What is the most frequent displeasing effect you see when performing lower eyelid blepharoplasty? What surgical approach do you most frequently use when performing lower eyelid blepharoplasty? How much skin removal of the lower eyelids? When performing lower lid blepharoplasty, what is your preferred method of managing pseudoherniated fat? If you perform midface lifting during blepharoplasty, what approach do you use? Analysis: Over the past 5 years, how has your technique or approach evolved or what is the most important thing you have learned in doing blepharoplasty?
Shan Baker, Keith LaFerriere, and Wayne Larrabee address questions for discussion and debate:
- 1.
What is the most frequent displeasing effect you see when performing lower eyelid blepharoplasty?
- 2.
What surgical approach do you most frequently use when performing lower eyelid blepharoplasty?
- 3.
How much skin removal of the lower eyelids?
- 4.
- 5.
If you perform midface lifting during blepharoplasty, what approach do you use?
- 6.
What is the most frequent displeasing effect you see when performing lower eyelid blepharoplasty?
Baker
In my experience, the most common displeasing effect following lower eyelid blepharoplasty in patients operated on by other surgeons is lower eyelid retraction. In addition, in older patients with considerable loss of soft tissue volume of the midface, I usually see hollowing of the lower eyelids. This finding is presumably related to fat excision during blepharoplasty. I prefer fat preservation when performing lower eyelid blepharoplasty. My usual approach is advancement of fat and redundant septum over the inferior bony orbital rim into a subperiosteal space. The most common displeasing feature I identify in my personal patients is persistent visibility of pseudoherniated fat, particularly in the lateral compartments. In addition, in elderly patients with atrophic soft tissue cover in the periorbital region, the mobilized fat can sometimes produce a subtle contour fullness in the infraorbital zone.
LaFerriere
- •
Conjunctival edema , most commonly seen with a transconjunctival incision and fat repositioning: Steroid eye drops will usually aid in resolution, but rarely a small conjunctival unroofing is necessary ( Fig. 1 ).
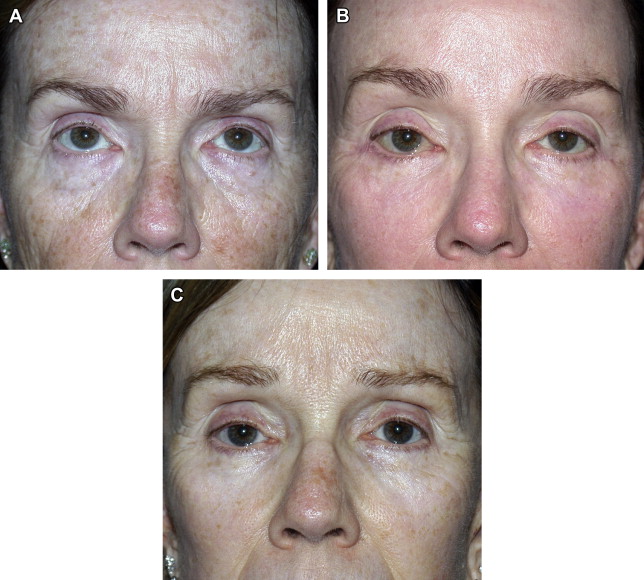
Fig. 1. LaFerriere
( A ) Preoperative view. ( B ) Four weeks after skin/muscle flap blepharoplasty with lateral retinacular repositioning canthoplasty with persistent conjunctival edema right eye. ( C ) Three months postoperative image with resolution of the conjunctival edema and normal lid positioning.
( Courtesy of Keith LaFerriere, MD, Springfield, MO. © Keith LaFerriere.)
- •
Immobility of the lower eyelid following a transconjunctival approach with fat repositioning: The lower lid should be able to be elevated to the superior limbus; but at times, there is restriction of the lid on the upward gaze. This effect almost always resolves with time and massage, but rarely triamcinolone 5 mg/mL injected into the middle lamella is needed. I have not seen a permanent problem with this ( Fig. 2 ).

Fig. 2. LaFerriere
Patient 2 weeks after transconjunctival lower blepharoplasty with fat repositioning demonstrating restriction on upward mobility. This effect has always resolved over time, in my experience.
( Courtesy of Keith LaFerriere, MD, Springfield, MO. © Keith LaFerriere.)
- •
Incomplete excision of the temporal fat pad , which can be seen as a lateral bulge: Meticulous removal of the temporal fat pad can greatly reduce this occurrence ( Fig. 3 ).
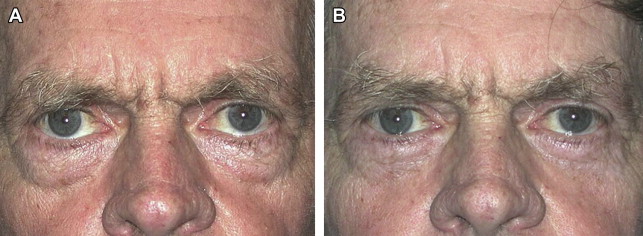
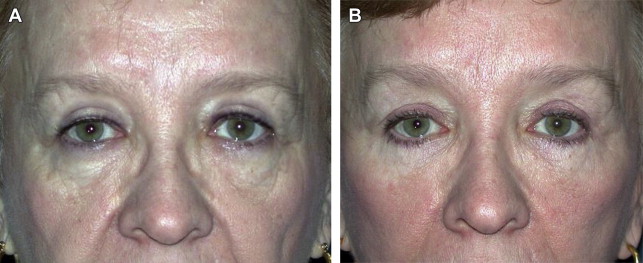
Fig. 3. LaFerriere
( A ) Preoperative image. ( B ) Postoperative transconjunctival lower blepharoplasty with fat repositioning and lateral retinacular repositioning canthoplasty showing incomplete removal of the temporal fat pad.
( Courtesy of Keith LaFerriere, MD, Springfield, MO. © Keith LaFerriere.)
- •
Mild lateral rounding of the lid with the skin/muscle technique: This effect can occur even if the flap is tacked laterally to the orbital rim. I think this is often related to the delayed return of function of the pretarsal orbicularis and usually resolves over time.
- •
Epidermal inclusion cysts in the incision lines secondary to suture tracts: These cysts are easy to correct but are a nuisance.
Larrabee
There are several problems that may be accounted for after lower eyelid blepharoplasty, including dry eyes, hematoma formation, globe injury, infection, asymmetry, and lower eyelid malposition (ie, retraction, ectropion). The techniques used in lower eyelid blepharoplasty have a major impact on the type of complication that may occur after surgery. For instance, the transconjunctival approach has a much lower rate of eyelid malposition ; the use of lateral canthal support significantly decreases the occurrence of scleral show and ectropion. The most frequent long-term complication in skin muscle flap blepharoplasty is lower eyelid malposition, whereas persistent fat is most common in the transconjunctival approach. The most frequent problem I see after blepharoplasty is scleral edema, which almost always resolves spontaneously in a relatively short time. Of the 2 choices provided here, minor contour irregularities or scar visibility are most frequent. I am quite conservative and, therefore, the issue is usually persistent pseudoherniated fat, most commonly in the lateral fat pocket. If I use the pinch technique, I am focused on keeping the lateral scar subciliary because there is a tendency for it to move a little inferior in this area. Retraction of the lid is either caused by excess skin excision or scarring in the middle lamella together with preoperative lateral canthal laxity. If a conservative approach is used during the skin-muscle flap technique, the risk decreases. It is uncommon to see eyelid retraction when performing a transconjunctival approach unless the middle lamella or, more specifically, the septum is damaged.
What surgical approach do you most frequently use when performing lower eyelid blepharoplasty?
Baker
The most common approach I use in performing lower eyelid blepharoplasty is a fat-preservation blepharoplasty accomplished by first performing a skin pinch to precisely excise dermatochalasis. A skin muscle flap is dissected to the inferior bony orbital rim. The arcus marginalis is incised, and a subperiosteal pocket is dissected from beneath the tear-trough area laterally to the malar eminence. The septum is incised at the level of the inferior bony orbital rim near the medial canthus extending laterally to the attachment of the arcuate expansion. Redundant septum and fat are advanced as a composite flap into the subperiosteal space and secured in place. The septum is incised over the lateral compartment and fat is removed.
LaFerriere
The decision regarding the technical approach to lower blepharoplasty depends on the clinical findings at the time of consultation. The factors that enter into the choice of technique are multiple, including the sagittal bony orbital relationship to the cornea (vector anatomy), the extent of fat pseudoherniation, the amount of dermatochalasis present, the lid tone and position, and the presence of malar bags. Depending on the findings in each individual case, all of the aforementioned procedures are in my armamentarium.
The most frequent approach used is transconjunctival because it maintains the integrity of the orbicularis muscle, gives equal exposure to the to the fat pads as do the external techniques, and allows for a skin pinch and/or laser resurfacing to correct the dermatochalasis. If the skin excess can be eliminated by a pinch excision alone, carbon dioxide (CO 2 ) or erbium laser resurfacing is not used. If fine rhytids are present, or if skin excess is minimal, laser resurfacing alone is performed ( Fig. 4 ). Skin excess and fine rhytids are treated with both skin pinch and laser resurfacing. This approach is also effective in patients who have very mild lid laxity because a canthoplasty can be avoided because the main supporting structures of the lid are maintained.
The skin/muscle external approach is used when there is extensive skin excess, festooning of the skin and orbicularis muscle, or malar bags ( Fig. 5 ). Extending the skin/muscle flap in the suborbicularis oculi fat (SOOF) layer can improve malar bags in some instances ( Fig. 6 ). Laser resurfacing can be used if fine rhytids are present.
If there is no fat pseudoherniation present and predominantly skin excess exists without malar bags, a skin-flap lower blepharoplasty is very effective in these patients. If there is any form of nicotine use, this technique is contraindicated, as is laser resurfacing at the time of surgery. This approach is by far the least frequently used approach in my practice.
Larrabee
I tailor my approach to the specific patient. The variables include a history of previous surgery; orbital anatomy, including the presence of a negative vector; skin texture and elasticity; lid tone; amount and location of pseudoherniated fat; presence of hypertrophic or lax orbicularis oculi muscle; and patient preferences. There are several techniques that may be used for lower eyelid blepharoplasty. These techniques include the skin-only approach, the skin-muscle flap, and the transconjunctival approach with or without skin excision. My most frequent approach is a transconjunctival blepharoplasty with a skin pinch. This technique allows for more controlled wound healing and, because the septum is left intact, has a lower tendency for scleral show or ectropion to develop. Fat is managed as discussed later, with either excision or transposition. Resurfacing is performed in patients who desire to address their rhytids simultaneously. Frequently, these patients are undergoing a full-face laser resurfacing in addition to the treatment of the lower lid. I currently use both active and deep fx laser resurfacing with the Coherent system. TCA (Trichoroacetic Acid) peels (35%) and full phenol peels (88%) are still useful techniques for lower lid resurfacing in my patients. I still use a skin muscle flap blepharoplasty in special situations. The major indication for this technique is hypertrophic orbicularis muscle or an extremely lax orbicularis muscle where I wish to excise redundancy and tighten the lower lid. I will also use a skin muscle flap in secondary or revision cases where a skin muscle flap was used in the primary operations. In these cases, there are sometimes scar adhesions and other problems best addressed in the same plane of dissection.
What surgical approach do you most frequently use when performing lower eyelid blepharoplasty?
Baker
The most common approach I use in performing lower eyelid blepharoplasty is a fat-preservation blepharoplasty accomplished by first performing a skin pinch to precisely excise dermatochalasis. A skin muscle flap is dissected to the inferior bony orbital rim. The arcus marginalis is incised, and a subperiosteal pocket is dissected from beneath the tear-trough area laterally to the malar eminence. The septum is incised at the level of the inferior bony orbital rim near the medial canthus extending laterally to the attachment of the arcuate expansion. Redundant septum and fat are advanced as a composite flap into the subperiosteal space and secured in place. The septum is incised over the lateral compartment and fat is removed.
LaFerriere
The decision regarding the technical approach to lower blepharoplasty depends on the clinical findings at the time of consultation. The factors that enter into the choice of technique are multiple, including the sagittal bony orbital relationship to the cornea (vector anatomy), the extent of fat pseudoherniation, the amount of dermatochalasis present, the lid tone and position, and the presence of malar bags. Depending on the findings in each individual case, all of the aforementioned procedures are in my armamentarium.
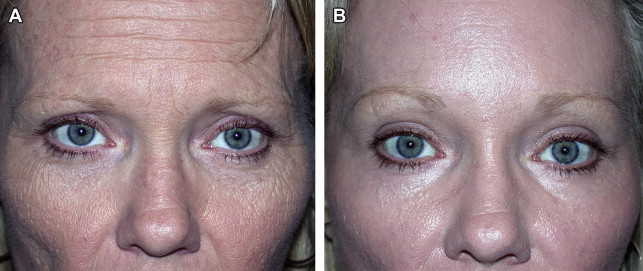
The most frequent approach used is transconjunctival because it maintains the integrity of the orbicularis muscle, gives equal exposure to the to the fat pads as do the external techniques, and allows for a skin pinch and/or laser resurfacing to correct the dermatochalasis. If the skin excess can be eliminated by a pinch excision alone, carbon dioxide (CO 2 ) or erbium laser resurfacing is not used. If fine rhytids are present, or if skin excess is minimal, laser resurfacing alone is performed ( Fig. 4 ). Skin excess and fine rhytids are treated with both skin pinch and laser resurfacing. This approach is also effective in patients who have very mild lid laxity because a canthoplasty can be avoided because the main supporting structures of the lid are maintained.
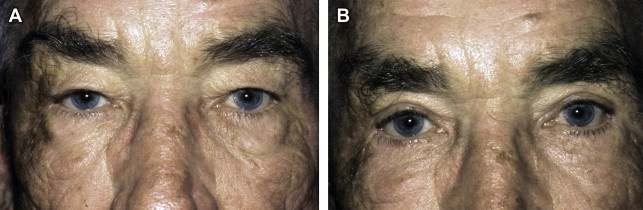
The skin/muscle external approach is used when there is extensive skin excess, festooning of the skin and orbicularis muscle, or malar bags ( Fig. 5 ). Extending the skin/muscle flap in the suborbicularis oculi fat (SOOF) layer can improve malar bags in some instances ( Fig. 6 ). Laser resurfacing can be used if fine rhytids are present.
If there is no fat pseudoherniation present and predominantly skin excess exists without malar bags, a skin-flap lower blepharoplasty is very effective in these patients. If there is any form of nicotine use, this technique is contraindicated, as is laser resurfacing at the time of surgery. This approach is by far the least frequently used approach in my practice.
Larrabee
I tailor my approach to the specific patient. The variables include a history of previous surgery; orbital anatomy, including the presence of a negative vector; skin texture and elasticity; lid tone; amount and location of pseudoherniated fat; presence of hypertrophic or lax orbicularis oculi muscle; and patient preferences. There are several techniques that may be used for lower eyelid blepharoplasty. These techniques include the skin-only approach, the skin-muscle flap, and the transconjunctival approach with or without skin excision. My most frequent approach is a transconjunctival blepharoplasty with a skin pinch. This technique allows for more controlled wound healing and, because the septum is left intact, has a lower tendency for scleral show or ectropion to develop. Fat is managed as discussed later, with either excision or transposition. Resurfacing is performed in patients who desire to address their rhytids simultaneously. Frequently, these patients are undergoing a full-face laser resurfacing in addition to the treatment of the lower lid. I currently use both active and deep fx laser resurfacing with the Coherent system. TCA (Trichoroacetic Acid) peels (35%) and full phenol peels (88%) are still useful techniques for lower lid resurfacing in my patients. I still use a skin muscle flap blepharoplasty in special situations. The major indication for this technique is hypertrophic orbicularis muscle or an extremely lax orbicularis muscle where I wish to excise redundancy and tighten the lower lid. I will also use a skin muscle flap in secondary or revision cases where a skin muscle flap was used in the primary operations. In these cases, there are sometimes scar adhesions and other problems best addressed in the same plane of dissection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





