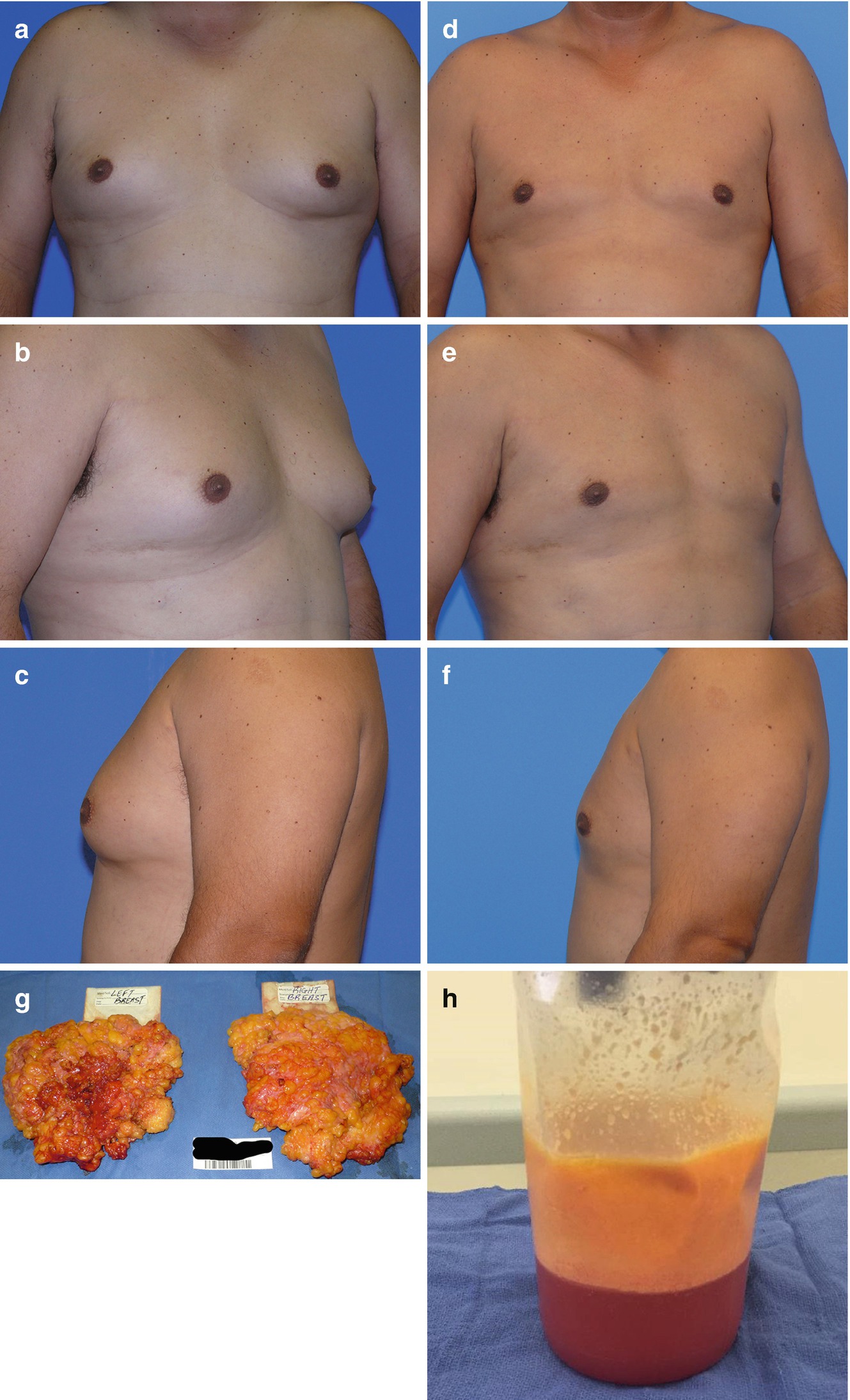
(a–e) Preoperative photography for gynecomastia includes anterior view, right and left oblique views, and right and left lateral views
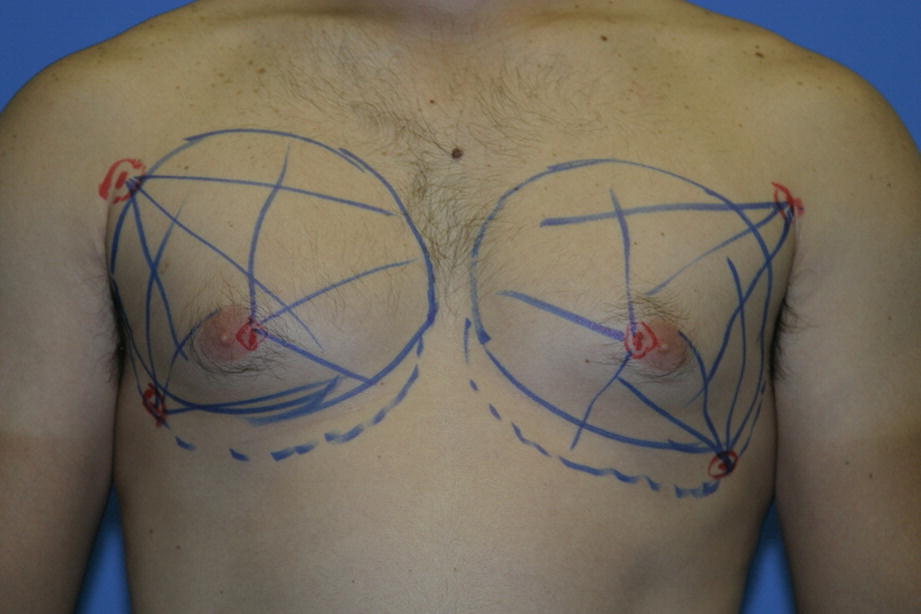
Typical preoperative markings for gynecomastia
Surgical Technique

Compression garment used postoperatively following gynecomastia surgery
Complications
During the informed consent process patients are advised of the possibility of postoperative hematoma, infection, visible scarring, nipple-areola depression deformity, contour irregularities, skin burns, and sensory changes to the nipples or breast skin. In reality complications are quite rare with this technique and the use of high amounts of epinephrine containing wetting solutions at room temperature has had a tremendous impact on avoiding the excessive bleeding and hematomas associated with the open techniques for treating gynecomastia.
Surgical Outcomes
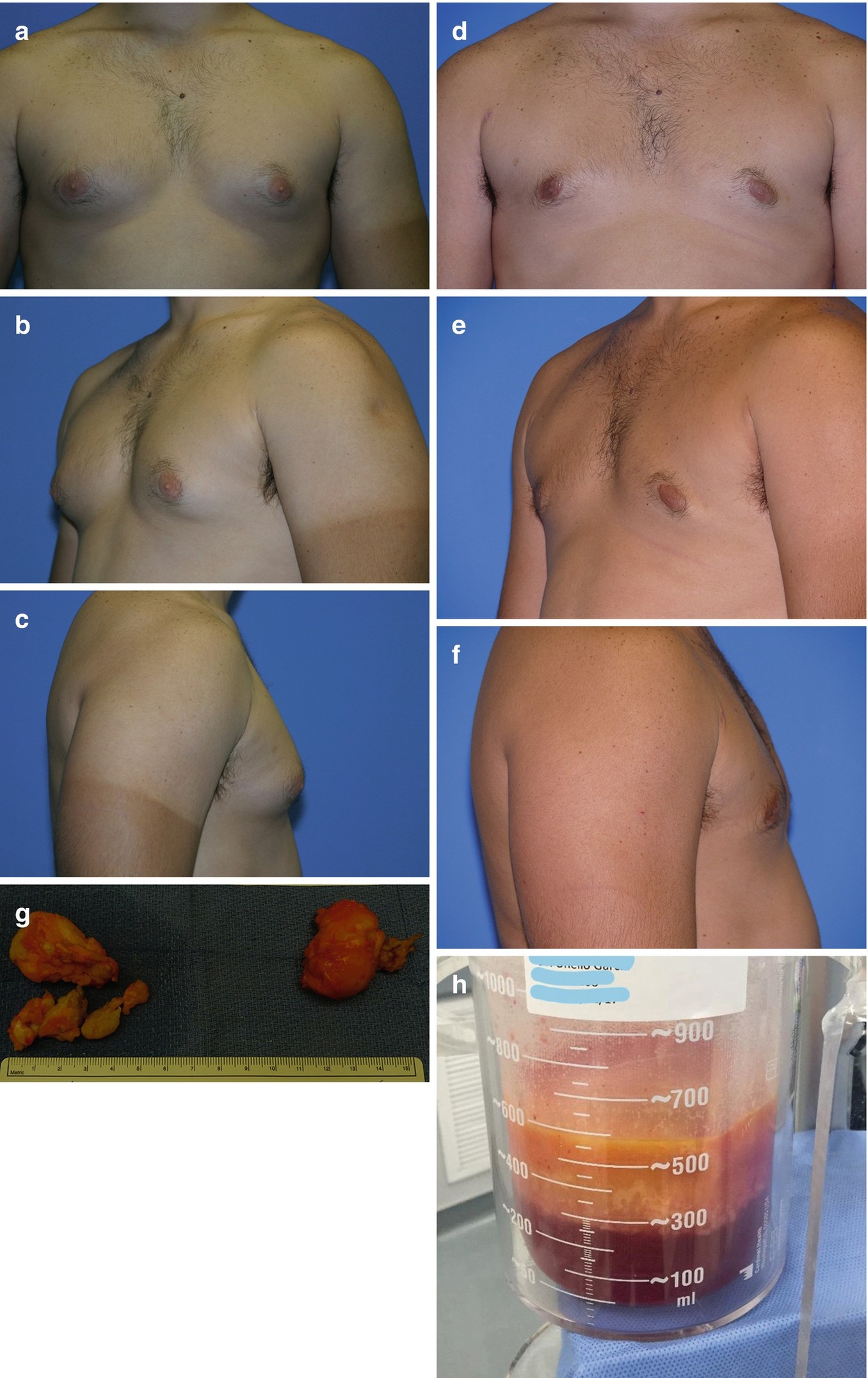
(a–f) Surgical outcomes at 6 months of 26-year-old male post-VASER-assisted resection of bilateral gynecomastia. (g, h) Surgical specimen of fibro-glandular tissue and VASER aspirate

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








