Liposuction for Treatment of Lymphedema
Dung Nguyen
Joseph Baylan
DEFINITION
Lymphedema is lymphatic transport alteration/damage resulting in the accumulation of proteinaceous fluid in the interstitial compartment.
Liposuction is the surgical removal of local excess fat from under the skin by vacuum suctioning using a cannula introduced through small skin incisions.
Dry liposuction is performed without the use of local anesthetic or dilute epinephrine.
Superwet liposuction uses a 1:1 mL ratio of infiltrate-toaspirate for large volume aspirate removal, decrease blood loss, avoidance of lidocaine toxicity, and to minimize resultant fluid shifts.
The pitting test refers to the amount of depression of the tissue (in millimeters) after the thumb is pressed as hard as possible on the extremity for 60 seconds.
Tissue edema that harbors more fluid will have more pitting and tissue edema that is mainly hypertrophied fat or fibrous tissue shows little or no pitting.
ANATOMY
Vital structures, such as neurovascular bundles and tendons that travel beneath the skin, can be injured during liposuction.
The key anatomical areas to avoid during liposuction in the upper extremity are the axilla, antecubital region, and the wrist.
In the lower extremity, liposuction at the femoral triangle, popliteal fossa, and ankles should be avoided.
Subcutaneous fat is divided into superficial, intermediate, and deep layer. Distribution of each layer varies depending on anatomical location and liposuction is carried out in the intermediate and deep layer.
Lymphatic capillaries are present in a subdermal plexus, which merge together into larger lymphatic vessels to form a complex network that carries lymph through the body. The lymph fluid enters a lymph node basin (ie, inguinal region, axilla) via several afferent lymph vessels where it is filtered and then transported toward the lymphatic ducts by efferent lymph vessels. Deep liposuction in the region of a lymph node basin can disrupt the lymphatic network and cause neurovascular injury.
PATHOGENESIS
Long-term accumulation of lymph fluid causes chronic tissue inflammation that induces excess differentiation of fat precursors, fat hypertrophy, tissue fibrosis, and hyperkeratosis.
Hypertrophied adipose tissue and tissue fibrosis are late signs of lymphedema.
PATIENT HISTORY AND PHYSICAL FINDINGS
Candidates for liposuction are those with late stage II (spontaneously irreversible) to stage III lymphedema (lymphostatic elephantiasis).
These patients have been treated and are refractory to complex decompressive physiotherapy (CDPT) and compression garments.
Physical examination:
Presence of nonpitting edema on pitting test.
Intact skin without open wounds.
No erythema or signs of infection.
Negative Homans sign, defined as calf pain with extension of the foot.
Treatment contract:
The success of the surgery relies on the patient being reliable and compliant with compression garment use 24/7 for life.
Patients who wish to proceed with surgery are asked to sign a treatment contract before surgery.
IMAGING
Dual-energy x-ray absorptiometry (DXA) is used to estimate the excess fat, muscle, and bone tissue in the lymphedema limb.
From the DXA scan, measurements are made in grams and transferred to volumes by density, which is useful in estimating the amount of excess fat to remove in patients scheduled for liposuction.
SURGICAL MANAGEMENT
Preoperative preparation:
Optimize nonsurgical therapy to reduce residual pitting edema in the tissue as much as possible prior to surgery.
Patients who have history of deep vein thrombosis (DVT) should get a baseline venous duplex study.
Appropriate preoperative evaluation of cardiopulmonary status is always indicated prior to any surgical procedure.
The patient must be aware of potential complications to include bleeding, infection, pain, numbness and tingling, contour irregularity, and wound healing problems.
Garments:
Two sets of garments are made to match the size of the normal limb (Juzo, class II 30-40 mm Hg): one set is given to the surgeon to put on the patient immediately after surgery; the other set, the patient will bring to the first postoperative clinic appointment.
Upper extremity garments include Juzo compression sleeve from wrist to axilla with shoulder strap and gauntlet.
Lower extremity garments include Juzo open toe compression stocking with adjustable waistband, toe cap, and biker shorts for compression of the thigh and hip area.
Donning device to aid in putting on and removing garments.
These garments are not sterilizable in the United States.
TECHNIQUES
▪ Anesthesia
General endotracheal anesthesia is preferred.
Epidural or peripheral nerve blockade performed by a regional anesthesia team is optional for postoperative pain management.
▪ Position
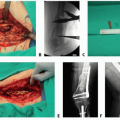
The patient is placed in supine position, and the affected extremity is rested on a hand table or a leg raise, respectively (TECH FIG 1).
During surgery, the extremity is raised with the help of an assistant to access the posterior surface of the limb.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree