PHARMACOLOGY OF LOCAL ANESTHETICS
I. CHEMISTRY
A. Local anesthetic (LA) molecules consist of three components, each of which contributes distinct properties to the molecule:
1. Aromatic ring: Determines lipid solubility and hence potency.
2. Amine end: exists in either a tertiary form (lipid soluble) or a positively charged quaternary form (water-soluble) depending on pH and determines the time of onset.
3. Intermediate ester/amide: determines pattern of biotransformation, allergic potential, and stability in solution.
II. MECHANISM OF ACTION
A. LAs reversibly block neural conduction in peripheral nerves by halting the propagation of action potentials.
1. *LAs prevent depolarization. Anesthetic molecules reversibly bind to Na+ channels and inhibit Na+ influx, thus preventing the depolarization threshold from being reached.
2. LAs have no effect on the resting or threshold potential, although the refractory period and repolarization may be prolonged.
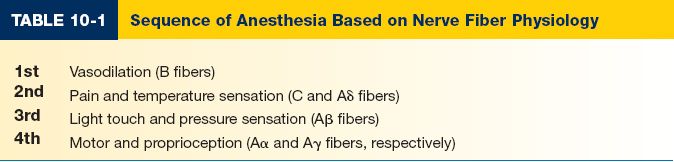
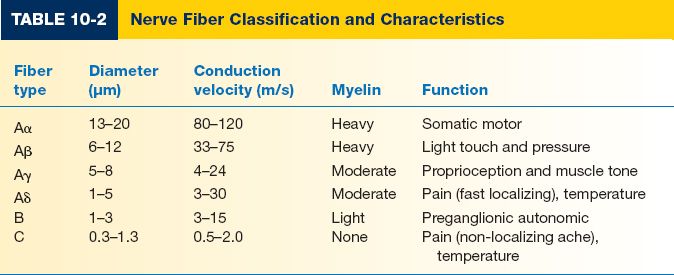
3. Sequence of anesthesia relates to nerve fiber biology (Tables 10-1 and 10-2):
a. Small diameter fibers more sensitive to LAs than larger diameter fibers. The distance of impulse propagation in small fibers is shorter.
b. Myelinated fibers are more sensitive than unmyelinated fibers. Myelinated nerves need only to be block at several nodes of Ranvier to inhibit impulse propagation, thus requiring smaller concentrations of anesthetic.
c. Nerves with higher firing frequency are more sensitive.
d. The affinity of LAs for Na+ channels depends on the state of the channel: Open state > inactivated state > resting state.
e. Pain fibers have a higher firing rate and relatively longer action potential than motor fibers and are thus more sensitive.
III. PHARMOKINETICS
A. Time of onset
1. The pKa of LAs determines the rate of onset
a. The pKa is the pH at which a solution of LA is in equilibrium, with half in the neutral base (salt) and half in the ionized state (cation).
b. A decrease in pH shifts equilibrium toward the ionized form.
c. *The lower the pKa (closer to pH 7.4), the higher the concentration of nonionized LA at a given pH, and therefore, the faster the onset.
d. Only the nonionized form crosses the plasma membrane.
e. After crossing the cell membrane, the LA is exposed to a more acidic intra-cellular environment and is converted to its ionized state. The ionized molecule then binds to the sodium channel and blocks conduction.
f. *The addition of sodium bicarbonate will raise the pH of the solution and thus speed the onset of action.
______________
*Denotes common in-service examination topics
2. Infected and inflamed tissues have a low pH, which decreases the concentration of nonionized LA and reduces the effect.
B. *Potency of an LA is determined by its lipid solubility
1. The aromatic ring determines the degree of lipid solubility.
2. As the lipid solubility increases, the ability of the LA to penetrate the plasma membrane increases.
C. Duration of action
1. LAs vary in their tendency to bind plasma proteins
a. When in circulation, LAs bind to α-1-acid glycoprotein.
b. LAs with higher affinity for protein binding remain bound to nerve membranes longer, increasing their duration of action.
c. Binding to plasma proteins decreases the concentration of free drug in circulation, reducing the potential for toxicity.
d. As pH decreases, the affinity for plasma proteins is decreased. Thus, in conditions of acidosis or decreased serum protein, there is a greater potential for toxicity.
2. Intrinsic vasodilatory effect reduces the duration of anesthesia
a. All LAs cause vasodilation, except cocaine, which causes vasoconstriction.
b. Vasodilation enhances removal of LA, thus shortening the duration.
c. *Epinephrine counters the vasodilatory effects of LAs and prolongs their duration of action
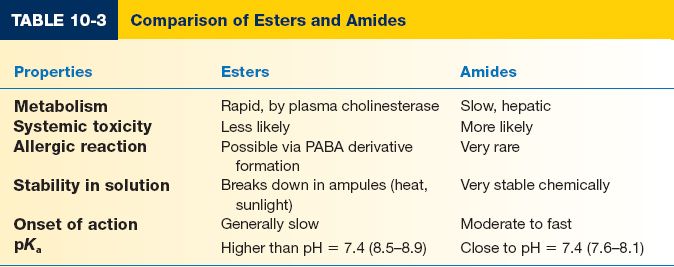
IV. CLASSES OF LOCAL ANESTHETICS (TABLES 10-3 AND 10-4)
A. Amino-esters
1. *Metabolized by circulating pseudocholinesterase, which causes shorter half-lives, except cocaine, which is metabolized by the liver.
2. *Potential for allergic reaction. Breakdown product created by the action of serum pseudocholinesterases on the amino ester includes para-aminobenzoic acid (PABA), which is very antigenic.
a. Majority of reactions are instead caused by anxiety, vasovagal responses, or accidental intravascular injection.
b. Less than 1% of reactions are true allergies.
3. Examples
a. *Cocaine: Vasoconstrictor; topical use only; useful intranasally for concurrent anesthesia and hemostasis.
b. Chloroprocaine: Rapidly metabolized; favored by obstetricians due to low fetal exposure.
c. Procaine (Novocaine): Rapid onset and short duration; not effective topically
d. Tetracaine (Pontocaine): Effective topically
B. Amino-amides
*Note: Amide LAs contain an “i” before the “-aine” in their names.
1. Metabolized in the liver. Half-lives are thus longer (2 to 3 hours).
2. True allergy is very rare.
a. Methylparaben is an antibacterial preservative sometimes used in LA cartridges that is metabolized to PABA.
b. There is no cross-reactivity between the amide and ester agents.
c. No longer contraindicated in patients with a family history of malignant hyperthermia.
3. Examples
a. Lidocaine (Xylocaine): Rapid onset; moderate duration; highly stable; non-irritating
b. Mepivacaine: Longer duration and more rapid onset than lidocaine.
c. Bupivacaine (Marcaine, Sensorcaine): Slow onset, long duration; high potency and toxicity; mixed with lidocaine for rapid onset and long duration block. Preferentially blocks sensory versus motor fibers.
d. Ropivacaine (Naropin): Similar to bupivacaine, but less potent and less cardiotoxic.
e. Etidocaine (Duranest): Used for regional blocks; preference for motor over sensory fibers.
f. Prilocaine (Citanest): 40% less toxic acutely but its metabolite, o-toluidine, can cause methemoglobinemia
V. VASOCONSTRICTORS
A. Combined with LAs to provide local hemostasis and prolong anesthesia by delaying absorption. In doing so, they decrease the potential for systemic toxicity and increase the safety margin.
B. Epinephrine is the most commonly used vasoconstrictor
C. Disadvantages with the use of epinephrine include the potential for tissue ischemia, tachycardia, hypertension, and arrhythmias
D. Contraindications
1. Small volumes of LA with dilute epinephrine concentrations (≤1:200,000) may be safe for digital blocks. However, use is contraindicated when digital perfusion is already compromised (e.g., diabetes, vascular disease, Raynaud’s disease, trauma, infection).
2. Do not use on any skin flap with limited perfusion (e.g., delayed flaps).
3. Do not use in the penis.
4. Use caution when giving larger doses in patients with known cardiac disease, hypertension, diabetes, and thyrotoxicosis and in patients taking β-blockers and/or monoamine oxidase inhibitor (MAO) inhibitors, as concomitant use has the potential to cause a hypertensive crisis.
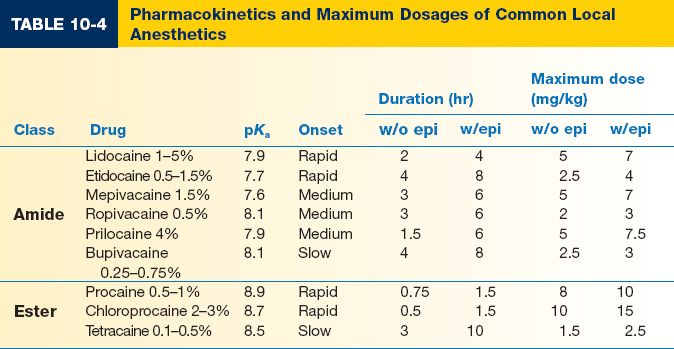
VI. DOSING AND CALCULATIONS (TABLE 10-4)
A. Epinephrine dosing
1. Expressed as a ratio of grams of solute in milliliters of solvent (e.g., a 1:100,000 concentration = 1 g epinephrine in 100,000 mL solution)
2. Typical epinephrine concentrations in anesthetic solutions = 1:400,000 (2.5 μg/mL), 1:200,000 (5 μg/mL), 1:100,000 (10 μg/mL), and 1:50,000 (20 μg/mL)
3. Plain epinephrine comes in either 1:1,000 (1 mg/mL) or 1:10,000 (0.1 mg/mL) concentration vials.
4. To prepare a 1:200,000 LA solution from plain epinephrine, 1:1,000 epinephrine must be diluted 200 times (a 1:10,000 solution must be diluted 20 times).
a. Example: Add 0.1 mL of 1:1,000 epinephrine to 20 mL of LA solution
b. Example: Add 2.5 mL of 1:10,000 epinephrine to 50 mL of LA solution
B. LA dosing
1. LAs come in various concentrations, for example:
a. Lidocaine: 1% (10 mg/mL), 2% (20 mg/mL), and 0.5% (5 mg/mL)
b. Bupivacaine: 0.5% (5 mg/mL) and 0.25% (2.5 mg/mL)
2. Maximum safety dose is increased by epinephrine.
3. Higher blood concentrations are associated with large volumes of dilute LA when compared to the same dose in a smaller volume.
4. Mixing LAs
a. Mixtures of lidocaine and bupivacaine are commonly given to provide rapid, long-lasting effect.
b. The toxicity of a mixture of LAs does not exceed that of its individual components.
c. Allows smaller volumes of individual LAs to be used.
5. *Maximum volume allowed × patient weight (kg) × [LA]1 × maximum safety dose
a. Example: 2% lidocaine with epinephrine in a 80-kg man
i. 80 kg × 1 mL/20 mg × 7 mg/kg = 28 mL
b. Example: 0.5% bupivacaine with epinephrine in a 70-kg woman
i. 70 kg × 1 mL/5 mg × 3 mg/kg = 42 mL
VII. ADVERSE REACTIONS AND MANAGEMENT
A. Central nervous system (CNS) toxicity
1. Initial excitatory symptoms reflect escalating drug concentrations in CNS.
2. Increasing concentration begins to block inhibitory pathways in the amygdala, resulting in unopposed excitatory neuron function. Symptoms: Muscular twitching, visual disturbance, tinnitus, light-headedness, tongue and lip numbness, anxiety, feelings of impending doom, disorientation, shivering, and tremors
3. Increasing concentrations cause depression of medullary centers. Symptoms: Respiratory failure, hypotension, bradycardia, arrhythmias, grand mal seizures, and coma.
B. Cardiovascular toxicity
1. The cardiovascular system is more resistant to the effects of LAs than the CNS.
2. LAs decrease myocardial excitation, the force of contraction, and the conduction rate.
3. Peripheral vasculature resistance is decreased secondary to arteriolar dilation.
4. Symptoms
a. Hypotension
b. Bradycardia
c. Arrhythmias
d. Ventricular fibrillation
e. Cardiovascular collapse
5. Cocaine differs from other LAs in that it blocks the reuptake of norepinephrine, resulting in vasoconstriction, hypertension, and cardiac arrhythmias.
6. Bupivacaine and etidocaine have the greatest cardiac toxicity and can cause profound cardiovascular depression after accidental intravascular injection.
a. Ropivacaine is similar to bupivacaine in onset and duration, but has a better safety profile in terms of cardiovascular toxicity
C. Neuromuscular toxicity
1. LAs depress calcium activity, leading to decreased muscle excitability and contractility.
2. Reversible myotonic effects with direct injection into muscles.
D. Methemoglobinemia
1. Can be caused by prilocaine’s metabolite, o-toluidine
2. Manifests as shortness of breath, cyanosis, mental status changes, headache, fatigue, dizziness, and loss of consciousness.
3. Arterial blood with elevated methemoglobin levels has a characteristic chocolate-brown color.
E. Allergic reaction
1. Most common adverse reaction
2. Often confused with patient anxiety, vasovagal responses, or accidental intravascular injection.
3. Signs and symptoms: Localized erythema, rash, pruritus, urticaria, edema, bronchospasm, and hypotension
F. Special considerations
1. Potential for toxicity is increased when amide anesthetics are used in patients with poor hepatic function or blood flow (e.g., congestive heart failure, cirrhosis, hypothermia, general anesthetics, β-blockers).
2. Epinephrine can have deleterious effects in patients with cardiac disease, hypertension, and thyrotoxicosis and in patients taking β-blockers and/or MAO inhibitors.
3. The toxicity of ester anesthetics is increased in patients with pseudocholinesterase deficiency.
1. CNS toxicity
a. Stop injection
b. Ensure airway patency
c. Administer supplemental O2
d. Ensure adequate ventilation (hyperventilation may help by increasing the pH in the presence of metabolic acidosis and hence decrease toxicity).
e. Confirm or establish IV access
f. Seizure control: Administer diazepam 0.1 mg/kg IV, thiopental 2 mg/kg IV, propofol 1 mg/kg IV, or succinylcholine 0.1 to 0.2 mg/kg IVP followed by intubation.
g. Assess cardiovascular status throughout.
2. Cardiovascular collapse
a. IV fluids for hypotension
b. Atropine for bradycardia
c. Manage arrhythmias according to ACLS protocols, except that additional lidocaine should not be administered.
d. Alert the nearest facility having cardiopulmonary bypass capabilities.
e. Consider treatment with lipid emulsion.
i. Bolus 1.5 mL/kg intravenously over 1 minute
ii. Continuous infusion 0.25 mL/kg/min
3. Methemoglobinemia
a. Administer 100% supplemental oxygen
b. Methylene blue 1% solution 1 to 2 mg/kg IV, administered slowly over 5 minutes.
4. Treat epinephrine-induced digital ischemia with phentolamine
5. Allergic reactions
a. Mild reactions
i. Treat with Benadryl 25 to 50 mg IV/PO in adults, 1 mg/kg IV/PO for pediatrics
b. Anaphylaxis
i. Airway management, IV fluids, supplemental oxygen
ii. Treat with 0.3 mL of epinephrine SC (1:1,000)
iii. Corticosteroids (125 mg methylprednisolone IVP or 60 mg prednisone PO)
NERVE BLOCKS
I. TEN WAYS TO DECREASE PAIN ASSOCIATED WITH INJECTION
A. Reassurance and distraction
1. Explanation, encouragement, and reassurance help decrease patient anxiety and thus pain perception.
2. Applying pressure or pinching skin near the site of injection stimulates local sensory A-fibers to inhibit stimuli from C-fibers conveying pain to the spinal cord, partially blocking the transmission of pain associated with injection.
3. Talk about other things with the patient while preparing supplies.
4. Do not show the needle/syringe to the patient.
5. No surprises – tell the patient that you will let them when you are going to do the injection.
6. Don’t try to minimize the effect with words like “little pinch”.
7. Don’t tell the patient about an upcoming injection before leaving the room to go get supplies.
B. Prior application of topical anesthetic (e.g., eutectic mixture of local anesthetics [EMLA]) decreases pain associated with injection.
C. Buffer solution with sodium bicarbonate (e.g., mix nine parts of LA with one part of sodium bicarbonate).
D. Warm the anesthetic solution to body temperature.
E. Use small gauge needle (25G or smaller).
F. Inject slowly and steadily.
G. Use the smallest volume of solution as possible.
H. Injecting into the subcutaneous tissue is less painful than infiltrating directly into the dermis.
I. Infiltrate through wound edges or introduce needle into previously anesthetized tissue (e.g., during field block).
J. Block nerves directly. A good knowledge of peripheral nerve anatomy helps avoid large volumes of LA.
II. UPPER EXTREMITY BLOCKS
A. Axillary block
1. Anesthetize the brachial plexus for procedures involving the elbow, forearm, and hand.
2. The axillary nerve and musculocutaneous nerve (which contains fibers of the lateral antebrachial cutaneous nerve) emerge from the plexus above the puncture site and may be incompletely anesthetized.
3. With the patient lying supine, the arm is abducted 90 degrees and positioned on a cushioned surface in a relaxed manner.
4. The course of the axillary artery of the medial upper arm can be palpated dorsal from the medial bicipital groove.
5. Palpate the axillary arterial pulse and follow it proximally until it disappears under the pectoralis major.
6. The puncture site is located slightly above the axillary artery, at the highest point in axilla and slightly beneath the pectoralis major muscle.
7. After disinfection and infiltrating the puncture site with LA, the needle is inserted parallel to the axillary artery at a 30-degree angle to the skin.
8. The needle is advanced with index finger over the pulse until either.
a. A distinctive “click” is heard, consistent with penetration into the plexus sheath.
b. Paresthesia is elicited in the median, ulnar, or radial nerve distribution.
c. Arterial blood is aspirated; inject half of the LA behind the artery by advancing the needle and the other half in front of the artery.
d. An attached nerve stimulator indicates needle tip placement within the sheath.
B. Bier block
1. Useful for procedures involving the forearm and hand
2. Technique
a. Place a double tourniquet on the upper arm and a peripheral IV distally.
b. Elevate the arm and exsanguinate with an ACE wrap all the way from the fingers to the tourniquet.
c. Inflate the proximal tourniquet and then remove the ACE bandage.
d. Slowly inject LA through the peripheral IV.
e. After 20 minutes (or sooner for patient discomfort), inflate the distal tourniquet and deflate the proximal one.
3. Anesthesia lasts as long as the tourniquet is inflated (maximum of 2 hours).
4. *Watch for signs of systemic toxicity caused by faulty tourniquet.
5. If a procedure lasts under 20 minutes, tourniquet deflation should be done in stages to avoid LA toxicity via IV bolus of anesthetic.
C. Wrist block
1. Median nerve block
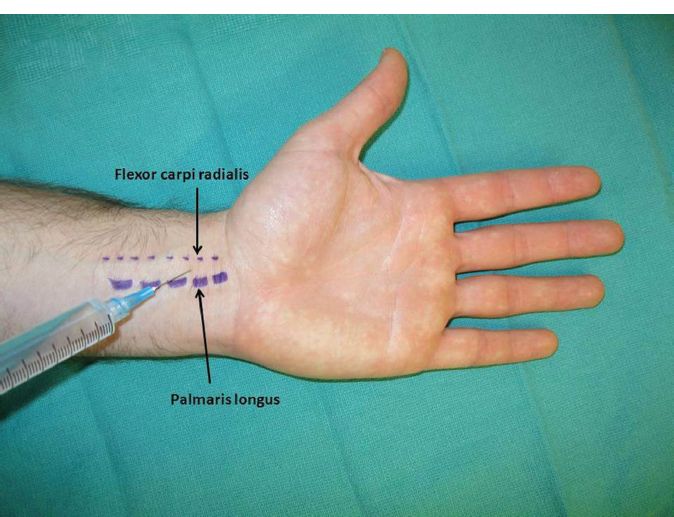
a. *The median nerve lies between the palmaris longus (PL) and flexor carpi radialis (FCR) (Fig. 10-1).
b. The PL is identified easily when the patient’s thumb is opposed to the little finger as the wrist is slightly flexed.
c. The injection is performed by introducing the needle between the PL and the FCR 2 to 3 cm proximal to the proximal crease of the wrist.
d. Inject after feeling penetration through the flexor retinaculum.
e. If there is no PL (in 15% of hands), inject on the ulnar side of the FCR.
f. Avoid direct injection into the nerve by asking the patient to report any paresthesias.
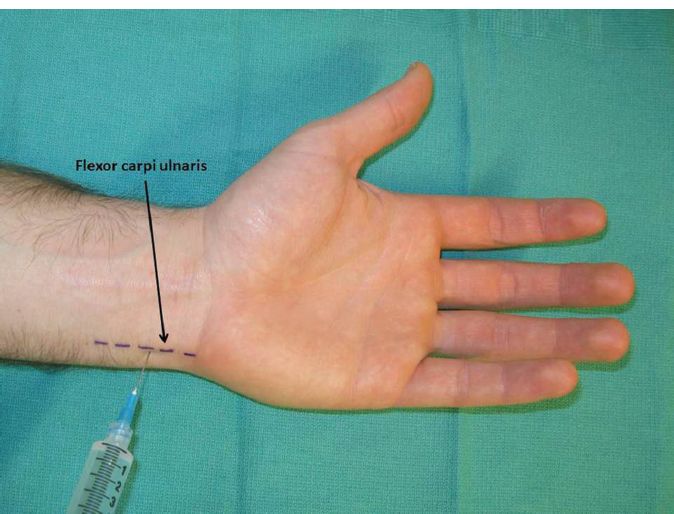
2. Ulnar nerve block
a. The ulnar nerve is located just radial to the flexor carpi ulnaris (FCU) at the wrist crease (Fig. 10-2).
Figure 10-1. Median nerve block.
Figure 10-2. Ulnar nerve block.
b. The FCU can be palpated over the ulnar side of the wrist when the wrist is slightly flexed.
c. The ulnar artery is located just radial to the ulnar nerve. Given its close proximity to the nerve, one should always aspirate prior to injection.
d. Injection is performed by introducing the needle ulnar and dorsal to the FCU.
e. The dorsal cutaneous nerve is blocked by subcutaneous infiltration extending from the injection site to the mid-dorsum of the wrist.
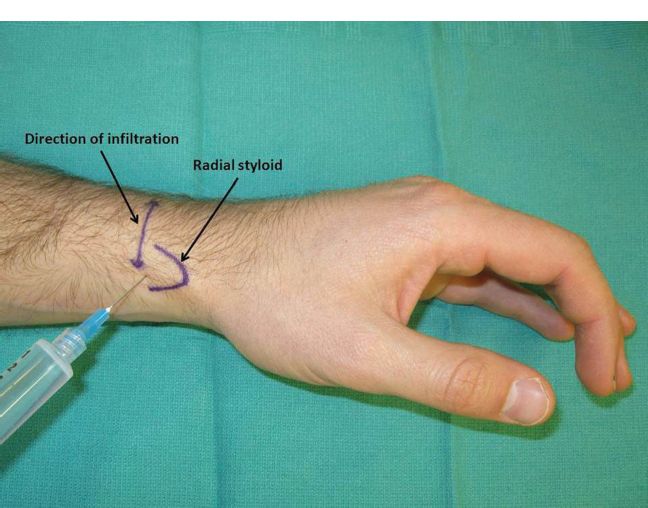
3. The radial nerve (sensory branch) block
a. The superficial radial nerve is divided into several branches at the level of the radial styloid (Fig. 10-3).
b. Local anesthesia is injected subcutaneously from the first to the third extensor compartment at the level of the radial styloid.
D. Digital block
1. Anatomy
a. The common digital nerves branch at the distal palmar crease and lie volar to the flexor tendons.
b. The digital arteries and nerves change orientation when entering the digits, with the nerve coming to lie volar to the artery in the digits.
c. The radial digital nerve to the thumb crosses the A1 pulley.
2. Dorsal sensory branches should also be anesthetized
3. Dorsal approach (Fig. 10-4)
a. Subcutaneous wheal over the extensor tendon to block the dorsal nerves.
b. Two injections are made at the level of the distal palmar crease, one on either side of the digit—advance the needle until the tip approaches the palmar skin surface and then withdraw while injecting slowly.
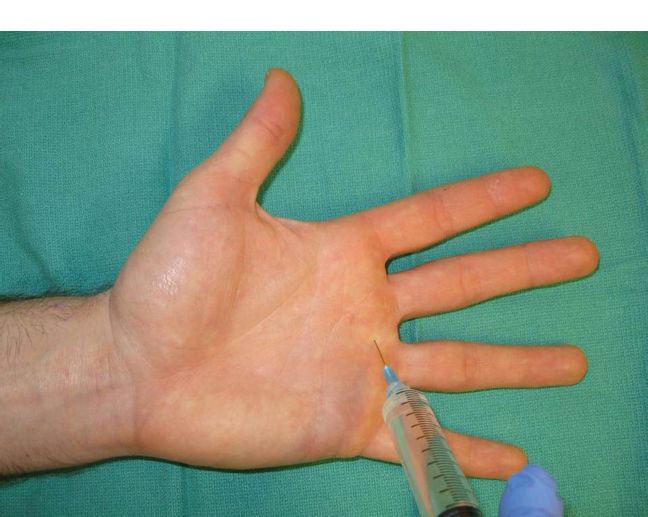
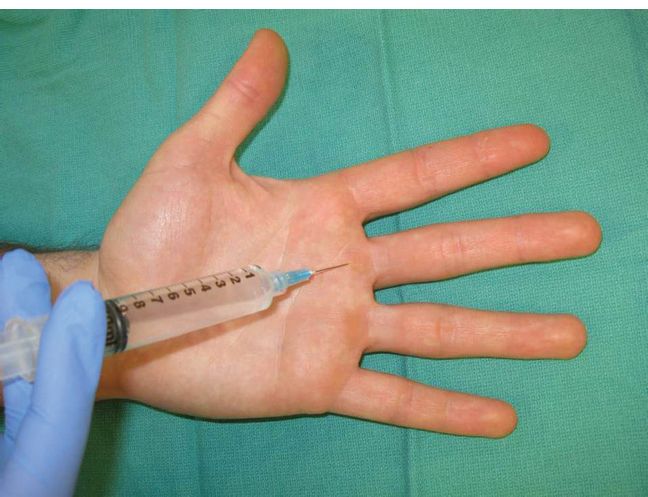
4. Volar approach (Fig. 10-5):
a. The needle is inserted vertically down to the flexor tendon. A subcutaneous wheal is placed directly over the flexor tendon and then laterally near the digital neurovascular bundles.
Figure 10-3. Radial sensory nerve block.
Figure 10-4. Digital block—Dorsal approach.
Figure 10-5. Digital block—Volar approach.
Figure 10-6. Digital block—Sheath approach.
5. Sheath approach (Fig. 10-6)
a. At the level of the palmar digital crease, the flexor sheath is easily palpable.
i. Insert the needle vertically through the flexor tendon, down to the bone.
ii. With slight pressure on the syringe plunger, withdraw the needle slowly until there is a loss of resistance, indicating injection into the potential space of the flexor sheath.
iii. Inject a few milliliters of LA.
iv. A fluid wave can be sometimes felt distally over the sheath.
b. This technique reliably results in digital anesthesia with one injection, but is not very effective in cases of sheath violation, such as distal amputation.
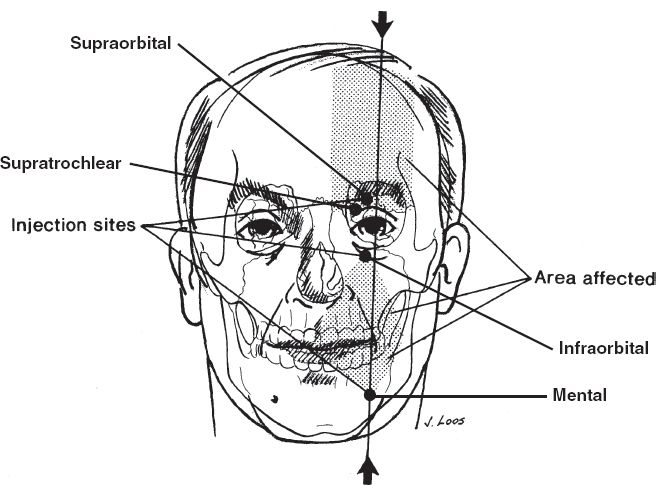
III. FACIAL BLOCKS (FIG. 10-7)
A. Supraorbital nerve
1. The supraorbital nerve exits the supraorbital foramen at the superior orbital rim at the mid-pupillary line (approximately 2.5 cm from midline).
2. Palpate the supraorbital notch just under the mid-portion of the eyebrow and inject 2 to 3 mL; avoid injection into the foramen.
B. Supratrochlear nerve
1. The supratrochlear nerve lies along the upper medial corner of the orbit approximately 1 cm lateral to midline and 1.5 cm medial to supraorbital notch.
2. Inject just lateral to the root of the nose in the medial portion of the orbital rim.
3. Both the supraorbital and supratrochlear nerves can be blocked by horizontal infiltration 2 cm above the eyebrow.
C. Infraorbital nerve
1. The infraorbital nerve innervates the ipsilateral lower eyelid, nasal sidewall and ala, upper lip, and medial cheek.
2. An upper buccal sulcus or external approach may be used.
3. The infraorbital foramen is just medial to the mid-pupillary line approximately 0.7 to 1 cm below the infraorbital rim.
Figure 10-7. Supraorbital, infraorbital, and mental nerve block. (From Fischer JE, ed. Mastery of Surgery. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2012.)
4. For the intraoral approach, advanced the needle through the upper buccal sulcus in between the canine and first premolar for about 1 cm, at which point 1 to 2 mL of anesthetic is injected just over periosteum.
D. Mental nerve
1. Innervates the lower lip and chin.
2. May be approached transorally or transcutaneously.
3. The mental foramen is located approximately 2.5 cm lateral to the midline just medial to the mid-pupillary line and midway along the height of the mandible.
4. For the intraoral approach, advance the needle at the lower buccal sulcus between the first and second premolar, aiming at the apex of the second premolar root.
E. Nasal anesthesia
1. External sensation is supplied by the infratrochlear (V1), external nasal (V1), and infraorbital (V2) nerves. Technique:
a. LA is injected along a line that starts from the nasolabial fold, continues lateral to the ala and along the base of nasal sidewall, and ends at the radix.
b. Inject cranially and caudally for a regional block.
2. Internal sensation is supplied by the inferior posterior nasal nerve, superior posterior nasal nerves, nasopalatine nerve, and branches of the ethmoidal nerves. Technique:
a. Either cotton pledgets dipped in 4% cocaine are placed directly on the nasal mucosa or LA is infiltrated directly between the mucosa and perichondrium. Oxymetazoline nasal spray (Afrin) may also be used as a vasoconstrictor to improve hemostasis during intranasal procedures.
1. External ear is supplied by
a. Auricular branch of the vagus nerve (Arnold’s nerve)
b. Auriculotemporal nerve
c. Lesser occipital nerve
d. Great auricular nerve
2. Technique
a. Perform a field block via two injection sites cranially and caudally.
b. Inject anteriorly and posteriorly around the ear either in a ring-like fashion or in a diamond-shaped pattern.
c. May be difficult to obtain adequate anesthesia for the auditory canal and tympanic membrane.
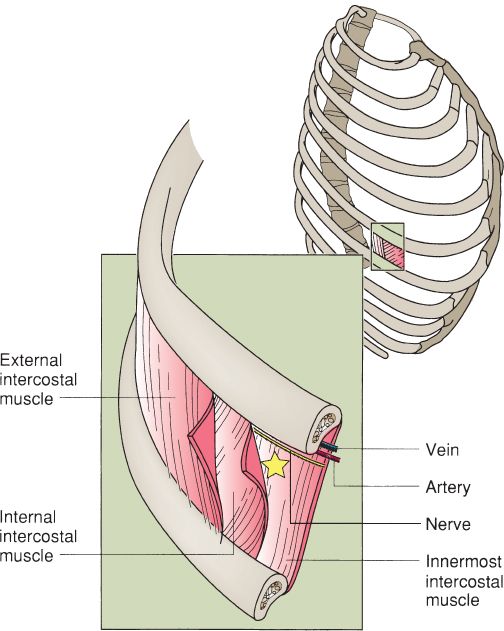
IV. INTERCOSTAL BLOCK (FIG. 10-8)
A. Provides anesthesia for chest and upper abdominal procedures.
B. The second through seventh intercostal nerves are anesthetized.
C. Anatomy
1. The neurovascular bundle lies in the subcostal groove
2. At the mid-axillary line, the rib is relatively superficial and easy to palpate
3. *The intercostal vein is most superior (mnemonic: VAN = vein/artery/nerve)
D. The patient is placed supine with the arms abducted.
E. After negative aspiration of blood, injection of 3 to 5 mL of the LA is performed inferior to each rib in the mid-axillary line.
Figure 10-8. Intercostal nerve block. The star indicates site of injection. (From Mulholland MW, ed. Greenfield’s Surgery. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2011.)
F. Additional subcutaneous infiltration is occasionally necessary
1. Superomedially, for superficial cervical plexus.
2. Midline, due to crossing innervation of the intercostals.
G. Complications include intravascular injection and pneumothorax.
TOPICAL ANESTHESIA
I. COCAINE
A. Used for topical anesthesia and vasoconstriction for surgery of the nose, throat, and oral cavity.
B. Absorbed rapidly through mucous membranes.
C. Topical solution strengths include 4% and 10%.
D. Concentrations greater than 4% are generally not recommended due to difficulty in controlling dosage and increased risk of toxicity.
E. The safe maximum dosage is reported to be 2 to 3 mg/kg.
1. Depends on the rate of absorption.
2. Spraying cocaine on surgical site leads to a more rapid absorption than application by pledgets.
3. Approximately one-third of the cocaine solution on pledgets is absorbed via the nasal mucosa.
F. Technique
1. Soak cotton pledgets in 4% cocaine solution. After being wrung out, use bayonet forceps to place pledgets in the nasal cavity, flush with the mucosa.
2. Apply three pledgets per side.
3. Wait 10 to 15 minutes before removal.
II. EMLA (EUTECTIC MIXTURE OF LOCAL ANESTHETICS):
A. Indicated for use on normal intact skin or genital mucosa for superficial minor procedures.
B. Useful in children to minimize discomfort prior to injections or starting an IV
C. Consists of a eutectic mixture of 2.5% lidocaine and 2.5% prilocaine formulated as an oil-in-water emulsion.
D. Duration and depth of pain blockade are both a direct function of the application time.
1. Acceptable dermal analgesia is achieved 1 hour after application. Anesthesia reaches a maximum at 2 to 3 hours and persists for 1 to 2 hours after removal.
2. Absorption is improved when applied under an occlusive dressing.
E. No local or systemic toxicity, but methemoglobinemia is a potentially life-threatening adverse effect in infants.
III. LMX4
A. Used to relieve pain caused by minor cuts, minor burns, sunburn, or insect bites, or prior to venipuncture.
B. Consists of 4% lidocaine delivered in liposomal vehicles, which enhances dermal penetration.
C. Similar to EMLA but faster onset and longer duration.
IV. VISCOUS LIDOCAINE
A. Used on mucosal surfaces to treat aphthous or radiation-induced ulcers or applied prior to performing an intraoral block.
B. Comes in 2 % solution. Used alone or in a compounded mixture as a mouthwash.
C. Anesthesia is achieved within 5 minutes. Duration of anesthesia is approximately 20 to 30 minutes.
V. LET
A. Useful for laceration repair; absorbs through the open surface of a wound.
B. Consists of Lidocaine 4%, 0.1% Epinephrine, and 0.5% Tetracaine in liquid solution.
C. Replaces tetracaine-adrenaline-cocaine (TAC).
D. Apply 1 to 3 mL to laceration with cotton swab. Apply remainder of dose to gauze and secure for 20 to 30 minutes.
A. Method of delivering a topical anesthetic using a low-voltage current to drive the transdermal delivery of lidocaine.
B. Lidocaine-soaked sponges are applied to intact skin, and electrodes are placed on top.
C. A low-voltage DC current is then applied to the skin.
D. Anesthetic effect occurs within 10 minutes and lasts approximately 15 minutes
E. The depth of anesthesia can reach up to 1 to 2 cm.
F. Disadvantages: Limited to small surface area, superficial burns are possible, and the equipment is comparatively complex.
PEARLS
1. Always verify anesthetic doses when solutions are prepared by others.
2. Wait 7 minutes after injection to allow epinephrine to take its hemostatic effect.
3. Perform injections with patients supine to avoid vasovagal response.
4. Premedicate children with ELA-Max or EMLA covered by occlusive dressing prior to injection or venipuncture.
QUESTIONS YOU WILL BE ASKED
1. How is epinephrine-induced digital ischemia treated?
Phentolamine
2. What are the key maneuvers that can be performed to minimize patient discomfort while administering LAs?
See Section I under nerve blocks. Maneuvers to minimize patient discomfort include reassurance and distraction, topical anesthesia prior to injection, buffer solution, warm solution, small gauge needle, slow injection, small volume, inject into subcutaneous tissues, inject in previous anesthetized tissues, and direct nerve blocks
3. What is the maximum dose of a mixture of 1% plain lidocaine and 0.5% bupivacaine that can be given to a 70-kg male? A 15-kg child?
Maximum doses
a. 70-kg male: 35 mL of 1% lidocaine, 35 mL of 0.5% bupivacaine
b. 15-kg child: 7.5 mL of 1% lidocaine, 7.5 mL of 0.5% bupivacaine
4. Name examples of amino-ester and amino-amide LAs, and what is the most clinically relevant difference between the two classes?
The major clinical difference between amino-amides and amino-esters is the potential for allergic reaction
a. Amino-amides examples: Lidocaine, mepicacaine, bupivacaine, ropivacaine, etido-caine, prilocaine
b. Amino-esters examples: Cocaine, chloroprocaine, procaine, tetracaine
5. What influences the duration of action of LAs? The potency? The time of onset?
The duration of action of an LA increases as its affinity for binding proteins increased. A higher pH increases binding protein affinity and a lower pH decreases affinity. Potency of an LA increases with increased lipid solubility. The pKa determines the rate of onset. The lower the pKa, the higher the concentration of nonionized LA at a given pH, and therefore, the faster the onset.
Recommended Readings
Chowdry S, Seidenstricker L, Cooney DS, Hazani R, Wilhelmi BJ. Plast Reconstr Surg. 2010; 126(6):2031–2034. PMID: 20697319.
Molony D. Adrenaline-induced digital ischaemia reversed with phentolamine. ANZ J Surg. 2006;76(12):1125–1126. PMID: 17199703.
Zide BM, Swift R. How to block and tackle the face. Plast Reconstr Surg. 1998;101(3):840–851. PMID: 9500408.
< div class='tao-gold-member'>