GENERAL 
 What is the anatomy of the mandible?
What is the anatomy of the mandible?
The mandible consists of two bony halves fused in the midline (symphysis). Each hemimandible consists of a condyle, neck, ramus, angle, and body. The masseter, temporalis, and medial pterygoid muscles close the mouth.
The lateral pterygoid muscle protracts the mandible and opens the mouth. The digastric, mylohyoid, geniohyoid, and genioglossus muscles also help open the mouth.
 What is the blood supply to the mandible?
What is the blood supply to the mandible?
The inferior alveolar artery, which is a terminal branch of the maxillary artery. It courses within the mandible along with the inferior alveolar nerve. The mandibular periosteum also provides additional blood supply.
 What nerve supplies sensation to the mandible?
What nerve supplies sensation to the mandible?
The inferior alveolar nerve, which enters the mandible on the lingual side of the ramus through the mandibular foramen. It travels through the mandible supplying sensation to the teeth, then a branch (mental nerve) exits the mandible at the mental foramen to supply sensation to the lower lip. Lower lip cancers can invade the mandible by perineural spread along the mental and inferior alveolar nerves, in addition to involving the mandible by direct extension.
 What is the function of the mandible?
What is the function of the mandible?
The mandible is essential for normal mastication, swallowing, and speech. It also sets the proportions and aesthetic contours of the lower face.
 What are the goals of mandibular reconstruction?
What are the goals of mandibular reconstruction?
1. Reestablish facial balance and symmetry.
2. Create a surface for mastication or dental restoration.
3. Prevent deviation of jaw leading to malocclusion.
4. Provide a stable wound that does not result in orocutaneous fistula.
 What are the common indications for mandibular reconstruction?
What are the common indications for mandibular reconstruction?
1. Primary bone tumor (e.g., osteosarcoma).
2. Tumor involving adjacent structures (e.g., squamous cell carcinoma of floor of the mouth).
3. Osteoradionecrosis.
4. Traumatic defects.
 What is the most common malignancy involving the mandible?
What is the most common malignancy involving the mandible?
Squamous cell carcinoma arising from the oral mucosa and invading the mandibular bone is the most common malignancy.
 What is ameloblastoma?
What is ameloblastoma?
Ameloblastoma is the most common odontogenic tumor. It is a locally aggressive, slow-growing epithelial neoplasm. The tumor is painless and causes gradual jaw expansion producing facial asymmetry. It is usually benign although rare malignant variants exist.
 What are the options for mandibular reconstruction?
What are the options for mandibular reconstruction?
1. Vascularized bony flaps such as a free fibular, iliac crest, scapula, or radial forearm osseous or osteocutaneous flap.
2. Pedicled pectoralis major muscle flap with or without reconstruction plate, or rib graft.
3. Nonvascularized bone graft.
4. Soft-tissue free flaps such as anterolateral thigh flap, rectus abdominis myocutaneous.
5. Primary closure.
 When can nonvascularized bone grafts be used in mandibular reconstruction?
When can nonvascularized bone grafts be used in mandibular reconstruction?
In small (<5 cm) isolated bony defects with good soft-tissue coverage and no history or need for radiation.
 What are the most common complications associated with the use of a reconstruction plate and soft tissue?
What are the most common complications associated with the use of a reconstruction plate and soft tissue?
1. Plate exposure.
2. Plate fracture or fatigue.
3. Screw loosening.
4. Infection.
 What are the major risk factors of reconstruction plate extrusion?
What are the major risk factors of reconstruction plate extrusion?
1. Anterior location.
2. Pre- or postoperative radiation.
 What is the Andy Gump deformity?
What is the Andy Gump deformity?
Resection of the anterior segment of the mandible, which leads to loss of oral competence, difficulties with speech and mastication and loss of chin projection.
 When might soft-tissue flaps be considered for mandibular reconstruction?
When might soft-tissue flaps be considered for mandibular reconstruction?
1. Posterior/lateral defects.
2. Sick or elderly patients who cannot tolerate a lengthy operation.
3. No bony options because of previous surgery/trauma or medical comorbidities.
 What are the typical pedicle lengths for the fibula, iliac crest, and scapula flaps?
What are the typical pedicle lengths for the fibula, iliac crest, and scapula flaps?
1. Fibula: 6 to 8 cm, but can be lengthened if fibula is removed from proximal pedicle.
2. Iliac crest: 6 to 8 cm.
3. Scapula: 4 cm, up to 14 cm if subscapular artery is included.
4. Radial forearm: up to 20 cm.
 How are the bony flaps fixed to the native mandible?
How are the bony flaps fixed to the native mandible?
With a reconstruction plate or miniplates. Studies have not shown any difference in rates of malunion or other complications.
 What are the advantages and disadvantages of use of miniplates?
What are the advantages and disadvantages of use of miniplates?
Advantages:
1. More precise application of hardware to bone flap.
2. Low profile and, therefore, avoids adding bulk to external surface of the bone.
3. Ease of selective removal should the need arise (e.g., extrusion).
4. Provides adequate stability.
Disadvantage:
1. Requires steeper learning curve to shape bone flap.
 What are the advantages and disadvantages of use of a reconstruction plate for flap fixation?
What are the advantages and disadvantages of use of a reconstruction plate for flap fixation?
Advantages:
1. Can be used as a template to help shape the bone flap.
2. Strong rigid fixation.
Disadvantages:
1. Plate can be bulky and hence palpable in patients with minimal soft-tissue coverage.
2. Stress shielding can lead to load bearing and subsequent bony resorption and osteopenia.
 What is the minimal length of an osteotomized segment?
What is the minimal length of an osteotomized segment?
Ideally at least 1.5 cm to ensure an adequate periosteal blood supply to the segment.
 What is osteoradionecrosis (ORN) of the mandible?
What is osteoradionecrosis (ORN) of the mandible?
A necrotic wound in irradiated bone that persists for 3 to 6 months without healing. The period of highest risk for ORN is the first 3 years after radiation therapy and most cases occur at radiation doses greater than 60 Gy.
 What are the indications of resection and reconstruction of ORN?
What are the indications of resection and reconstruction of ORN?
1. Pain.
2. Fistula.
3. Fracture.
4. Exposed bone.
 What must be excluded prior to diagnosing ORN?
What must be excluded prior to diagnosing ORN?
Recurrent cancer.
 What is the optimal method of treatment for ORN of the mandible that has failed conservative treatment?
What is the optimal method of treatment for ORN of the mandible that has failed conservative treatment?
Resection of necrotic mandible and reconstruction with a free flap to bring well-vascularized tissue into the irradiated area.
 What is the role of hyperbaric oxygen in the treatment of ORN?
What is the role of hyperbaric oxygen in the treatment of ORN?
The use of hyperbaric oxygen is controversial. It is frequently used to treat ORN; however, the practice is not supported by randomized clinical trials. It may be helpful for small lesions, following surgical debridement.
 What is bisphosphonate related osteonecrosis of the jaws (BRONJ)?
What is bisphosphonate related osteonecrosis of the jaws (BRONJ)?
Similar to ORN, patients who receive intravenous bisphosphonate for cancer or, much less commonly, oral bisphosphonates for osteoporosis, are at risk for developing necrosis of the mandible and maxilla.
 What is the pathophysiology of BRONJ?
What is the pathophysiology of BRONJ?
Although not completely understood, bisphosphonates are known to cause apoptosis of mature osteoclasts and osteoclast progenitor cells as well as strongly inhibit osteoblastic activity and cause a reduction in bone vascularity. The net effect appears to be an overall reduction in bone resorption and turnover, but also a reduced ability to heal, possibly resulting in osteonecrosis in some patients.
 How is BRONJ treated?
How is BRONJ treated?
Early-stage BRONJ is treated with oral hygiene care, antibiotic mouthwash, and oral antibiotics. Many patients respond to this treatment. Once BRONJ becomes advanced, with pathologic fracture, fistula, or osteolysis extending to the inferior mandibular border, surgical debridement or mandibular resection is indicated.
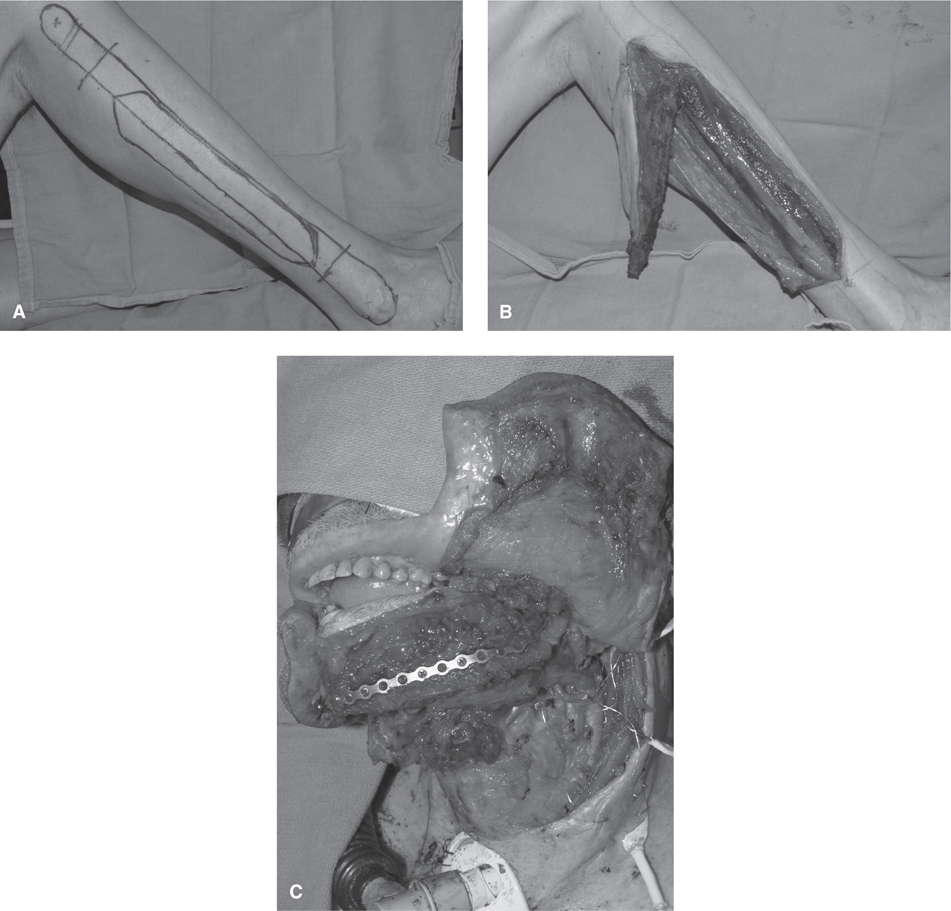
 What are some options for reconstructing composite mandibular defects that include a through-and-through cheek defect (see Figs. 80-1 to 80-3)?
What are some options for reconstructing composite mandibular defects that include a through-and-through cheek defect (see Figs. 80-1 to 80-3)?
Figure 80-1 Right fibula osteocutaneous free-flap skin markings (A), and completed harvest (B)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree