TRAUMA AND OPTIONS FOR RECONSTRUCTION
I. GOALS
A. Form: Major component of body image
B. Function: Provides stability, organ of sensation, mobility. An intact leg without function is a hindrance to rehabilitation and recovery.
C. Vitality: Debride devitalized tissue and obtain healthy wounds
D. Amputation may result in
1. Quicker recovery course
2. Improved mobility
3. Improved wound healing
4. Improved level of activity
II. ANATOMY AND PHYSIOLOGY
A. Skeleton
1. Femur
2. Patella
3. Tibia: Bears 85% of weight, no anteromedial muscular coverage
4. Fibula: Primarily serves as anchor for muscular attachments
5. Tarsals: Calcaneus, cuboid, navicular, and cuneiforms (medial, intermediate, and lateral)
6. Metatarsals (5)
7. Phalanges (14)
B. Musculature and soft tissue
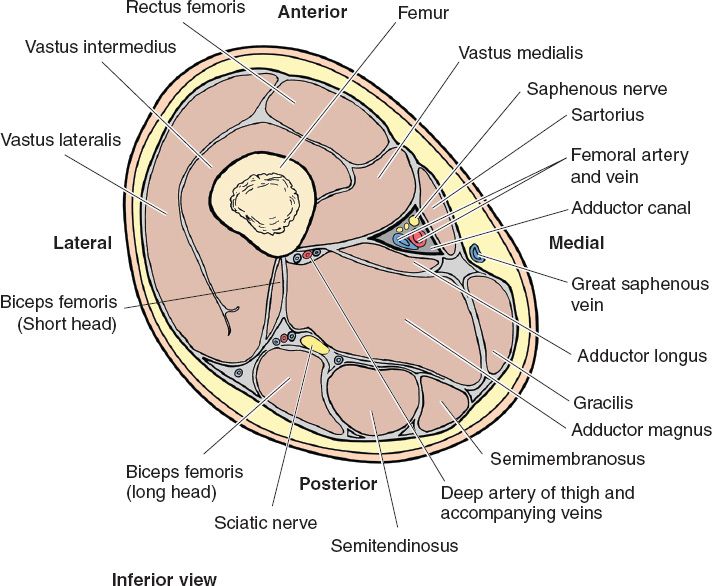
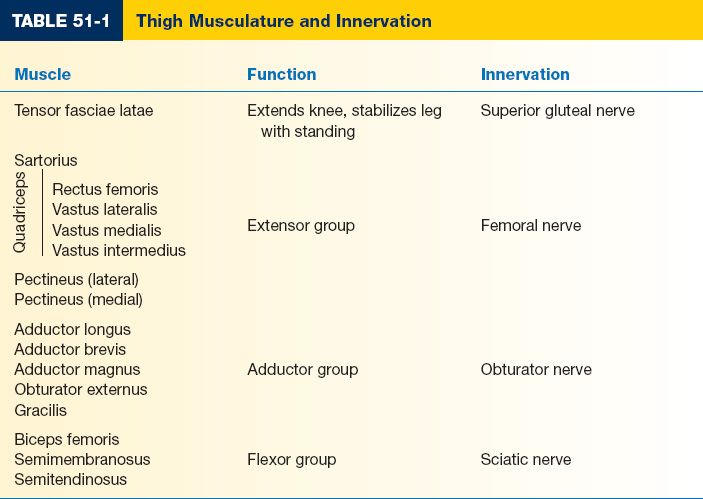
1. Thigh (Fig. 51-1 and Table 51-1)
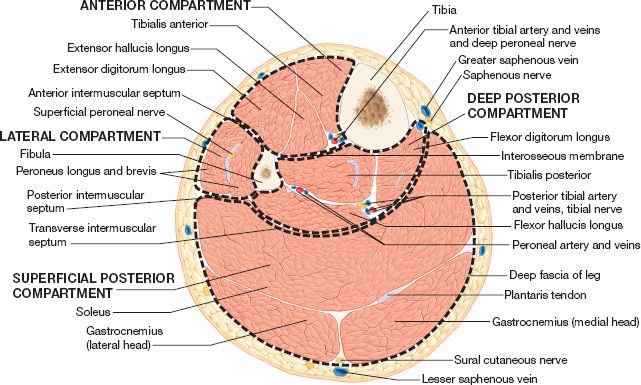
2. Lower leg (Fig. 51-2 and Table 51-2)
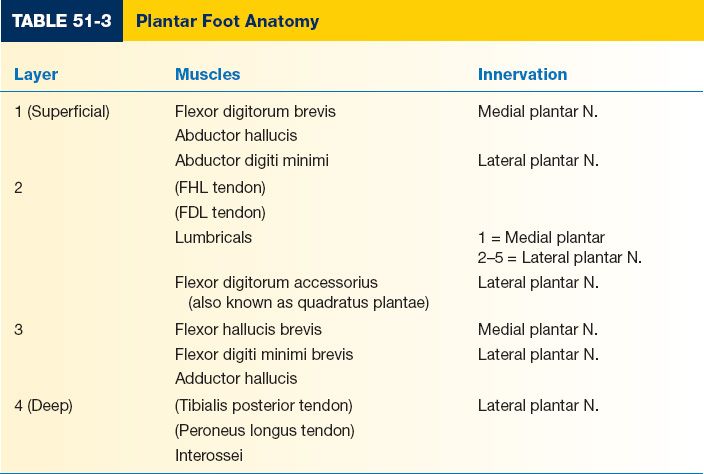
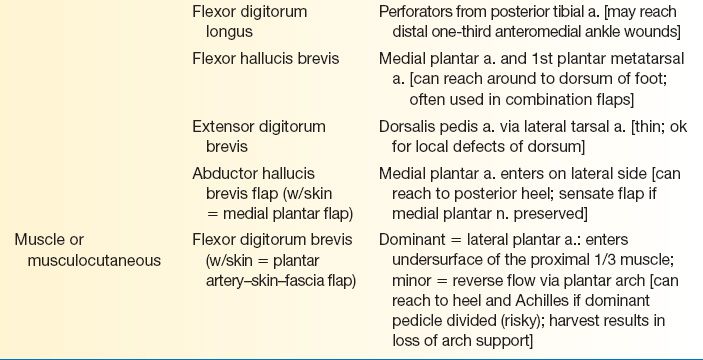
3. Plantar foot (Table 51-3)
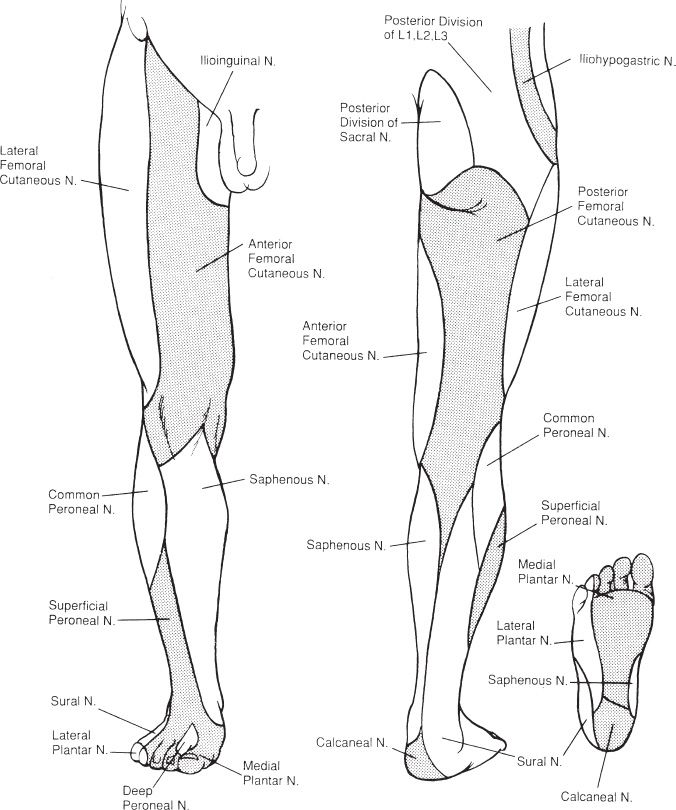
4. Sensory innervation and nerve anatomy (Fig. 51-3)
5. Muscular loss is not a contraindication to limb salvage since even a fused ankle can be ambulatory
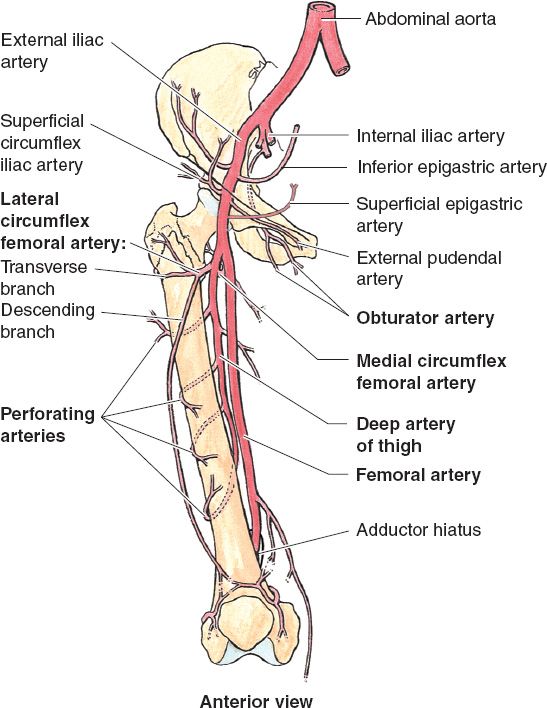
C. Vascular
1. Thigh and knee (Fig. 51-4)
a. Femoral artery
b. Deep femoral artery
c. Ascending, transverse, and descending branches of the lateral circumflex iliac artery
d. Popliteal artery
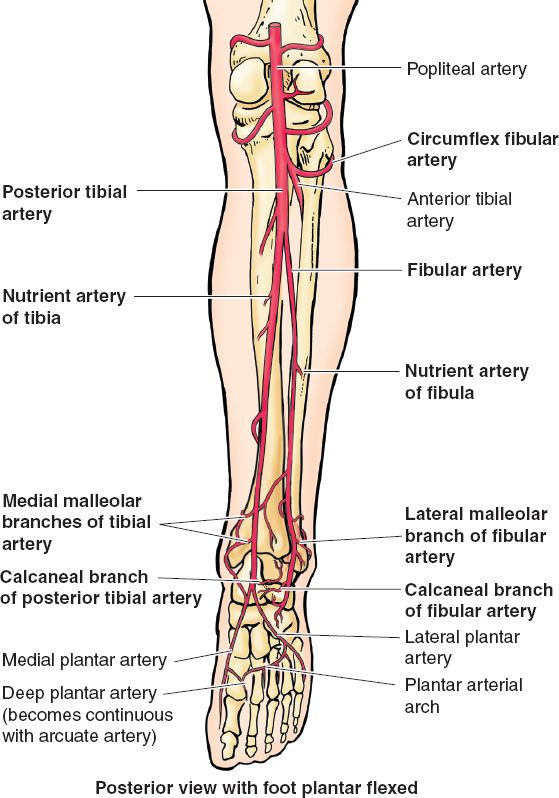
2. Leg and foot
a. Trifurcation: Anterior tibial, posterior tibial, and peroneal artery origins
b. Dorsalis pedis and posterior tibial
III. ETIOLOGY OF LOWER EXTREMITY WOUNDS AND INJURIES
A. Trauma
B. Neoplasm
C. Infection/osteomyelitis
D. Diabetic lower extremity wounds
______________
*Denotes common in-service examination topics
Figure 51-1. Anatomy of the mid thigh in cross section. (From Moore KL, Dalley AF, Agur AM, eds. Clinically Oriented Anatomy. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
Figure 51-2. Lower leg in cross section.
E. Peripheral vascular disease
F. Pressure wounds/decubitus ulcers
G. Iatrogenic/postoperative wounds
H. Irradiated tissue
I. Other
1. All of the above can be compounded on one another
2. Compartment syndrome is a risk in any lower extremity injury/reconstruction
IV. LOWER EXTREMITY RECONSTRUCTION
A. Evaluation
1. Principles of management of trauma patients: Treat the whole patient; amputation can be life-saving
2. Pertinent history
a. When/where did injury occur; potential contaminants; length of time for devascularized tissues?
b. Mechanism of injury
c. Other past medical and social history (especially smoking)
3. Physical examination
a. Neurovascular status: Pulses and sensorium
b. Skeletal and joint stability: Joint above and below injury
c. “Fracture + Laceration”: Assume open fracture until proven otherwise
4. Wound assessment
a. Extent of injury: Depth, tissues involved or devitalized
b. Exposure of vital structures: Nerve, vessels, bone, joint, and hardware
c. Contamination: Soil, chemical, marine, machinery, etc.
i. Length of time/chronicity
ii. Prior cultures (type/reliability of cultures)
iii. Prior debridements/dressings
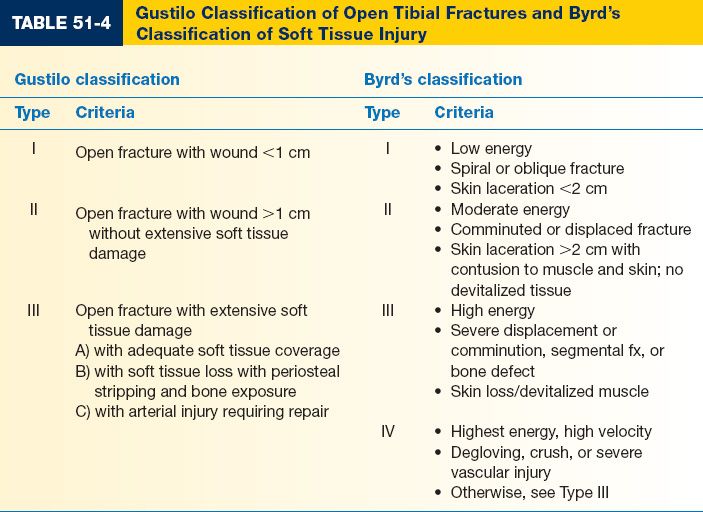
5. *Gustilo classification (Table 51-4) and Byrd’s classification: Severity of soft tissue injury predicts clinical course and healing probability
B. Acute treatment of an open fracture
1. Stabilize fracture
2. Confirm vascular adequacy: Vascular Surgery consultation early if necessary
3. If risk of compartment syndrome, four-compartment fasciotomy as necessary
4. Irrigation and debridement
5. Coverage of exposed vital structures
6. Delayed definitive closure versus serial debridements
7. Patients may benefit from early flap coverage
C. Decision point: Limb salvage versus primary amputation
1. Decisions must be made on individualized, patient-oriented basis
2. Indications for primary amputation
a. Devitalized or unsalvageable limb: Consider both short- and long-term
b. Risk to life: Intractable bleeding, overwhelming infection, etc.
Figure 51-3. Cutaneous innervation of the lower extremity.
3. Relative indications for primary amputation
a. *Tibial nerve disruption (insensate plantar foot)
b. Major soft tissue injury/fractures with significant devascularized tissue
c. Combined diaphyseal and major joint fractures
d. Open long-bone fracture with significant burns
e. Consider the patient: Elderly, obtunded and/or neurologic injury, morbid obesity, severity of fractures (not necessarily location)
4. Recent cost-utility analyses indicate that when technically possible, reconstruction is always preferable over amputation. Reconstruction results in less long-term costs and increased utility when compared to amputation.
D. Complicating factors
1. Vascular injury
a. Fracture reduction may improve spasm or compression of vessels
b. Consider temporary vascular shunts if stabilization process prolonged and limb is ischemic
c. Single vessel is usual adequate to perfuse distal lower extremity
d. If revascularization is performed, consider early fasciotomies
e. Saphenous vein is common vein graft source
2. Soft tissue avulsion
a. Injury extend often more significant than can initially be appreciated
b. Requires resection of avulsed tissue with skin harvesting for skin grafting
3. Nerve injury
a. Nerve grafting has not shown to be effective historically, better in pediatric
b. Loss of posterior tibial nerve relative contraindication to salvage
c. Sural nerve grafts
i. Minimal donor site morbidity (lateral foot numbness)
ii. Limited to use in clean and closed wounds
d. Prognosis of primary repair, if attempted, is guarded: Most patients require lifetime splinting or tendon transfers
4. Osteomyelitis
a. Diagnostic testing/studies
i. Erythrocyte sedimentation rate (ESR): High negative predictive value
ii. C-reactive protein (CRP)
Figure 51-4. Arterial anatomy of the lower extremity. (From Moore KL, Dalley AF, Agur AM, eds. Clinically Oriented Anatomy. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2010.)
iii. Bone culture and biopsy: Identification of the organism and diagnosis confirmation
iv. X-ray: Findings lag behind the progression of the disease (not accurate)
v. Tc99: False-positives if blood flow is poor
vi. Gallium—False-positives with soft tissue inflammation
vii. MRI: T1-weighted images demonstrate decreased signal in infected bone; significant interference from hardware
viii. Standards: ESR, MRI, and bone culture/biopsy
b. Treatment
i. Debridement
ii. IV antibiotics (often 6 weeks or longer)
iii. Reconstruction as needed for coverage of vitalized/healthy tissue
5. Bone gaps
a. Cancellous bone grafting
i. Needs well-vascularized bed and delayed 6 to 12 weeks from trauma
ii. >90% effective in gaps of a few centimeters
b. Ilizarov technique
i. Bone lengthening with distraction osteogenesis
ii. Best in gaps 4 to 8 cm
iii. Requires external pins, risk of pin track infections
c. Vascularized fibular grafts
i. Must preserve the proximal and distal 6 cm of donor fibula to maintain knee/ankle function; up to 25 cm theoretically harvestable
ii. 87.5% reported success rate; approximately 15 months to weight bearing with single fibula or 6 months if “twin-barreled” paired fibula
iii. Vascular supply: Peroneal artery (via nutrient artery) and periosteal
6. Compartment syndrome
a. Compartments of lower leg (Fig. 51-2)
i. Anterior
ii. Lateral
iii. Deep posterior
iv. Superficial posterior
b. Pathophysiology
i. Life- and/or limb-threatening condition
ii. Compartments function as closed containers—pressure can build without adequate release
iii. Syndrome results when compartment pressures exceed perfusion pressures (approximately 30 mm Hg), leading to myoneural necrosis
iv. Can cascade: Hematoma increases pressure, causes inflammation increasing pressure, etc.
v. Do not be fooled: An open fracture does not protect against compartment syndrome, patient still requires full fasciotomies
vi. Systemic damage from necrotic debris, rhabdomyolysis, or even reperfusion injury following correction. Consider alkalizing urine (HCO3 in IV fluids) goal urine pH > 8
c. Signs and symptoms (“cardinal signs”)
i. Pain out of proportion
ii. Pain on passive movement (flexion or extension)
iii. Swollen/tense compartments
iv. Loss of pulses (LATE) and anesthesia (LATE)
v. Clinical diagnosis
vi. Pressure needles (Stryker): If convenient, gold standard for testing
vii. Can use standard needle or even arterial line kit to measure pressures
viii. Threshold pressures for diagnosis is controversial
a) Some consider >30 mm Hg an indication for fasciotomy
b) > 40 mm Hg for >6 hours OR >50 mmHg for any length of time
d. Treatment: Four-compartment fasciotomy
V. TECHNICAL ASPECTS OF RECONSTRUCTION AND MATERIALS
A. Amputation: Core concepts
1. Preserve length
a. Practice limb salvage through amputation
b. Ideal below-knee amputation (BKA) length is 10 cm below the tibial tuberosity
i. The transverse incision is made 10 cm distal to the tibial tuberosity
ii. Its length is equal to two-thirds of the circumference of the leg at that level
iii. The posterior incision is made parallel with the gastrocnemius/soleus muscle complex
iv. The length of the posterior flap is equal to 2 times the distance from mid-tibia to lateral extent of incision (gastrocnemius/soleus complex)
v. The tibia is scored circumferentially, and a periosteal elevator is used to dissect the soft tissues away from the tibia for a distance of approximately 3 to 4 cm
vi. The tibia is then transected just proximal to the transverse skin incision angled distally so anterior part of tibia does not bear excess weight
vii. Use rasp or reciprocating saw to smooth out bone
viii. The fibula is then transected with a bone cutter at least 1 cm cephalad to the tibial transection level
ix. The corners of the incisions are curved to avoid dog-ears
x. Close over drain
c. Person with a BKA has an increased energy demand
d. Benefits of BKA versus above-knee amputation (AKA)
i. BKAs requires less work for ambulation than AKAs
a) 25% vs. 65% increase in energy expenditure than with no amputation
b) 45% increase in energy expenditure for patients with bilateral BKA
ii. BKAs report better quality of life than AKAs
iii. Midfoot amputations show no added benefit over BKAs
2. Keep “spare” parts
a. Fillet flaps (commonly fasciocutaneous flaps) may be used in tissue transfer
b. Skin grafts (full- or split-thickness) can be obtained from the amputated part
3. Contaminated wounds: Delayed closure/reconstruction; guillotine amputation
B. Primary reconstruction
1. Timing
a. Immediate coverage indicated for clean wounds with exposed vital structures
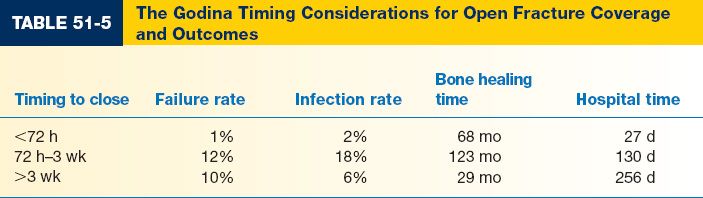
b. Early coverage has been advocated to limit complications (Table 51-5)
c. Goal: Clean, viable, vascularized wound bed with no exposed vital structures
d. Note: Platelets increase fourfold as acute phase reactant and may contribute to subsequent complications
2. Skeletal stabilization
a. First goal of operative management to provide stable fixation
b. Skeletal blood supply
i. Periosteal and nutrient arteries
ii. Periosteal stripping should be minimized
c. Techniques
i. Traction: If patient unstable, temporary measure
ii. Cast immobilization: Adequate for closed fractures or open fractures with a stable/clean wound
iii. Intramedullary nailing
a) Useful with minimal comminution and no significant bone loss
b) Reamed nails: Early mobility, but tight fixation results in endosteal vascular obliteration
c) Nonreamed nails: Risk in Gustilo grade IIIB/C for intramedullary infection; can be very effective
d) Early, stable coverage necessary
iv. Plate/screw fixation
a) May require significant soft tissue and periosteal stripping
b) Early, stable coverage necessary
v. External fixation
a) Gold standard with significant trauma to soft tissue
b) Minimizes additional soft tissue/vascular trauma
c) May obstruct subsequent reconstruction efforts
d) Pin tract infection risk
e) May be combined with procedures for bone gaps
3. Debridement
4. Soft tissue reconstructive ladder versus elevator
a. Observation/dressing changes
i. Unavailable if exposed vital structures
ii. Must keep tendon moist to avoid desiccation
iii. Vacuum-assisted closure (VAC) devices shown to be useful
a) Decrease bacterial counts
b) Increase cell division
c) Reduce edema/fluid collection
d) *Reduces wound metalloproteinases
e) Often temporizing for final reconstruction
f) Less effective if devitalized tissue still present or if exposed bone without periosteum
b. Primary closure: Requires low tension; healthy, clean wounds
c. Skin grafting
i. Poor coverage on weight-bearing areas (i.e., heel and plantar midfoot)
ii. Inappropriate over hardware, bone, vital structures, or bare tendon
d. Tissue expansion: Poor results, high complication rates (>75%)
e. Local flaps (see below)
f. Regional flaps
i. Cross-leg flaps are of historic significance only
ii. Propeller-type flaps based on perforators from the peroneal artery can be an alternative to free tissue transfer
i. Valuable in complicated wounds or wound with significant local soft tissue injury
ii. Contouring of muscle flaps improves over time (secondary to atrophy from denervation and disuse)
iii. *Anastamosis should be outside zone of injury (vein grafting as needed)
iv. End-to-side anastomosis beneficial: Does not sacrifice distal circulation
v. Preoperative imaging (CTA, ultrasound, or angiography) allows for improved preoperative planning
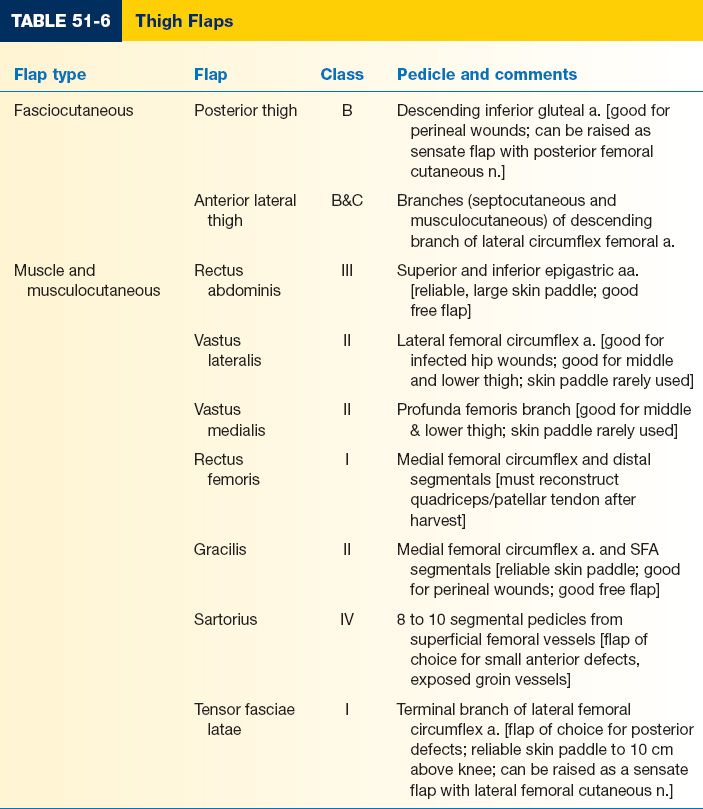
5. Thigh reconstruction (Table 51-6)
a. Ample muscle/soft tissue surrounding femur is an advantage
b. Rarely requires distal free flap reconstruction
6. Knee reconstruction
a. Skin graft satisfactory if joint capsule intact (may be unstable or result in limiting joint contracture)
b. Gastrocnemius muscle flap (medial or lateral head)
i. Medial head provides wider arc of rotation (4 cm more), broader belly
ii. Lateral gastrocnemius requires identification of common peroneal nerve to avoid injury
iii. Dominant vasculature: Medial and lateral sural arteries off the popliteal, respectively
iv. Muscle fascia can be scored to provide additional coverage area
c. Alternatives
i. Distally based gracilis, sartorius, vastus lateralis muscle flaps
ii. Random flaps can be designed off anastomosis of superior geniculate vessels and the descending branches of the lateral circumflex femorals
iii. Consider distally based anterior lateral thigh (ALT) fasciocutaneous flap
d. Note: May require patellar tendon reconstruction—consider tensor fascia lata (TFL) flap
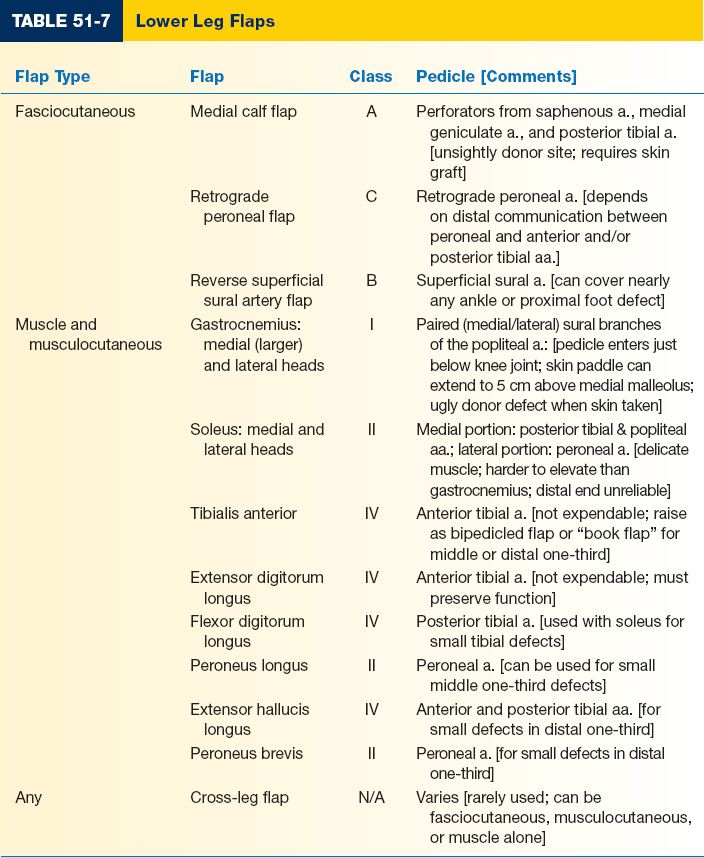
7. Lower leg reconstruction—“Rule of Thirds” (Table 51-7)
a. Proximal third
i. First choice: Gastrocnemius muscle flap with skin grafting
ii. Alternatives: Soleus, tibialis anterior
iii. Bipedicled tibialis anterior muscle flap
a) Preserves dorsiflexion
b) Useful for proximal and middle third of lower leg
iv. Free tissue transfer is typically preferable in this location than cross-leg
b. Middle third
i. First choice: Soleus muscle flap (proximally based) with skin graft
ii. Alternatives: Gastrocnemius, tibialis anterior, and flexor digitorum longus
iii. Again, consider free flap
c. Distal third
i. First choice with large soft tissue defects: Free flap
ii. If free flap is contraindicated, consider alternative regional flaps
a) Soleus, peroneus brevis, extensor digitorum longus, extensor hallucis longus, tibialis anterior, lateral supramalleolar flaps
b) Random, multiply delayed flaps
c) Dorsalis pedis flap
iii. Reverse superficial sural artery flap
a) Pedicle is distal peroneal artery perforators located 4 to 7 cm proximal to malleolus
b) Also uses vascular plexus of sural nerve and lesser saphenous vein
c) Increased complications with (1) age >40 years, (2) comorbidity (peripheral vascular disease, venous insufficiency, and diabetes)
d) 21% reported local flap necrosis
e) Can delay at time of initial wound debridement
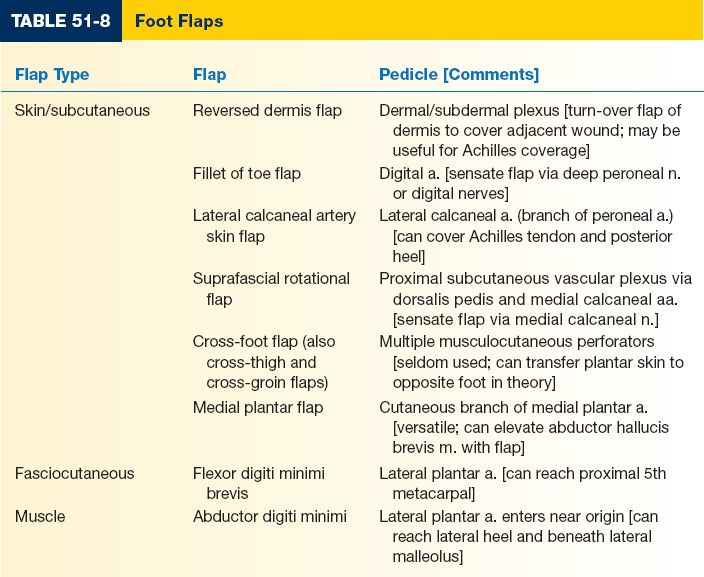
8. Foot reconstruction (Table 51-8)
a. Dorsum of the foot: Think thin flap with high surface area (i.e., fasciocutaneous flaps are excellent options)
b. Plantar foot
i. Thickest skin on the body (up to 3.5-mm-thick)
ii. First choice: Instep flap versus fasciocutaneous flap
iii. Alternatives: Skin graft (unstable)
iv. Attempts should be made to preserve sensation
CHRONIC ULCERS AND THE DIABETIC FOOT
I. GENERAL CONSIDERATIONS
A. Why does an acute wound become chronic? (See Chapter 1)
B. Useful labs and studies
1. Hemoglobin A1C
2. Osteomyelitis workup (see above)
3. Cultures and biopsies (do not forget possibility of malignancy—Marjolin’s ulcer, etc.)
4. Ankle-brachial index (ABI) testing
a. Involve vascular surgery if abnormalities exist
b. History of claudication and/or rest pain
c. Physical examination: Cool extremity with dry, shiny, and hairless skin
d. Other studies per vascular consult: Arteriogram, CTA, MRA, etc.
e. ABI less than 0.4 indicates major inflow disease and necessitates vascular surgery consultation
5. *Quantitative cultures: Generally 1 × 105 of most species will impair wound healing and prevent skin grafts from taking. This may be lower for Streptococcus pyogenes species (1 × 103 may impair healing).
6. Venous stasis ulcers and lymphedema (See Chapter 13): Mainstay is compression
7. Consider labs for rheumatologic/vasculitic disease if appropriate
C. Debridement of devitalized tissue, obtaining and clean wound, and offloading facilitate healing in most ulcers
II. ETIOLOGY
A. Neuropathy
1. Pathophysiology
a. Alerted neuronal metabolism due to prolonged hyperglycemia
b. Buildup of sorbitol in perifascicular connective tissue leading to intraneural compression
c. Decreased rate of anterograde axoplasmic flow (decreased nerve healing)
d. Compounded by “double crush phenomenon”: Additional sources of compression (i.e., cubital or carpal tunnel syndromes) compound the problem
2. Sensory neuropathy: Leads to inability to detect, sense, or protect injuries/wounds
3. Diagnosis: 10 g of pressure using a 5.07 Semmes–Weinstein filament
4. Autonomic neuropathy: Anhydrosis and arteriovenous shunting lead to dry and cracked skin
5. Motor neuropathy: Alerted mechanics and function, leading to joint/toe deformity
B. Ischemia
1. Secondary to micro- and macrovascular disease
2. “Trashed trifurcation” disease: Destruction and arteriosclerosis of the infrapopliteal branches; foot branches may be spared
3. ABI’s: Falsely elevated due to calcification (incompressible vessels). TBI’s may be a better indicator of blood supply.
C. Immune dysfunction and immunosuppression
1. Involves both cellular and humeral immune systems
2. Superficial infections usually gram-positive cocci
3. Deep infections usually polymicrobial, including anaerobes
D. Mechanical/traumatic
1. Charcot Foot: Collapse of midfoot bones (rate: 1 in 800 diabetics)
2. Shortening of the Achilles tendon: Due to loss of collagen elasticity
III. TREATMENT AND RECONSTRUCTION
A. Superficial injury (with or without infection): Pressure relief and topical antibiotics as necessary
B. Cellulitis
1. Antibiotics: Consider coverage for β-hemolytic streptococcus and methicillin-resistant Staphylococcus aureus (MRSA)
2. Gold Standard: Trust only tissue cultures (swabs are notoriously misleading)
3. Consider fungal infections, for example, Tinia pedis, in persistent cellulitic infections
C. Deep ulcers
1. Assessment
a. Exposed bone: Obtain bone biopsy, begin osteomyelitis workup
b. Sequestrum: Devitalized and infected bone and soft tissue that must be debrided thoroughly
c. Consider infectious disease involvement, will likely need 6 weeks IV antibiotics if osteomyelitis is considered
d. Severe osteomyelitis generally necessitates some level of amputation, especially in patients who are poor candidates for subsequent reconstruction
e. Depending on clinical scenario, toe amputation, ray amputation, midfoot amputation, or BKA may be appropriate
2. Postoperative care includes pressure offloading, optimization of nutrition, diabetic or wedge shoes in ambulatory patients, and regular foot examinations
PEARLS
1. Debridement of all devitalized tissue is key to successful staged reconstruction
2. Understand different options for soft tissue coverage of the lower leg including the following workhorse flaps: gastrocnemius for upper third, soleus for middle third, and free tissue transfer for the distal third
3. Limb salvage should be the default operation, but understand the relative indications for amputation
4. Understand the concept of perforator flaps and the vascular anatomy of the lower extremity
5. Chronic wounds can be properly managed with offloading, nutrition, edema control, and bacterial management
QUESTIONS YOU WILL BE ASKED
1. Mathes–Nahai flap classification of flap types (know dominant and minor vessels)
See Tables 51-6 and 51-7.
2. A patient undergoes open reduction and internal fixation of an open tibial fracture and develops purulent drainage. An extensive debridement is performed with subsequent flap coverage. IV antibiotics are continued for 8 weeks. The patient does well initially, but at a post-op appointment 3 months later, a recurrence of the infection is present. Why?
If hardware is left in place, bacteria may survive on a biofilm. If hardware was removed, inadequate bone debridement with retained sequestrum is likely the cause.
3. What is the most appropriate reconstruction for an open distal third tibia fracture?
The classic answer is that free flap reconstruction is necessary for these types of injury. However, recent literature has shown that peroneal or posterior tibial-artery-based propeller flaps can be useful as well.
4. What nerve is most at risk in dissection of lateral gastrocnemius flap?
Common peroneal.
THINGS TO DRAW
1. Draw the lower extremity vascular anatomy in detail, including thigh, knee, lower leg, and foot (Fig. 51-4).
2. Draw the lower extremity dermatomes (Fig. 51-3).
3. Draw a cross-section of the leg at different levels within the thigh and lower leg (Figs. 51-1 and 51-2).
Recommended Readings
Allen MJ, Stirling AJ, Crawshaw CV, Barnes MR. Intracompartmental pressure monitoring of leg injuries. An aid to management. J Bone Joint Surg Br. 1985;67(1):53–57. PMID: 3968144.
Byrd HS, Spicer TE, Cierney G 3rd. Management of open tibial fractures. Plast Reconstr Surg. 1985;76(5):719–730. PMID: 3903801.
Chung KC, Saddawi-Konefka D, Haase SC, Kaul G. A cost-utility analysis of amputation versus salvage for Gustilo type IIIB and IIIC open tibial fractures. Plast Reconstr Surg. 2009;124(6):1965–1973. PMID: 19952652.
Godina M. Early microsurgical reconstruction of complex trauma of the extremities. Plast Reconstr Surg. 1986;78(3):285–292. PMID: 3737751.
Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58(4):453–458. PMID: 773941.
< div class='tao-gold-member'>