous attachments to the lower jaw.
ANATOMY
The deep circumflex iliac artery arises from its posterolateral side at the level of the inguinal ligament. The artery, together with its paired venae comitantes, courses upward and laterally in its own fascial sheath behind the inguinal ligament toward the anterior superior iliac spine (Fig. 208.1). The paired venae comitantes join to form a single vein 2 to 3 cm lateral to the external iliac artery. This vein then characteristically diverges upward from its artery to reach the external iliac vein. In so doing, it crosses either in front of or behind the external iliac artery. At this point of divergence, there is usually a communication with one of the venae comitantes of the superficial circumflex iliac artery.
Approximately 1 cm medial to the anterior superior iliac spine, a large ascending muscular branch is given off. This vessel pierces the transversus muscle and the internal oblique. It may be found reliably 1 cm above and lateral to the anterior superior iliac spine. Rarely, the deep circumflex iliac vessels may lie in a more superficial plane, and when this occurs, the variation usually is associated with an abnormal obturator artery.
 FIGURE 208.1 Diagram of the deep circumflex iliac artery with its periosteal supply to the inner cortex of the ilium and the musculocutaneous perforators that pierce the three muscles of the abdominal wall at intervals to nourish the overlying skin. The iliacus muscle is cross-batched. (From Taylor et al., ref. 2, with permission.) |
The musculocutaneous perforators to the skin arise from the parent artery as it lies adjacent to the inner aspect of the ilium. They penetrate the muscles beyond the anterior superior iliac spine and emerge from the external oblique in a row approximately 1 cm above the iliac crest. The terminal part of the deep circumflex iliac artery usually emerges as the largest perforator 8 to 10 cm from the anterior superior iliac spine.
The deep circumflex iliac artery is 1.0 to 1.5 mm in diameter and is usually suitable for anastomosis. It can be used to provide a distal runoff from the graft or to connect to another vessel (e.g., the superficial circumflex iliac artery) to augment cutaneous circulation. After division of the three layers of the abdominal wall, the deep circumflex iliac artery will be found situated in the fold between the overhanging transversus muscle and the iliacus.
FLAP DESIGN AND DIMENSIONS
We perform angiography on most patients, which provides valuable information on both the donor and recipient vessels (Fig. 208.2). It outlines the effects of previous surgery, radiation, or tumor expansion on the vascular anatomy. The finding of an abnormal obturator artery in the groin is a preoperative warning that the course of the deep circumflex iliac artery may be more superficial than normal, although we have yet to encounter this in a clinical case.
The presence or absence of suitable recipient vessels on one side of the neck is noted after neck dissection or radiation therapy, and this predicts the need for vein grafts or a modification of graft design.
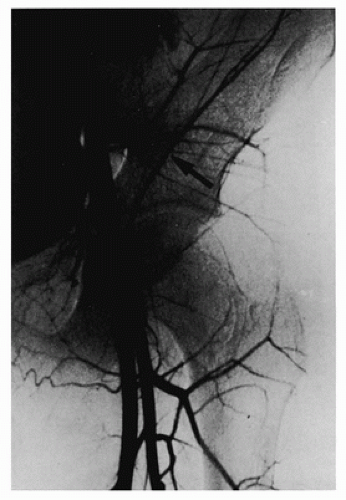 FIGURE 208.2 Angiogram showing the characteristic “paintbrush stroke” of the deep circumflex iliac artery passing upward and laterally at 45 degrees from the region of the hip joint. (From Taylor, Daniel, ref. 11, with permission.) |
An acrylic pelvis with detachable iliac crests is a useful aid when selecting the donor hip for planning the correct orientation of the graft. A methyl methacrylate replica of the bone defect is made preoperatively and used both in the planning and as a preoperative check of the size and shape of the graft both at the donor and recipient sites (Fig. 208.4). The mandible may be designed from the iliac crest in one of three ways, depending on the length of graft required and the position of the vascular pedicle (see Fig. 208.1).
The usual method uses the ipsilateral hip. The lower jaw is designed in such a way that the anterior superior iliac spine becomes the angle of the mandible, the anterior inferior iliac spine becomes the head, and the iliac crest becomes the body of the mandible. The vascular pedicle will be situated behind the new angle of the jaw. Here it is readily accessible for anastomosis to one of the branches of the external carotid system (e.g., the facial artery). This design allows the greatest length of graft to be obtained for mandibular construction. A wedge or step osteotomy is performed in the midline to adjust the curvature of the bone when the graft extends beyond the chin (Fig. 208.5, left).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








