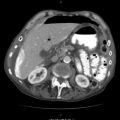
Fig. 41.1
Chest wall defect 5–10 cm in diameter with open pneumothorax, comminuted rib fractures, intercostal muscle tearing, and underlying pulmonary injury
After airway management, examine the edges of the chest wall defect for significant bleeding. Many experienced first responders are capable of clamping an arterial or venous bleeder in the chest wall, assuming they have an appropriately sized clamp. It does not make sense to embark on a significant transport to a higher level of care while an easily accessible vessel continues to hemorrhage. The chest wall contains numerous named arteries and veins, e.g., the intercostal arteries and veins as well as the muscular branches of the subclavian and axillary vessels, any of which can exsanguinate the patient. Any continuous bleeding during transport can lead to a coagulopathy that will be difficult to reverse even once the patient arrives at a hospital. Only the most obvious sites of hemorrhage should be clamped and not more than 3 min should be spent under austere conditions. First responders would not be expected, however, to try to clamp a pulmonary laceration within the thorax or attempt to control a source of mediastinal hemorrhage. In the case of severe pulmonary or mediastinal bleeding, however, following airway control, the hemithorax should be tightly packed with gauze in the hope of at least slowing the hemorrhage.
You should cover the defect itself with a sterile or clean dressing, e.g., a dry gauze, petrolatum gauze or plastic wrap, and secure on three sides only so that the accumulating pleural air, e.g., from a pulmonary or tracheobronchial laceration, can escape from the pleural space. This measure will prevent the development of a tension pneumothorax and will also prevent further contamination of the wound from the outside.
Because these patients have a high risk of deterioration and will likely require immediate surgery, transport to a designated trauma center should not be further delayed. During transport, a hypotensive strategy of resuscitation should be employed to minimize blood loss, dilutional coagulopathy, and pulmonary edema.
41.2 Emergency Department Management
For a patient with a larger and more destructive chest wall injury, the emergency department (ED) should be bypassed for direct transport to the operating room (OR). If an OR is not ready, ED management should be limited to life-saving procedures that cannot wait until an OR is available. For example, you can address exsanguinating hemorrhage from the edges of the defect, within the pulmonary parenchyma or in the mediastinum. Hilar clamping and the pulmonary hilar twist are effective means of temporarily controlling pulmonary hemorrhage. Time spent in the ED can also be used to obtain a blood specimen for type and cross, to ensure adequate venous access, to obtain a chest radiograph, and to begin blood product transfusion.
If the chest wall defect is smaller and hemorrhage is controlled, you can start a search for associated injuries in the ED prior to operative repair. In cases where the chest wall defect resulted from an explosion or a severe blunt mechanism, extrathoracic injuries may take precedence in the treatment plan. Head, neck, and torso CT scans may be indicated.
41.3 Operative Management
You can safely and effectively manage the smaller defect of 5–10 cm in diameter (Fig. 41.1) with minimal contamination of dirt and debris in one to three serial operations: Administer to the patient prophylactic intravenous antibiotic coverage for gram-positive organisms. The first operation consists of wound cleansing and debridement of devascularized skin, subcutaneous fat, muscle, and bone. If the defect involves only the intercostal muscle between two ribs and wound contamination is nil or very minimal, debride the defect and close it in a single operation. The intercostal muscle defect is closed by approximating the two ribs together with absorbable suture, taking care not to entrap the intercostal nerve. The best way to approximate the ribs without nerve entrapment is to drill four holes in each rib and cerclage the two ribs together with figure-of-eight ties. Then close the skin over a bulb suction drain.
If the defect involves comminuted rib fractures, tissue loss, and contamination, then at least two operations are necessary. Excise the portions of the rib that are partially devoid of muscular attachments because the devascularized bone will not survive and will later become a nidus for osteomyelitis. If contamination is nil or minimal, a biologic tissue patch derived from the human or porcine dermis can be sutured circumferentially to the defect in the first operation (Fig. 41.2). Such tissue patches provide protection to the underlying lung, effectively bridge the defect with a firm yet flexible platform, and are less prone to infection than a nonbiologic prostheses. If along one of the edges of the defect, a rib fracture or even a comminuted rib fracture with a small tissue gap is present, affix an absorbable, polylactide fracture repair plate to the rib to provide a stronger edge to which to anchor the patch (Fig. 41.2 inset).
Fig. 41.2
A biologic tissue patch derived from human or porcine dermis is sutured circumferentially to the defect. If a comminuted rib fracture is present, an absorbable plate is affixed to the rib to provide a stronger edge to which to anchor the patch (inset). Partially devascularized bone should be excised
Place an anterior 32 or 36 French chest tube, either straight or right-angled, to underwater seal/wall suction to drain air and fluid that will accumulate. Dress the wound with a vacuum suction dressing over the biologic patch (Fig. 41.3) for at least 2 and as long as 3 days. The patient can be extubated postoperatively depending on the extent of the pulmonary injury and any associated injuries. The vacuum dressing can be expected to provide an adequate degree of chest wall stability for this smaller-sized defect.