Escharotomies. The lines indicate the location for escharotomies. Note that it is important that the cut is deep enough to accomplish a tissue release. This needs to be specifically addressed at the areas marked, as it is more difficult to assess the right tissue depth at these locations, i.e., close to the major joints
C. Circulation
The circulatory status of the patient should be examined. It includes assessing the skin color, sensitivity, peripheral pulses, and capillary refill. Heart rate and blood pressure should also be included to confirm adequate organ perfusion. Be aware that heart rate effects need to be judged cautiously as it may also be affected by other reasons than hypovolemia, such as anxiety and/or pain. Blood pressure monitoring when done may be difficult, be aware of the risk for faulty or compromised measurements by, e.g., deep circumferential burns. In cases the peripheral circulation in the extremities is compromised, consider early escharotomies and invasive blood pressure measurements (See Fig. 11.1).
D. Disability
The burn injured patient during “normal” conditions in the acute phase should not have an altered level of consciousness (LOC) even in cases of very severe burns. The LOC should be assessed, e.g., by the Glasgow Coma Scale (GCS). If the level of consciousness (LOC) is altered, suspect other underlying processes such as other trauma, carbon monoxide and/or cyanide intoxication, hypoxia, e.g., especially in a closed space and where fire is fierce, or other medical conditions such as stroke or diabetes.
E. Expose and Examine
Patients with >30% TBSA obtain two large bore, indwelling venous catheters and a suggested simplified prehospital fluid management plan may be as is presented in this Table (11.1)
A simplified fluid management plan | |
≤5 years | 125 mL LR/h |
6–13 years | 250 mL LR/h |
≥14 years | 500 mL LR/h |
11.2.2.2 Secondary Assessment
The complementary second assessment is undertaken rapidly after the first assessment and it is aimed at examining the patient thoroughly from head to toe, mainly in order to rule out other more important injuries that may pose a danger to the patient. One important point is that this examination needs to be undertaken in detail as the burn injury often is the most prominent injury and it may lead to that other injuries may be overlooked. If the assessment is done at larger facilities and there is a suspicion of other concomitant trauma, a regular trauma assessment algorithm may be undertaken and involving, e.g., ultrasound scan abdomen and/or (complementary) whole body CT scan.
- 1.
Circumstances of the burn. Where and when did it happen—what were the injury mechanisms (scald, flame, chemical, or electrical). Especially the factors, heat level (degrees) and exposure time (seconds) may signal the risk for deep injuries. Indoor accident and risk for inhalation injuries. Are other injury mechanisms present and relevant?
- 2.
Medical history. Previous or associated illnesses (diabetes; hypertension; other heart, lung, or kidney disease)— Ongoing medical treatment, alcohol use or other (abuse), allergies. Time for last oral fluid or food intake. The tetanus immunization status—need for complementary injections?
11.2.2.3 Fluid Treatment
Crystalloid-based protocols | |
Parkland | Ringer’s lactate/acetate 2–4 mL/kg/TBSA%; half of the fluid during first 8 h |
Children: Ringer’s lactate/acetate 3–4 mL/kg/TBSA% | |
Modified Brooke | Ringer’s lactate/acetate 2 mL/kg/TBSA% |
Colloid-based protocols | |
Evans | NACl 1 mL/kg/TBSA%+ colloid 1 mL/kg/TBSA%+ 2000 mL glucose solution (5%) |
Brooke | Ringer’s lactate/acetate 1.5 mL/kg/TBSA%+ colloid 0.5 mL/kg %+ 2000 mL glucose solution (5%) |
Slater | Ringer’s lactate/acetate 2000 mL/24 + fresh frozen plasma 75 mL/kg/24 h |
Dextran-based protocols | |
Demling | Dextran 40 in NaCl (2 mL/kg/h in 8 h) + Ringer’s lactate/acetate in sufficient amounts to induce a urine volume of 30 mL/h + fresh frozen plasma (0.5 mL/kg/h from 8 to 26 h post burn) |
Hypertonic protocols | |
Monafo | 250 mEq Na/L. Amounts provided to induce a urine output of 30 mL/h |
Warden | Ringer’s lactate + 50 mEq sodium bicarbonate (total 180 mEq) during the first 8 h to induce a urine output of 30–50 mL/h. Thereafter Ringer’s lactate with the same urinary output goal |
The Parkland protocol
Adults |
Ringer’s lactate/acetate 2–4 mL/kg/TBSA%. 50% provided during the first 8 h. The remaining fluid during the following 16 h |
Children |
Ringer’s lactate/acetate 3–4 mL/kg/TBSA%. 50% provided during the first 8 h. The remaining fluid during the following 16 h. Normal 24 h fluid needs are added to this as glucose solution |
It is important to stress that neither too little fluid nor too large fluid volumes in relation to the needs should be provided as it will lead to less successful results [33]. The needs vary largely between injuries and patients underlining the need for close surveillance and follow-up. In general and presently, in cases of less successful fluid resuscitations most often too large fluid volumes have been provided [30]. Too large fluid volumes will lead to deepening of the burn wound and secondary complications from other body compartments such as generalized large edema including cerebral, pulmonary edema and compartment situations, most importantly abdominal compartment syndrome [33]. Especially if using central circulatory endpoints rather than urine output during the first 12–18 h, such risk is higher [34]. Using the parkland formula, the patients appear “hypovolemic” as examined by central circulation techniques, e.g., echocardiography in the very early part of the resuscitation period [35, 36].
There are situations where larger fluid needs may be present. In general it has been claimed especially for inhalation or electrical injuries and in cases of a delayed start of fluid treatment. In the case of inhalation injuries the data supporting larger fluid needs are older and in newer investigations smaller effects of inhalation injury on the fluid needs have been seen [30]. In electrical injuries, the total tissue damage may be larger despite that the skin burn is less extensive. Other instances where larger fluid volumes are called for are in cases of high voltage electrical injuries or crush injures or when myo- och hemoglobinemia is present. Under these circumstances, an increased diuresis and alkalinization of the urine is recommended. The diuresis should reach 1–2 mL/kg/h (adults) and the pH of the urine should be kept alkaline preferably around or above 7. This is accomplished by adding sodium bicarbonate solution to the resuscitation fluids. This strategy should be continued as long as the pigments are present in the urine.
11.2.2.4 Burn Wound Evaluation
Most often the first burn wound evaluation is made under the heading “exposure” in the primary survey, at, e.g., the accident. A more thorough examination is then be made after the second survey. In evaluating the wound, it is important to have it adequately exposed and cleaned from debris and blisters, the latter situation calls for good analgesia or is done during general anesthesia. The risk of hypothermia should always be addressed. The wound evaluation is done mainly in two aspects, to determine, the depth and total percent body surface area injured (TBSA%). The depth is mainly important as it affects the treatment (surgical excision or not) and the TBSA% is important for the prognosis. TBSA% (including depth) is together with the age of the patient and the prevalence of inhalation injury, the most important prognostic factors for the injury. This will govern prognosis and also the fluid treatment.
Burn Wound Depth
How deep into the skin the injury progresses is dependent on several factors. Firstly, it depends on the thermal energy transferred to the tissue. This depends on the temperature and the exposure time; high temperature and longer exposure times increase the risk for significant injuries. The energy transfer process is further affected by the type of transfer, e.g., convection transfers more energy, and this is counteracted by the ability of the tissue to withstand the temperature (thicker skin—better resistance) or dissipate the heat (higher blood flow reduces the injury). In practice, this is exemplified by the lower risk for injuries on the back, in palms and soles with their thicker nature and the higher risk in elderly and children with their generally thinner skin.
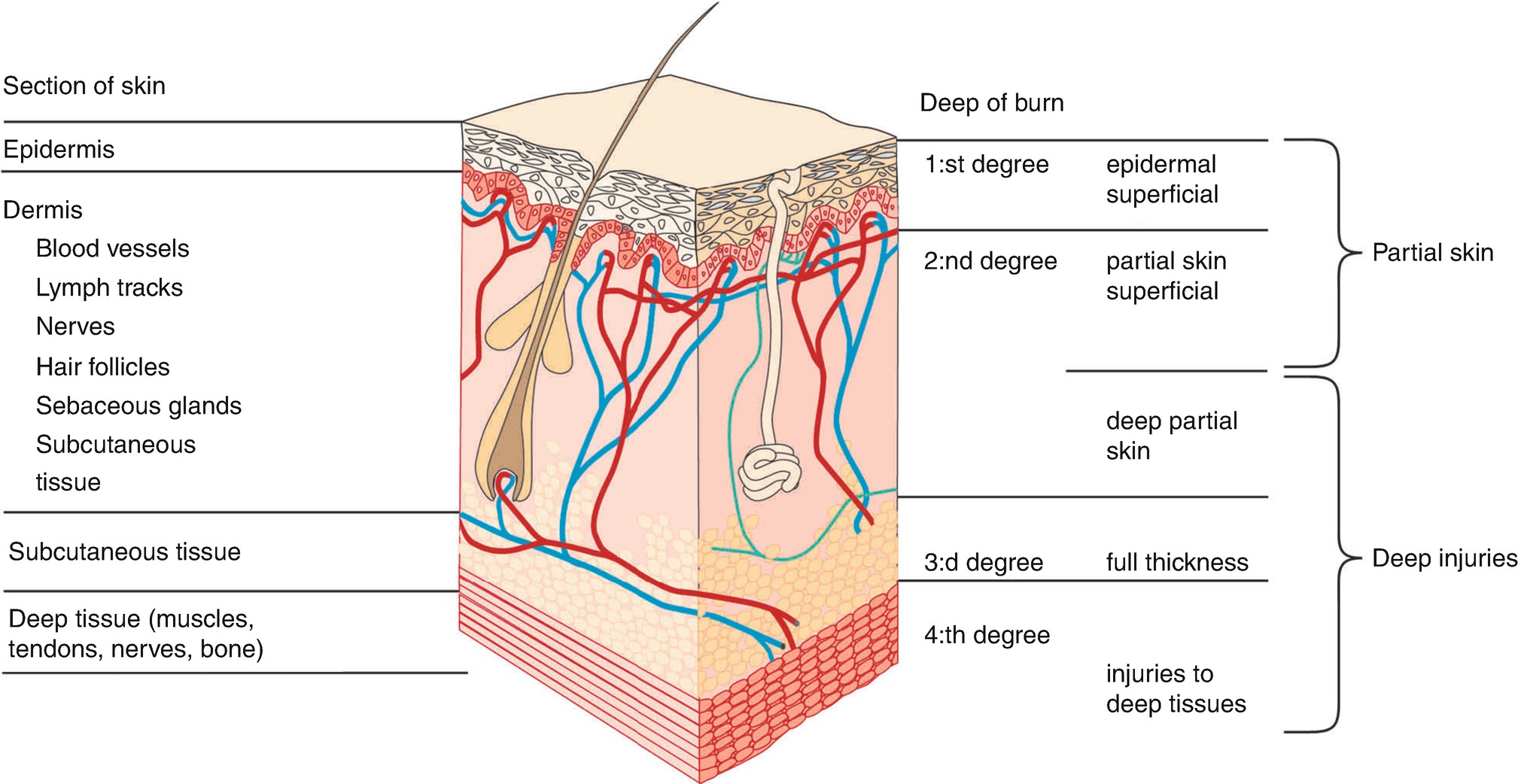
Burn wound. Skin anatomy in relation to burn wound depth terminology

Different burn depths (a–c) (Photos). (a) Superficial dermal burn wound—Partial thickness wound. (b) Deep dermal burn wound—Full thickness wound. (c) Full thickness wound extending down subdermally

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








