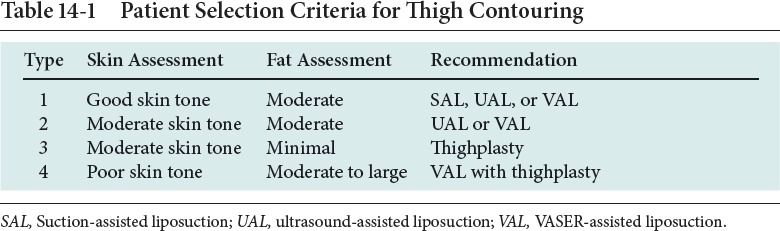
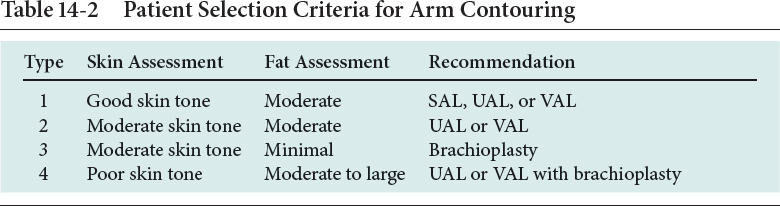
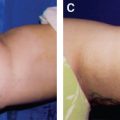
CHAPTER 14 The extremities are three-dimensional, cylindrical structures that exhibit an uneven distribution of compartmentalized fatty deposits. These deposits present contouring challenges that are not encountered in the trunk. It is generally agreed that circumferential contouring of the extremities yields a more harmonious aesthetic result than “spot” liposuction. This is true for both suction-assisted liposuction (SAL) and ultrasound-assisted liposuction (UAL). Rohrich et al assessed the efficacy of UAL compared with SAL for multiple anatomic sites in their 1998 textbook, Ultrasound-Assisted Liposuction. They rated the efficacy of UAL as good to excellent for the thighs and arms, fair to good for the calves, and fair to ineffective for the ankle area. Third-generation ultrasound devices were introduced to the field of liposuction in the early 2000s. The VASER (Solta Medical, Hayward, CA) third-generation UAL device became available in 2001 and has undergone several upgrades since then. It is currently capable of rapid fat emulsification while delivering significantly lower amounts of ultrasound energy to the tissues, particularly in the pulsed VASER mode. High ultrasound energy delivery to the tissues was implicated as the main source of complications encountered with the earlier generations of UAL devices. Numerous studies have since reported improved aesthetic results with low complication rates and minimal blood loss with the use of VASER-assisted liposuction (VAL). Because of the low complication rates, minimal associated blood loss, and greater ease of performing fine and detailed sculpting, I have used VAL for the majority of liposuction patients I have treated over the past 15 years. Currently the efficacy of VAL for contouring of thighs, calves, and arms could be rated as excellent. The efficacy of any type of UAL of the ankles is fair to poor at best; therefore UAL should not be used in this area. The majority of liposuction of the lower extremities (more than 95%) is performed on female patients. To achieve a harmonious and feminine aesthetic result for these patients, it is important to not dissociate the hips and the buttocks from the thighs. The typical anatomic areas of lipodystrophy in women are the lateral thighs (“saddlebag deformity,” the area inferior to the lateral gluteal depression and superior to the iliotibial tract), the superior medial thighs (the area that extends from the medial groin crease to the midmedial thigh zone of adherence), the infragluteal area (“banana roll deformity,” the area that extends from the inferior gluteal fold to the posterior thigh zone of adherence and blends laterally with the lateral thigh or saddlebag area), the medial knees, and the superoanterior thighs. As previously mentioned, circumferential liposuction is preferred over “spot” liposuction for aesthetic contouring of the extremities. The hip area should be included to create aesthetic proportions between the trunk and the thighs (see Chapter 13). Fig. 14-1 © 2017 Solta Medical, Inc. Used with permission. VASER and VASERsmooth are registered trademarks of Solta Medical, Inc. or its subsidiaries in the U.S. and in other countries. Liposonix is a registered trademark of Solta Medical, Inc. or its subsidiaries in the U.S. and in other countries. Areas to be avoided during liposuction of the thighs are the five zones of adherence: (1) the lower lateral thigh area of the iliotibial tract, (2) the gluteal crease, (3) the lateral gluteal depression, (4) the midmedial thigh area, and (5) the posterior distal thigh above the popliteal crease. Violation of these areas with ultrasonic probes or suction cannulas often leads to iatrogenic contour deformities. An exception to this rule may be the midmedial thigh zone of adherence, which may only be relatively contraindicated for liposuction. When there is significant thigh lipodystrophy, I frequently perform VAL to blend the superomedial thigh area with the medial knee region. Judicious fat extraction in the thighs improves their aesthetic contour and prevents contour deformities. In this patient, the typical areas of female lipodystrophy are marked in green, and the zones of adherence are marked in red. Gilliland and Lyos conceptually divided the arm into three regions—anteromedial, anterolateral, and posterolateral—for the purposes of planning upper extremity contouring procedures. The majority of the lipodystrophy in the upper extremity occurs in the posterolateral area of the arm. There is a modest amount of fat located in the anterolateral region and minimal fat in the anteromedial region. Liposuction is performed in the posterolateral and anterolateral regions. However, performing liposuction in the anteromedial region should be avoided in most cases. The pinch test in the anteromedial region commonly yields less than 1 cm, and fat extraction in this area will frequently lead to contour irregularities. Access incisions for arm liposuction, particularly with UAL or VAL, should be placed in the posterior axillary fold and the radial aspect of the elbow to avoid damage to the ulnar nerve. Both ultrasonic probes and suction cannulas are inserted longitudinally along the long axis of the arm. However, the surgeon needs to avoid moving the tip of the ultrasound probe into the ulnar area of the elbow when it is inserted proximally and avoid moving the tip of the probe into the axilla when it is inserted distally. The typical areas of upper extremity lipodystrophy are marked in green, and the areas to be avoided are marked in red. Anatomic Danger Zones Lower Extremity ■ Lower lateral thigh area of the iliotibial tract ■ Gluteal crease ■ Lateral gluteal depression ■ Midmedial thigh area ■ Posterior distal thigh above the popliteal crease Upper Extremity ■ Anteromedial region of the arm ■ Ulnar area of the elbow Patient selection has always been the most important consideration for liposuction. During the early evolution of SAL, plastic surgeons quickly learned that strict patient selection is essential to achieve consistently good aesthetic results while minimizing complications. The strict guidelines that must be followed include limiting the procedure to young, healthy individuals with good skin tone who are close to their ideal body weight and who have well-defined and localized areas of lipodystrophy. With the advent of third-generation UAL devices, plastic surgeons have been able to significantly expand the patient selection criteria for these procedures. With the use of VAL, I currently perform high-volume lipoplasty with acceptable results on healthy but significantly overweight patients with moderate skin tone and poorly defined areas of lipodystrophy. The best candidates for liposuction of the lower extremities are individuals who are close to their ideal body weight and who have a disproportionately high distribution of fat in the thighs and legs relative to the trunk. Lateral thigh fat (saddlebag deformity) is dense, fibrous, and covered by thicker dermis. Upper medial thigh fat is relatively loose, soft, and covered by very thin dermis. These anatomic differences make the lateral thigh a fairly forgiving area for the performance of liposuction, whereas the upper medial thigh is quite unforgiving. Poor patient selection and overextraction are the most common causes of inferior aesthetic results after liposuction of the inner thighs, and they usually result in significant skin laxity and visible contour deformities. Liposuction of the medial thighs should be avoided in patients with significant skin laxity or minimal fat distribution in the area (less than 2 cm on pinch test). These patients are best treated with an open excisional procedure such as a thighplasty. Extracting the fat through UAL or VAL in combination with thighplasty is a highly efficient technique for the treatment of skin laxity in patients with significant amounts of fat in the medial thighs. Performing fat extraction as a closed liposuction procedure in combination with a thighplasty allows the surgeon to limit the tissue undermining, which diminishes the empty space and preserves the lymphatic drainage; as a result, this minimizes seroma formation and the wound-healing complications associated with these procedures. VAL can be used to emulsify the fat before extraction while minimizing the amount of ultrasound energy delivered to the tissues. Numerous classifications have been proposed to improve the preoperative planning process for liposuction contouring of the arm. All of these classifications have in common a comparison of the relationship between excess arm fat and the excess skin envelope. However, poor skin tone—regardless of the amount of excess fat—usually dictates that the surgeon must perform a resection procedure to properly contour the arm. The same could be said for patients who display minimal excess fat, even with moderate skin tone. Occasionally, in patients with poor skin tone and a significant amount of excess fat, a combination procedure that employs UAL or VAL for fat extraction, followed by brachioplasty for skin resection, is a highly efficient method of correcting arm contour. The use of VAL is preferred over UAL when it is advantageous to use smaller-diameter ultrasound probes to deliver the least amount of ultrasound energy necessary to emulsify the fat that lies beneath a thin dermal cover. The algorithm for patient selection below mirrors that used when one is considering thigh liposuction procedures. Table 14-3 Patient Selection Criteria for Body Contouring
Liposuction of the Upper and Lower Extremities
Surgical Anatomy
Indications and Contraindications
INDICATIONS FOR LIPOSUCTION OF THE LEGS AND THIGHS
INDICATIONS FOR LIPOSUCTION OF THE ARMS
Patient Evaluation
Type | Characteristics | Recommendations |
1 | Good skin tone, well-defined lipodystrophy, minimal skin irregularities | SAL, UAL, or VAL |
2 | Decreased skin tone, generalized lipodystrophy, skin irregularities, fibrous areas | UAL or VAL |
3 | Skin redundancy and lipodystrophy | VAL with excisional procedures |
The decade of 2000-2010 brought technologic advances in ultrasound body contouring devices that allowed surgeons to expand the patient selection criteria for liposuction. However, one criterion that remains unchanged is the patient’s general health status. As with any elective aesthetic procedure, liposuction should only be offered to healthy individuals who are in relatively good physical condition. From a psychological point of view, it is imperative that the patient be capable of understanding the limitations of the procedure so that realistic expectations can be established regarding the expected outcome. After the patient meets the physical and psychological requirements for undergoing an elective aesthetic procedure, the surgeon will further determine his or her suitability for a liposuction procedure. The two most important factors are the amount of fat in the anatomic locations being considered for contouring and the quality of the overlying skin envelope. A classification for body contouring patients based on the amount of skin redundancy and lipodystrophy was described by Rohrich et al.
The patient is evaluated in the standing position. The lower extremities are examined from the anterior, posterior, and right and left lateral views. Typically the assessment of the upper extremities is performed from the anterior and posterior views with the arms abducted 90 degrees from the shoulder and the elbows flexed 90 degrees. The skin tone and lipodystrophy are evaluated. Any asymmetries and the presence of cellulite, telangiectases, contour deformities, striae, and varicose veins are noted. The findings should be documented preoperatively on a body contouring data sheet with body diagrams and then discussed with the patient.
Preoperative Planning and Preparation
Patients who are considering liposuction undergo an extensive consultation that includes a thorough medical history and a physical examination. It is important to take note of and discontinue commonly used nonprescription medications that may alter platelet function. It is also important to carefully examine risk factors that could potentially lead to deep vein thrombosis (DVT) and pulmonary emboli (PE) in these patients. In a survey of ASAPS members, Grazer and de Jong reported a mortality rate of 19 of 100,000 for patients undergoing liposuction, with approximately 25% of the deaths being the direct result of PE. In a survey by Teimourian and Rogers of more than 75,000 major liposuction procedures, there was a reported incidence of DVT of 33 out of 100,000 and a diagnosis of PE of 12 out of 100,000. Although the protocol for patients at high risk for DVT during excisional body contouring procedures should include prophylactic doses of low-molecular-weight heparin, many plastic surgeons do not use pharmacologic DVT prophylaxis for routine liposuction procedures because of the complications related to excessive bleeding during the procedure as well as increased postoperative bruising. Sequential pneumatic compression devices should be part of the routine protocol for major liposuction procedures.
The informed consent procedure requires that the surgeon provide the patient with the pertinent information about the proposed surgical procedure in a manner that allows the patient to make an informed decision about the surgery. In addition to the universal risks of undergoing surgery while under anesthesia, the patient must be informed of the following complications that may occur as a direct result of liposuction: bleeding, infection, contour deformities or asymmetry leading to the need for a secondary procedure, scarring, skin discoloration, sensory changes, seroma, PE, fluid overload (pulmonary edema), severe dehydration (shock), chronic pain, injury to deep structures, and skin and soft tissue burns during UAL. Serious complications associated with liposuction are rare. The most common complications are relatively minor and consist of contour deformities and asymmetries. As one would expect, the incidence of complications is higher among patients undergoing high-volume liposuction.
Consistent photographic standards are of paramount importance when planning body contouring procedures. Attention to details, such as lighting, backdrops, focal distance, and positioning, ensures accurate preoperative and postoperative photographic comparisons.