Mandible Reconstruction With Free Fibula Flap
JOHN BRADLEY TURNER
HENRY C. VASCONEZ
EDITORIAL COMMENT
The way to go in bony mandibular reconstruction. Soft tissue coverage is a must.
INDICATIONS
The free fibula flap has become the gold standard for reconstruction of the mandible in several clinical scenarios (1). It has been demonstrated that for defects greater than 6 cm, the flap has a significantly higher rate of success than nonvascularized bone grafts, especially in hostile environments (2). In patients undergoing either neoadjuvant or postoperative radiation
therapy, the most successful mandible reconstruction includes vascularized bone with the greatest advantage from the free fibula (3, 4). Other less common indications for mandibular reconstruction include congenitally or acquired mandibular hypoplasia, infected nonunions or chronic osteomyelitis of mandibular fractures, osteoradionecrosis or bisphosphonate-related osteonecrosis of the jaw (BRONJ), high-velocity penetrating injuries, and salvage reconstruction in instances of failed plate/soft-tissue reconstructions.
therapy, the most successful mandible reconstruction includes vascularized bone with the greatest advantage from the free fibula (3, 4). Other less common indications for mandibular reconstruction include congenitally or acquired mandibular hypoplasia, infected nonunions or chronic osteomyelitis of mandibular fractures, osteoradionecrosis or bisphosphonate-related osteonecrosis of the jaw (BRONJ), high-velocity penetrating injuries, and salvage reconstruction in instances of failed plate/soft-tissue reconstructions.
Versatility in flap design including the ability to capture muscle and fascia for bulk and resurface intra- and extraoral lining defects with skin
Excellent length (22 to 24 cm) and strength of bone
Dual blood supply to the bone allowing multiple osteotomies for contouring
Excellent pedicle length
Two-team approach to reconstruction
Minimal long-term morbidity of the donor site in low-demand patients
Reported disadvantages are few but include:
Lack of vertical height leading some to attempt “double barrel” approach
Unsightly lower leg donor scar
Occasional vascular variability
ANATOMY
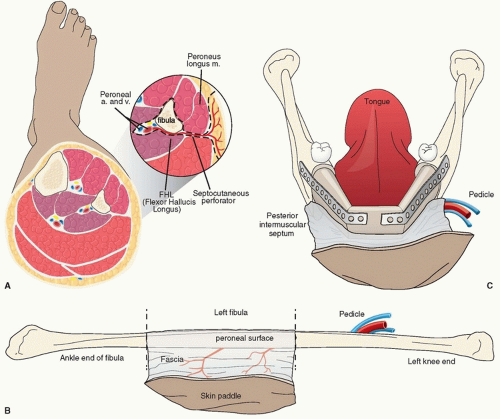
The fibula is the lateral, non-weight-bearing bone of the leg. The proximal and distal segments contribute to translational stability of the knee and ankle joints. The fibula flap is vascularized by the peroneal vessels, which bifurcate from the tibi-operoneal trunk (Fig. 213.1). This occurs 3 to 4 cm below the bifurcation of the popliteal and anterior tibial arteries. The pedicle remains within the deep posterior compartment of the leg until the distal third. The pedicle resides between the flexor hallucis longus posteriorly and the tibialis posterior anteriorly, with the fibula lateral to the vessels. As the vessels descend to
the fibula, they provide four to six segmental perforators to the bone, periosteum, and surrounding musculature allowing flexibility in tissue harvest and bony osteotomies. A nutrient branch of the peroneal artery, which enters the posteromedial fibula in the mid-diaphysis, provides endosteal circulation. The surgeon should be aware of the bifurcation of the common peroneal nerve at the fibular head proximally. Vascular abnormalities including arteriosclerotic disease and peroneal arteria magna are contraindications to this flap. Up to 15% of the population possess a peroneal arteria magna anomaly in which the blood supply to the foot is derived solely from the peroneal artery (6).
the fibula, they provide four to six segmental perforators to the bone, periosteum, and surrounding musculature allowing flexibility in tissue harvest and bony osteotomies. A nutrient branch of the peroneal artery, which enters the posteromedial fibula in the mid-diaphysis, provides endosteal circulation. The surgeon should be aware of the bifurcation of the common peroneal nerve at the fibular head proximally. Vascular abnormalities including arteriosclerotic disease and peroneal arteria magna are contraindications to this flap. Up to 15% of the population possess a peroneal arteria magna anomaly in which the blood supply to the foot is derived solely from the peroneal artery (6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree