Compound finger flexion using distance between the fingertip and palmar crease as a measurement of finger ROM at the metacarpophalangeal and interphalangeal joints. Source: Ellis and Bruton, 2002 [25]
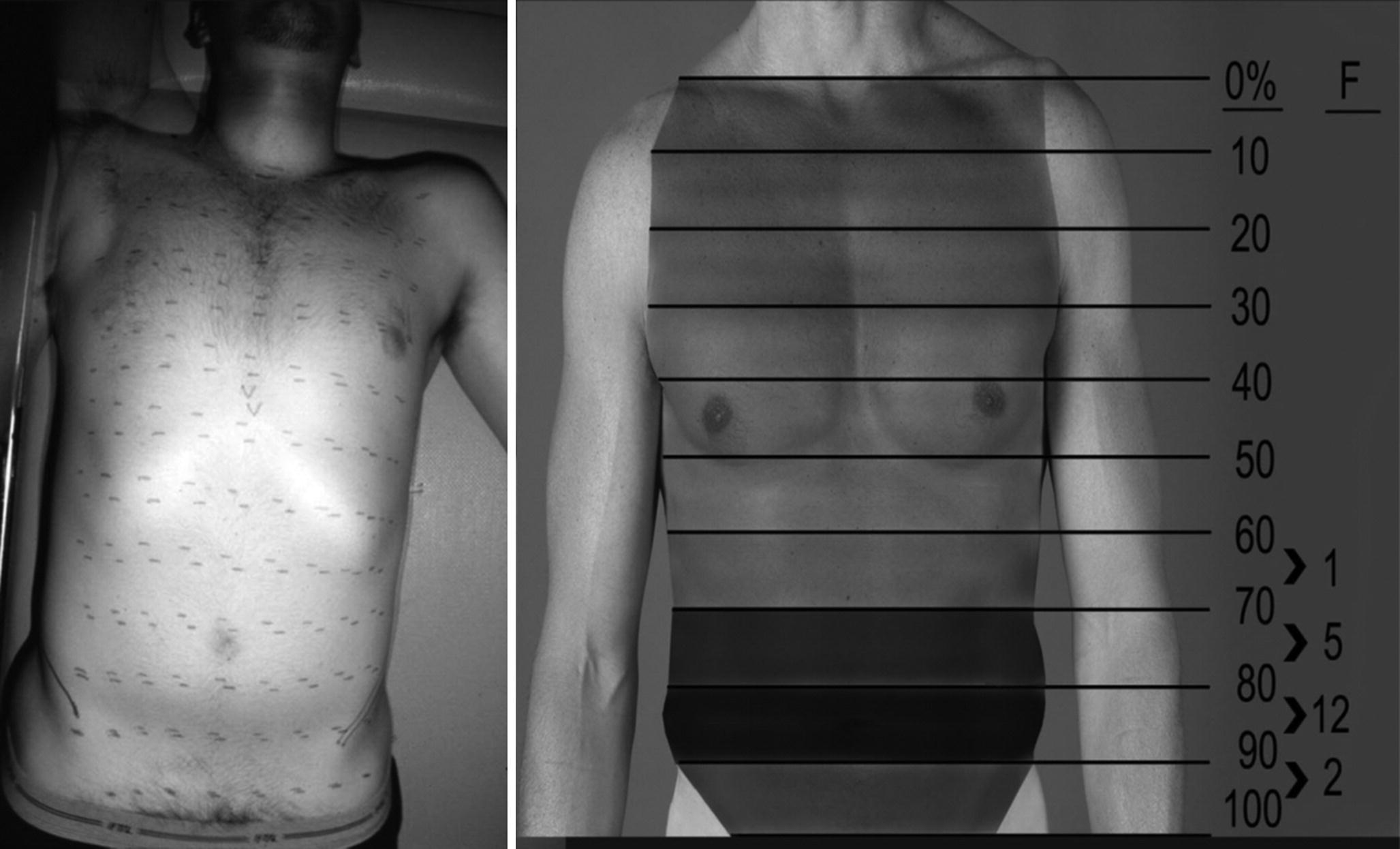
Cutaneous functional units . Skin markings are spaced at 2 in. increments on the anterior torso. The image to the left is a double exposure photograph demonstrating the movement of markings indicating skin recruitment during shoulder abduction. The image on the right identifies the size of the soft tissue recruitment in normal individuals; the majority of the individuals tested (14 of 20) recruited soft tissue to at least the umbilicus. Source: Richard et al., 2009 [27]
Following burn injury, this pliable skin is replaced with scar tissue with reduced elasticity. Not surprisingly, the volume of CFUs affected by burn injury has shown value in predicting the development of burn scar contracture in survivors [28]. As a result, burn rehabilitation providers should be mindful of not only the impact of local injury to a joint, but the compound effect of scarring to the pool of soft tissue surrounding the joint in a wider area involved in full joint motion. The risks of developing specific issues must also be considered, such as webbing between digits, microstomia (loss of opening volume of the mouth), ectropion (inversion of the eye lid), and lagophthalmos (incomplete eyelid closure) [6, 29].
Frequently, the methods employed for patients at varying stages of recovery need to evolve over time from the onset of injury. In early stages , techniques must accommodate bulky dressings, acute pain, ongoing medical interventions such as central lines, and patients with impaired level of consciousness and deconditioning. In later stages, these factors lessen, however, as patients regain independence contracture prevention methods may become more difficult to tolerate and may compete with functional use of limbs, but can be replaced with more active and functional techniques of restoring and maintaining ROM.
28.2.1.1 Mobilization
Early mobilization is key to limit the impact of bed rest, reduce adverse events, and to begin the process of functional recovery and contracture prevention. Specific to the post-grafting period, mobilization must balance concerns for early graft loss with the areas above. In many cases, surgeons will require a period of immobilization prior to resuming activity. Early post-operative mobilization has been proposed, but medical literature to guide specific decision-making are limited [30, 31]. Recent practice guidelines have been proposed from the burn rehabilitation community regarding early ambulation for patients with smaller grafts (less than 300 cm2) which are not overlying joints and that can be effectively braced and have pressure dressings applied and can serve as a starting point for team decisions regarding early post-operative therapy [30].
28.2.1.2 Positioning
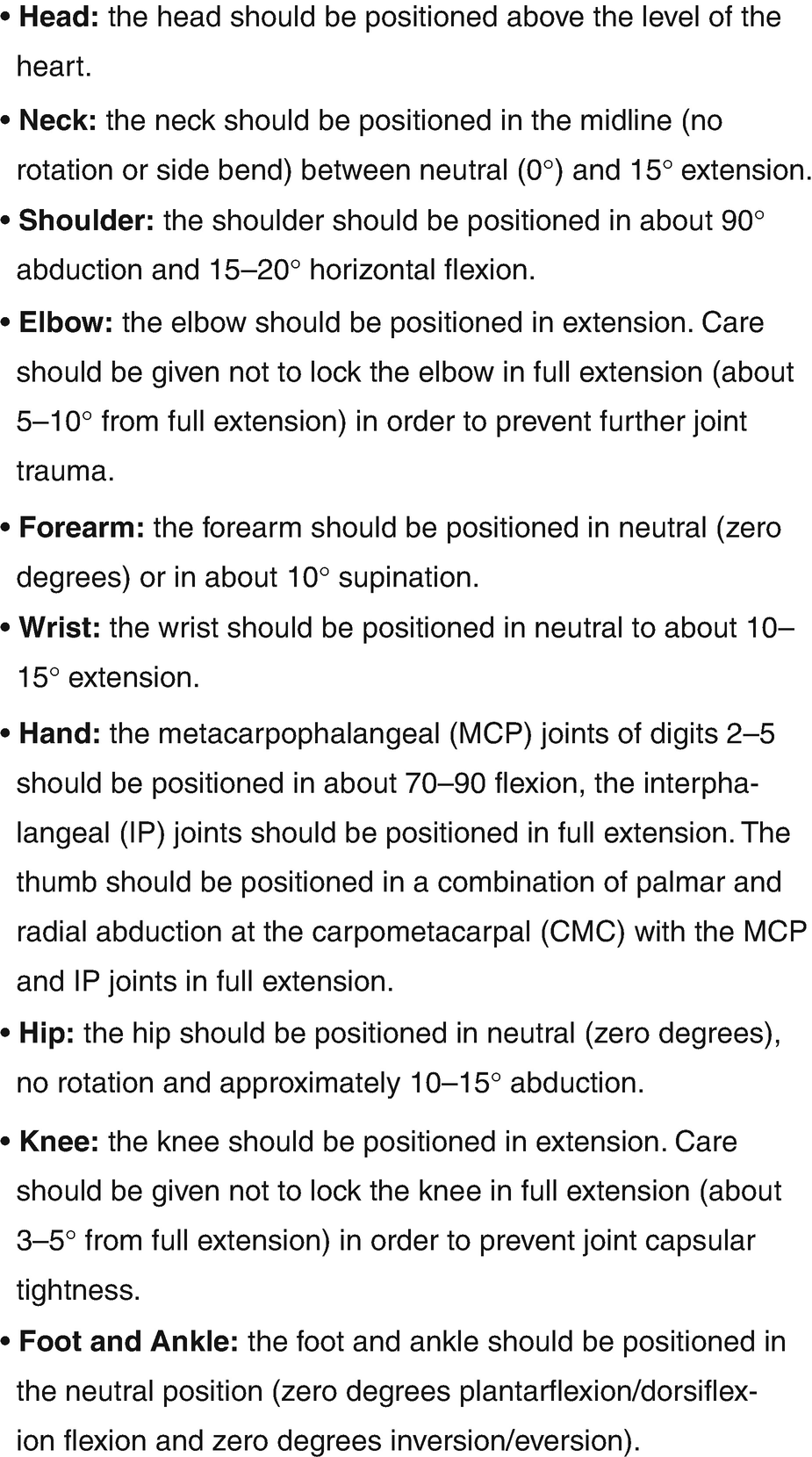
Clinical practice guidelines for joint positioning following burn injury. Source: Serghiou et al., 2016 [32]
28.2.1.3 Splinting
Splinting is frequently used to provide prolonged low-load stretching, particularly during periods of early graft fragility, reduced level of consciousness, but also with focused application in later care. A large range of splints have been employed in burn recovery to prevent and treat losses in ROM through prolonged, passive stretching, though scientific data supporting use of specific splint designs is limited, as are outcomes studies evaluating specific approaches and prescriptions of use [33–36]. While there are theoretical concerns regarding the influence of prolonged stretch on the development of contracture during wound healing, recent analyses have found substantially decreased odds ratios of developing contracture through splint usage as a therapy tool [37, 38].
28.2.1.4 Stretching and Scar Massage
Mechanical stretching and massage of scar tissue to improve extensibility are also traditional approaches to burn-associated contracture. Like other interventions, specific medical literature to guide technique and outcomes are limited but suggest benefit for burn recovery [39, 40]. Stretching has the theoretical advantages of being focused on specific areas of ROM losses, progressive throughout a treatment to continually advance ROM gains, and can be integrated into functional or recreational activities over time. Scar massage is typically deferred for a few weeks following skin grafting to prevent early graft shearing or superficial injury, but a number of techniques exist as potential tools once skin resilience has improved.
28.2.1.5 Functional Impact of Contracture
The specific functional impairment from contracture remains a complex issue. At face value, the basic relationship is simple—as ROM decreases, impairment is expected to increase. However, injuries of some locations on the body (e.g., hands) have much larger functional implications than a simple size and depth of burn for another location (e.g., torso). Predicting the impact of specific contractures is also challenged by the potential for multi-joint ROM losses leading to compound movement issues [41]. Finally, the functional needs of individual patients and baseline ROM may also vary.
28.2.2 Edema
Inflammation and wound healing lead to formation of edema particularly in the acute phase of care. Functionally, this can hinder mobility and cause pain particularly in dependent areas and can factor into contracture [42]. Elevation of dependent limbs above the heart can reduce edema and can be initiated early post-injury, and edema in the head and face can be managed by elevating the head of the bed. Compressive dressings and splinting can reduce edema while preventing contracture and become increasingly important for the lower extremities as patients mobilize [43]. Edema can be particularly limiting in the setting of hand injuries, and early graded pressure approaches can improve pain and ROM. In later stages, compression gloves can be employed. Active muscle contraction and functional use of the hand should be encouraged to promote edema mobilization.
28.2.3 Scar Hypertrophy
Scar formation is common following burn injury and is associated with many factors ranging from depth of injury, complications, age, and genetic background [44]. In many cases, scarring becomes hypertrophic, with progressive increases in scar height and thickness, altered pigmentation, erythema, and reduced pliability. During the acute phase of care, hypertrophic scarring is typically not present given the timeframe of development, however, acute care rehabilitation team members should be aware of the fundamentals of burn scar hypertrophy and its management.
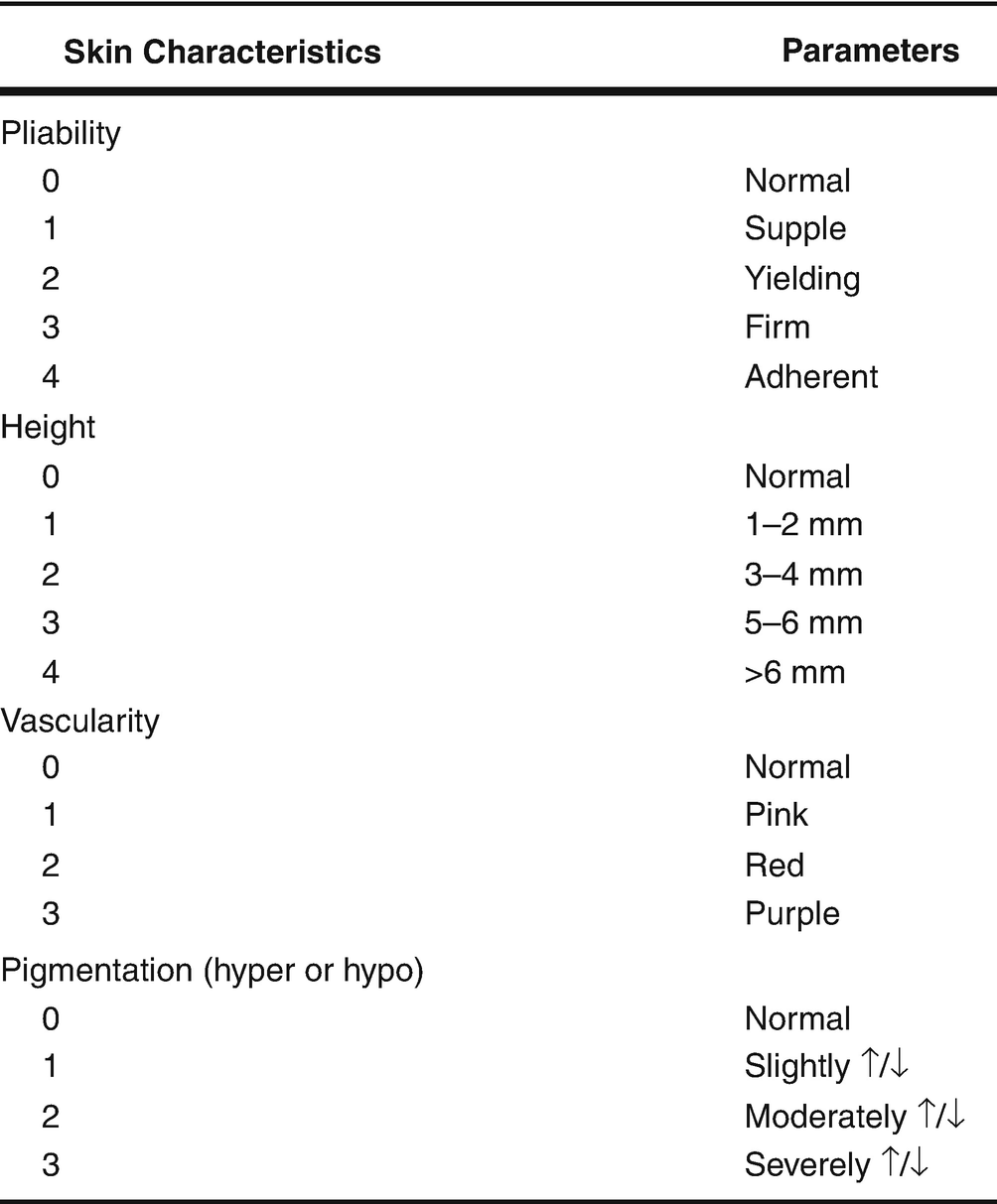
The two primary means of treatment are custom pressure garments and silicone gels and sheets. Pressure garments influence the collagen remodeling phase of wound healing. While the exact mechanism of action is unknown, it may be related to impact on local hydration, circulation, or inflammation [48]. Recent reviews of the available medical literature have found that pressure therapy is effective for scar height and erythema, less clearly associated with improvements in scar pliability and joint range of motion, and less likely to impact pigmentation or scar maturation [8]. Pressure garments should be custom fitted, employed as soon as wound healing allows application without adverse effect on dressings or injury from shearing, and worn 23 h per day for 12 months or until scar is mature [8].
Silicone is hypothesized to mitigate hypertrophy through mechanisms such as occlusion and hydration of the skin [49]. Recent practice guidelines for the use of silicone gels and sheets have noted the following: silicone should be applied in cases likely to form hypertrophy scars once the wound has re-epithelialized, the benefit is likely only for immature scars, and silicone gels may have reduced adverse reactions compared to gel sheets [50].
28.3 Skin Physiology Following Burn Injury
The skin is the largest organ in the human body, and it plays a range of physiological roles including the sense of touch, temperature regulation, and moisturization of the skin. The majority of these functions occur through dermis-derived structures that are compromised with deep tissue injury and which typically remain impaired despite split thickness or sheet grafting. Long-term physiological skin changes from deep dermal injury should be considered in early recovery and patient education.
The loss of distal nerve endings in the dermis leads to an increased threshold for detecting light touch, cold, and heat and a subsequent loss of perceived skin sensation and these changes typically persist long term [51, 52]. Temperature regulation occurs through the skin both through vascular shunting of blood via vasodilation and constriction as well as sweating and piloerection. Following skin grafting, these processes remain impaired with consequent decreased heat and cold tolerance relative to the size of skin injured [51, 53] though heat acclimation exercises may improve heat tolerance over time [54]. This is of particular importance given the benefits of strength training and aerobic conditioning in burn recovery [55].
Superficially, the loss of sebaceous glands and oil production may seem trivial, but problems with pruritis, dry skin, and need for artificial lubrication through lotion remain some of the most common long-term complaints following major burn injury [52]. Beyond the need for early education, alterations in skin oil may need to be considered for activities and employment that are accompanied by exposure to chemical irritants, dry heat, or cleaning materials.
28.4 Burn-Specific Complications
28.4.1 Peripheral Nerve Injury
The incidence of peripheral nerve injury in burn injury ranges widely in the medical literature depending on the inclusion criteria regarding the severity of burn injury [56, 57]. In those categorized as major burn injury, research has found an incidence of 11% and associations with larger burns, more days on mechanical ventilation, increased surgical requirements, and longer periods of hospitalization [56].
Focal peripheral nerve injury typically occurs in the region of the burn injury, but can also arise as a consequence of critical illness, pressure from positioning or dressings, edema, or compartment syndrome. Focal injury incidence typically follows that of entrapment neuropathies, with the median, ulnar, and peroneal nerves most often at-risk and the upper extremity a more common site than the lower [56–58].
28.4.2 Heterotopic Ossification
Heterotopic ossification is the formation of pathological, ectopic bone in soft tissue and it is associated with a wide range of conditions ranging from spinal cord injury and traumatic brain injury to bony fractures and joint replacement surgeries. In the setting of burn, it is a rare complication associated with larger total body surface area of injury, and most often occurring adjacent to the elbow joint [59]. While rare, the rehabilitation implications of heterotopic ossification can be severe, with patients experiencing increased pain, loss of ROM, and nerve entrapment particularly involving the ulnar nerve. These changes may often be first noted during therapy interventions. Described medical interventions for prevention and treatment have included non-steroidal anti-inflammatory drugs, bisphosphonates, and radiation, and many patients require surgical resection of heterotopic ossification once the process has matured and the risk of recurrence has diminished months after onset.
Specific to rehabilitation, management of heterotopic ossification is ill defined. Early studies and scientific theories raised concerns that early, aggressive mobilization may be associated with the development and progression of heterotopic ossification [60]. However, in many cases the absence of early mobilization in the at-risk population would be expected to lead to soft tissue contracture and, once present, heterotopic ossification can cause severe upper extremity disability present for prolonged periods before patients can become candidates for surgery. Given these competing demands, there may be a role for ongoing mobilization despite concerns with heterotopic ossification, but the timing, intensity, and safety parameters of doing so remain unclear [60–62].
28.4.3 Electrical
Electrical injuries can cause all of the complications and therapy concerns discussed in this chapter, but due to the potential for deep tissue injury from electrical current travelling through the body can cause a wide range of additional pathology with functional implications. Electrical injury is associated with fourfold increased risk of peripheral nerve injury, spinal cord injury and dysfunction, increased rates of limb amputation, ophthalmological complications including cataract formation, and a wide range of neurological and psychological manifestations [56, 63–68].
Complicating these issues is the fact that in many cases development of complications can continue to progress for weeks or months following injury. This may be due to the varied nature of the injury itself, with trauma occurring not only from thermal energy, but also due to vascular injury and pathological changes at a cellular or subcellular level [69], such as lasting cell membrane damage and protein denaturation. In addition—and likely also due to the unusual nature of damage from electrical injury—routine medical testing may fail to identify focal pathology [70]. As a result, rehabilitation providers should have a low index of suspicion for electrical injury-associated complications both at onset and over time, and consider the wide range of potential areas of tissue injury when reviewing patient complaints.
28.5 Summary
Early rehabilitation efforts are a key component of acute burn management. Burn caregivers should be aware of the short- and long-term impact of wound maturation and scarring and the consequences for functional recovery and quality of life, as well as techniques for preventing and treating burn-associated impairments. Successful programs should consider an evolution of recovery from the intensive care unit to the community and incorporate support and planning for sustained prevention of complications and long-term activity goals.
Summary Box
Patient assessment and goals
The impact of burn rehabilitation
Quality of life and long-term recovery
Functional complications of burn injury: contracture, edema, and scar hypertrophy
Skin physiology following burn injury
Burn-specific complications: peripheral nerve injury, heterotopic ossification, electrical injury
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








