Management of Pediatric Mandible Fractures
Nataliya Biskup
Brian S. Pan
DEFINITION
The pediatric facial skeleton is largely protected from fractures due to larger facial fat pads, more malleable bone, and a larger head-to-face ratio compared to that of adults.1
Mandible fractures are one of the most common pediatric facial fractures.2
Proper management of the pediatric mandible fracture is critical to limit disruptions in growth and dental development that can ultimately impact occlusion and function.
ANATOMY
The mandible is a unique bone composed of vertical and horizontal elements that form a U-shaped construct.
The growth pattern of the mandible occurs in a superior and posterior direction, resulting in a concomitant downward and forward displacement of the mandibular body and symphysis.3
From early childhood through adolescence, the inferior alveolar nerve changes in position as the canal migrates cephalically from the lingual inferior border of the mandible to a more superior position.
The preadolescent mandible has high osteogenic potential due to its rich blood supply from the inferior alveolar artery.
Following permanent tooth eruption, the medullary center of the mandible becomes more thickened and calcified.
PATHOGENESIS
The most common cause for facial injuries in children is motor vehicle collisions.
Sports-related injuries are the second most common cause of facial fractures.
These injuries occur more commonly in older children and in adolescence.
Childhood falls and assault/nonaccidental trauma are the least common causes.
Assaults occur most commonly in adolescence.
Males are twice as likely to sustain facial fractures compared with females.4
Condyle fractures are considered the most common type of mandible fractures followed by the symphysis, the body of the mandible, the angle, and lastly the ramus.
PATIENT HISTORY AND PHYSICAL FINDINGS
Depending upon the age of the child, an accurate history may not be available.
If patient compliance for an adequate exam is not possible, proceed with imaging and consider an exam under sedation.
Physical exam findings may include pain on palpation over the fracture site, malocclusion, decreased maximal incisive opening, jaw deviation with opening, loose teeth, and intraoral lacerations or ecchymosis.
Assess for paresthesia or anesthesia caused by injury of the inferior alveolar and mental nerves.
Chin abrasions and lacerations, coupled with blood in the external auditory canal, should raise suspicion for a condylar fracture.5
IMAGING
Although a panorex and plain films of the mandible can be obtained, a computed tomographic (CT) scan is the standard for imaging in the setting of facial trauma.
Cone beam CT (CBCT) scans are another means for accurately diagnosing facial fractures and have the advantage of exposing the child to less radiation.
NONOPERATIVE MANAGEMENT
Most pediatric mandible fractures are treated conservatively. Minor malocclusions will self-correct by the ability of the pediatric mandible to remodel and with minor orthodontic manipulations at skeletal maturity.
Children with deciduous and mixed dentition have a capacity for spontaneous occlusal readjustment after injury and treatment, as deciduous teeth are shed and permanent teeth erupt.6
Observation is indicated for:
Patients with condylar and subcondylar fractures
Mild malocclusions may be treated with soft diet and/or maxillomandibular fixation (MMF).
Minimally displaced fractures in the tooth-bearing mandible, namely, parasymphysis, body, angle. These areas are filled with developing tooth follicles, and thus operative intervention should be avoided if possible.
Start the patient on a mechanical soft diet, rigorous physiotherapy, avoidance of rigorous physical contact, and symptomatic pain control for 4 to 6 weeks. Arrange long-term follow-up to closely monitor mandibular growth.
SURGICAL MANAGEMENT
Position
Place the patient supine under anesthesia with nasotracheal intubation.
May consider sedation-only anesthesia, if only closed reduction is to be performed without MMF or with minimal MMF (such as an Ivy loop or lingual splint).
TECHNIQUES
▪ Closed Reduction and Maxillomandibular Fixation Options
Reduction
Reduce fractures manually as appropriate depending on fracture pattern and direction of displacement.
Verify adequate reduction by assessing occlusion while the patient is in centric relation. The pediatric mandible can tolerate a greater degree of variability in fracture reduction than the adult patient.
IMF Bone Screws
Obtain preoperative imaging (either CT scan or panorex) to identify positions of permanent and deciduous dentition.
Place screws in appropriate locations to avoid injury to dental structures:
Verify CT scan (ideally one with 2-mm cuts) to accurately identify location of tooth roots to avoid during screw placement.
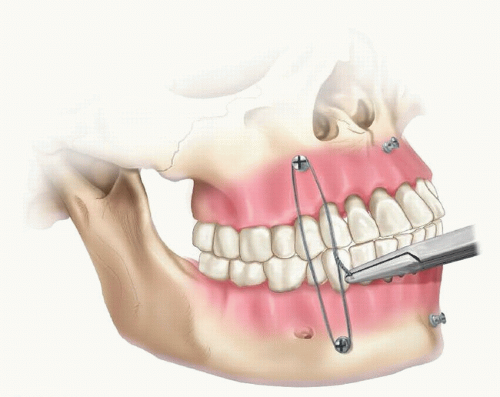
Use self-drilling, self-tapping bone screws, placing at minimum two within the mandible and two within the maxilla (TECH FIG 1):
Consider placement of a single midline screw in the mandible and one in the maxilla as this can often be adequate for fixation and ideal to avoid tooth roots.
Secure centric occlusion with 25-gauge wire loops.9
Arch Bar Application
Measure and apply the Erich arch bars of appropriate lengths to the maxilla and mandible to allow for all teeth to be wired.
Secure the arch bars with prestretched stainless steel 26-gauge wire, passing one end of the wire through the buccal gingiva above the arch bar:
The wire is then captured on the lingual side and passed through the lingual gingiva, capturing the wire on the buccal side of the tooth (TECH FIG 2A).
The ends of the wire are then twisted clockwise until the bar is tightly coapted to the tooth (TECH FIG 2B).
Repeat this process until the majority of the dentition is secured and the arch bars are stable.
Check the stability of the anchoring teeth with bimanual palpation.
Cautiously apply wires around deciduous teeth because they are more prone to extraction by wire tightening:
Note that primary teeth have short conical roots, wide cervical margins without a well-defined cingulum that makes securing the wire more technically challenging. Ideally, apply arch bars in patients older than 9 to 11 years of age.10
Cautiously, apply wires around erupting secondary teeth; periodontal ligaments are not well attached to the bone, and, therefore, the teeth can be extruded by the wire.
Use rigid wires or elastics to secure occlusion. Elastics may be better tolerated in children with equivalent outcomes as far as fracture healing and mandibular function (TECH FIG 2C).11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree