LIP RECONSTRUCTION
I. FUNCTIONAL AND AESTHETIC GOALS
A. Oral competence is the primary goal of lip reconstruction. Specifically, this includes maximizing oral aperture, mobility, and sensation. Dribbling of saliva or food results from loss of lip function, sensation, or deficiency of the lower lip sulcus.
B. Restoration of static and dynamic symmetry. The lips are essential for facial expression and communication.
II. LIP ANATOMY
A. Layers: The lip consists of skin, a thin layer of subcutaneous tissue, orbicularis oris muscle, and mucosa
1. Vermillion
a. Unique tissue consisting of modified mucosa with relatively few underlying minor salivary glands
b. The “white roll” is the junction of the vermillion and the lip skin; *its continuity is critical during reconstruction because even a 1 mm step off is noticeable at conversational distance
c. The posterior vermillion line (wet-dry border) is where the upper and lower lips meet when the mouth is closed. This is the transition from oral mucosa to vermillion mucosa.
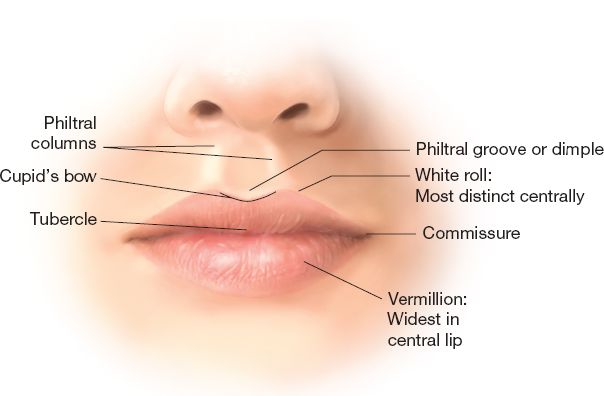
B. External anatomy (Fig. 21-1)
1. The lips are divided into four subunits
a. Philtrum: Between the philtral columns. The tubercle is the central portion of vermillion inferior to the philtrum.
b. Lateral wings: Between each philtral column and nasolabial fold
c. Lower lip: The entire lower lip is a single subunit
2. The labiomental fold separates the lower lip from the chin
3. The nasolabial folds confine the lateral extents of the upper lip
4. The normal intercommissural distance in an adult at rest is 5 to 6 cm. This width is approximately the distance between the medial limbi of the corneas. Ideally, this width should also equal the distance from the stomion to the menton.
C. Muscular anatomy
1. Orbicularis oris muscles
a. The primary muscles for closure of the lips.
b. Function as a sphincter for the oral cavity and also act to evert the lips.
c. Originate from the modiolus and decussate at the midline in the lower lip; in the upper lip the muscles cross the midline and insert into the opposite philtral column.
d. Innervation is by the buccal branches of the facial nerve.
2. The paired mentalis muscles
a. Principle elevators of the lower lip.
b. They arise from the lower border of the mandible and insert into the soft tissues of the chin below the level of the labiomental crease.
c. Innervation is by the marginal mandibular branch of the facial nerve.
______________
*Denotes common in-service examination topics
Figure 21-1. External lip anatomy.
3. Lip elevators
a. Include the paired levator anguli oris, levator labii superioris, zygomaticus major, and zygomaticus minor muscles.
b. Innervation is by the zygomatic and buccal branches of the facial nerve.
4. Lip depressors
a. Include the paired depressor anguli oris and depressor labii inferioris muscles.
b. Innervation is by the marginal mandibular branch of the facial nerve.
c. *The paired platysma muscles also provide some lateral lower lip depression (e.g., during full denture smile) and are innervated by the cervical branch of the facial nerve.
D. Sensation
1. Upper lip: The infraorbital nerve is the terminal branch of the maxillary division of the trigeminal nerve (V2) and exits the maxilla at the infraorbital foramen in line with the pupil and 1 cm inferior to the infraorbital rim
2. Lower lip: The mental nerve is the terminal branch of the mandibular division of the trigeminal nerve (V3) and exits the mandible at the mental foramen at the level of the second premolar.
E. Blood supply
1. Arterial
a. The superior and inferior labial arteries are branches of the facial artery. They form a rich vascular network that spans circumorally and allows for the design of multiple flaps for lip reconstruction.
b. *The labial artery usually lies between the orbicularis oris muscle and mucosa within the vermillion portion of the lip.
c. Superior labial artery is 10 mm from superior lip margin.
d. Inferior labial artery is 4-13 mm from lower lip margin.
2. Venous: Superior and inferior labial veins drain to the ipsilateral facial vein
F. Lymphatic drainage
1. *The upper lip and lower lateral lip segments drain into the submandibular nodes.
2. The central lower lip drains into the submental nodes.
III. APPROACH TO LIP DEFECTS
A. Etiology of lip defects: Cancer resection is the most common cause (>90%) and squamous cell carcinoma is the most common neoplasm.
1. *Vermillion cancers (anterior to wet-dry line) behave like cutaneous tumors, but those posterior to this landmark behave like intraoral tumors (higher risk of metastasis).
2. A surgical margin of 7 to 10 mm is recommended for squamous cell carcinoma. For basal cell carcinoma, a surgical margin of 2 to 4 mm is recommended.
B. Reconstruction of lip defects requires consideration of
1. What tissue is missing: Vermillion, skin, orbicularis muscle, and mucosa
2. How much of the lip is missing: The proportion of total lip tissue missing is often described in thirds, superficial versus full-thickness defect, involvement of commissure, and involvement of the philtrum.
3. Patient factors: Age of patient, tissue elasticity, lip redundancy, need for dentures, radiation, previous scars, tolerance for complex reconstruction, and general health status
4. Lip defects that involve >30% of the lip may result in microstomia if closed primarily. Microstomia is a difficult condition that impedes eating, use of dentures, and adequate oral hygiene.
IV. SUPERFICIAL LIP DEFECTS
A. Superficial defects of the skin: Usually do not cause functional deficits
1. Skin grafts can provide efficient coverage of superficial lip defects, but can result in inferior aesthetic results.
a. Split-thickness skin grafts contract more than full-thickness grafts.
b. Severe cases of retraction can lead to lip eversion and decreased oral competence.
2. Local tissue rearrangement techniques generally offer the best match in tissue thickness, color, and texture
a. Cheek advancement flaps combined with perialar excisions and lateral V–Y advancement flaps are commonly used for upper lip skin defects.
b. Lower lip defects are often resurfaced with rotational flaps (e.g., bilobed) and transposition flaps (e.g., rhomboid).
c. If the defect is confined to the philtrum, consider healing by secondary intention or full-thickness skin grafting.
B. Vermilion defects
1. General principles
a. Before infiltrating local anesthetic, use a fine-tipped pen and mark the superior and inferior edges of the white roll.
b. Lesions of the vermillion are preferentially excised perpendicular to the white roll in order to facilitate alignment of this landmark.
c. Local tissue rearrangements that involve skin only will require the use of one of the following techniques to repair the vermillion.
2. Techniques for reconstruction
a. Small defects can be treated with musculomucosal V–Y advancement flaps (generally horizontally oriented).
b. Large defects (such as after vermillionectomy for precancerous lesions) involving the entire vermillion can be resurfaced with a retrolabial mucosal advancement flap and dissected to the sulcus at a level between the orbicularis oris muscle and the accessory salivary glands, which are included in the mucosal flap
c. Staged procedures that borrow mucosa from the upper lip (e.g., bipedicled mucosa flap, cross lip mucosa flap).
d. Staged tongue flap: Dorsal tongue for upper lip and volar tongue for lower lip.
e. For superficial vermillion defects <30% of the lip, the vermillion–skin border can be incised and the vermillion can be directly advanced along the lip.
f. For more complex vermillion defects <30% of the lip, full-thickness excision can be performed.
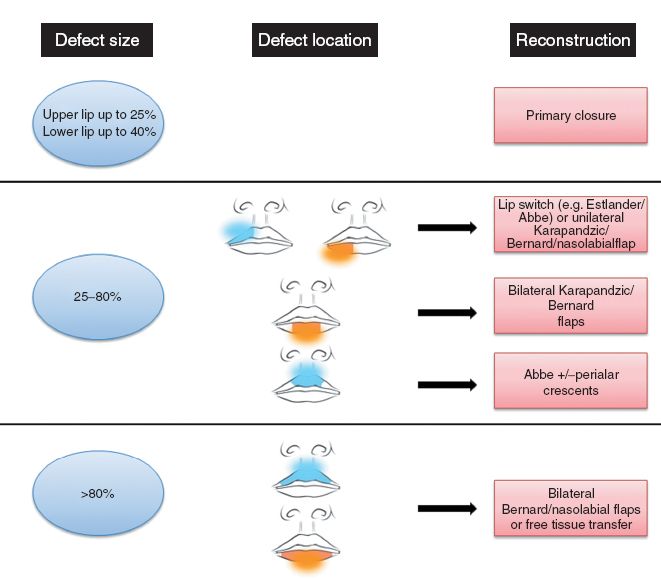
Figure 21-2. Reconstructive algorithm for full-thickness lip defects.
V. TECHNIQUES FOR FULL-THICKNESS LIP RECONSTRUCTION (FIG. 21-2)
A. Full-thickness defects up to one-third of the lip: Primary closure is most appropriate
1. Shield or wedge excision: Preferred design around lip lesion for excision. Can be modified into a “W” on the lower lip to limit the length of closure and prevent disruption of the labiomental or nasolabial creases.
2. Central upper lip defects involving the philtrum can be reconstructed with an Abbe flap to maintain aesthetic subunits.
3. Optimal repair and prevention of notching requires determined approximation of the orbicularis oris muscle, mucosa, white roll, dermis, and epidermis.
B. Defects of one-third to two-third of the lip
1. Primary closure with skin excisions
a. For defects slightly larger than one-third of the lower lip, bilateral labiomental crease excisions (Schuchardt procedure) can provide enough laxity for primary closure.
b. For the upper lip, bilateral perialar crescentic excisions with cheek advancement (Webster flaps) may allow for primary closure.
2. Lip-sharing techniques
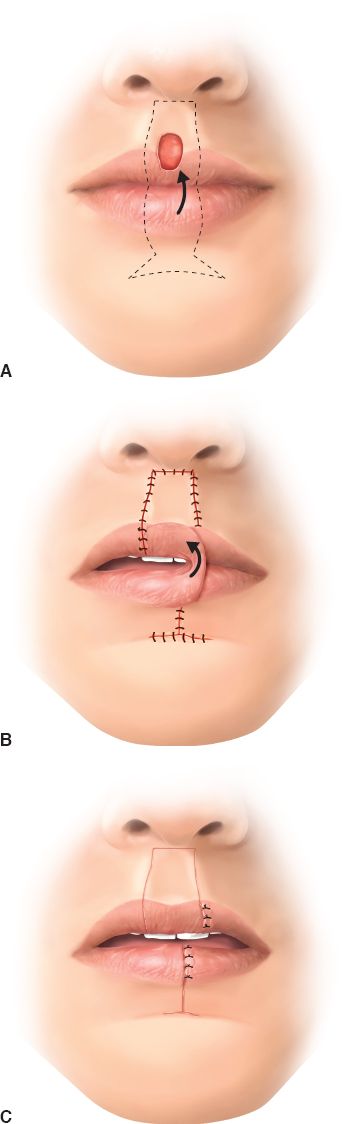
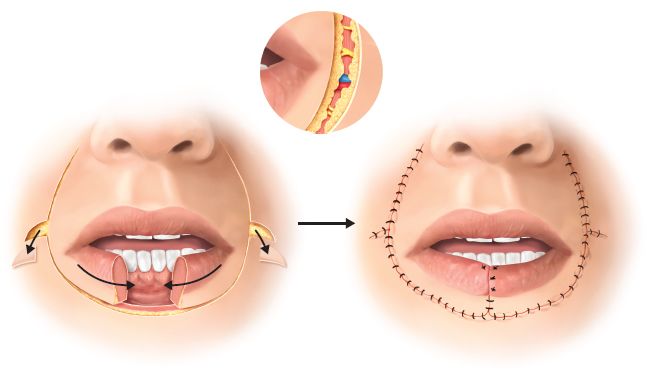
a. Abbe flap (Fig. 21-3): A two-staged lip-switch procedure where a full-thickness flap of up to one-third of the donor lip can be used to reconstruct up to a two-third defect of the recipient lip. The flap is rotated 180° on its pedicle (labial artery) and remains for about 3 weeks, when the pedicle is divided.
i. This technique can be utilized with upper and lower lip defects.
ii. Flaps are designed with their borders parallel to relaxed skin tension lines. The height of the flap should match that of the defect. The width of the flap should be about half of the defect (to allow for proportional reduction of both lips).
Figure 21-3. Abbe flap. A: An upper lip defect is being prepared. Complete excision of the lesion will produce a full thickness lip defect that can be reconstructed with an Abbe flap. Markings are shown. B: The Abbe flap has been rotated into the defect. The flap is perfused by the labial vessels. C: After two or three weeks the flap is divided and inset.
iii. Due to generous vascularity of the lip, the Abbe flap can be based on either a medial or lateral pedicle.
iv. Several millimeters of labial mucosa should be maintained around the pedicle to allow for venous drainage.
v. Despite denervation of the orbicularis oris muscle during harvest, motor and sensory function improves over the first year.
vi. In the upper lip, an Abbe flap can be used for either philtral or lateral lip reconstruction.
vii. An Abbe flap can be performed in conjunction with labiomental crease incisions or perialar crescent excisions for larger defects.
viii. In general, the artery is located at a level equivalent to the white roll on sagittal section.
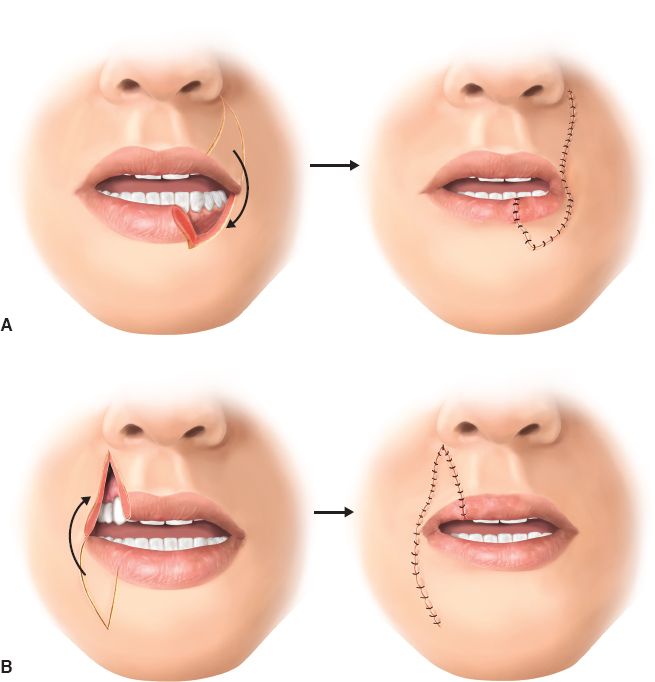
b. Estlander flap (Fig. 21-4): A medially based lip-switch technique that is indicated in lip defects that demonstrate commissure involvement
i. Principles of design similar to the Abbe flap. Again, the flap width should be about half the defect width for deficit balance.
ii. Flaps are designed so that incisions lie within the nasolabial fold and are used with upper and lower lip defects.
iii. Despite being a one-stage reconstruction, there is often blunting of the reconstructed commissure and patients often require commissuroplasty
Figure 21-4. A: Estlander flap. B: Reverse Estlander flap.
iv. Flap is not innervated and oral animation can be distorted.
v. Blood supply more tenouous than the Abbe flap because it comes from contralateral labial artery.
vi. Cuff of muscle should be maintained at rotation point to improve vascularity to flap.
3. Staircase technique: A one-stage operation most commonly used to reconstruct lower lip defects, but may also be used for upper lip defects
a. A series of steps are designed originating diagonally from the defect along skin creases. Full-thickness rectangles or squares of skin and subcutaneous tissue are excised under each step to allow for advancement of local tissue into the defect.
b. The number and dimensions of the necessary steps are determined by the size of the defect and available laxity
c. This technique does not require violation of the orbicularis oris muscle or the opposite lip
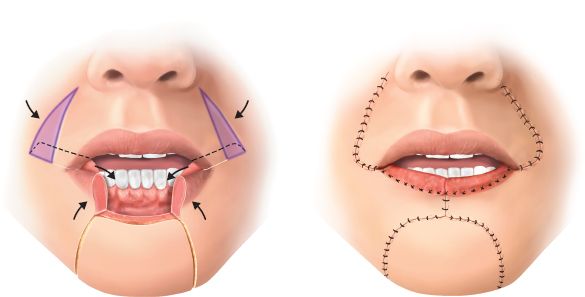
4. Karapandzic flap (Fig. 21-5): A modification of the Gillies’ fan flap, *this one-stage technique preserves motor and sensory function through meticulous dissection of the neurovascular pedicles and is ideal for large central defects of up to 80% of the lower lip
a. For lower lip defects, circumoral incisions are made extending from the defect and curve up around the commissures to include the nasolabial folds.
b. For upper lip defects, incisions are made along the nasolabial creases and extend down to the labiomental crease.
c. Bilateral opposing flaps are created and the incisions are limited to skin and subcutaneous tissue superficially and separate incisions to release the mucosa.
d. The intervening neurovascular structures are bluntly dissected out with scissors and preserved as the soft tissues are released to provide laxity to close the defect.
e. The Karapandzic flap may be used in cases with commissure involvement as the rotating donor lip tissue creates a new commissure.
f. Because it is often used for large lip defects, the Karapandzic flap may lead to blunting of the commissures and microstomia, which may require the use of lip-stretching appliances.
Figure 21-5. Karapandzic flap. The flap elements are incised and elevated (left). Small Burow’s triangles may be excised to facilitate rotation. The blood vessels and facial nerve branches are preserved (inset). The flaps are rotated into position and closed (right).
C. Subtotal and total lip defects
1. Combination of flaps
a. For the lower lip, two lateral Abbe flaps are used to reconstruct the lower lip while perialar crescent excisions with cheek advancement are used to close the upper lip Abbe donor sites.
b. For the upper lip, an Abbe flap from the lower lip is used to reconstruct the philtrum in addition to bilateral perialar crescent excisions with cheek advancement.
2. Karapandzic flap: Appropriate for very large defects if patients demonstrate sufficient tissue laxity.
3. Bilateral opposing cheek advancement: Many eponyms exist, but all are based on horizontal advancement of cheek skin with removal of Bürow triangles. Excisions involve skin and subcutaneous excisions only to protect neurovascular structures and preserve as much oral competence as possible. Buccal mucosa is used to reconstruct the vermillion.
a. Bernard–Burow for lower lip (Fig. 21-6): Two large Bürow triangles are excised lateral to the upper lip
b. Webster modification of Bernard–Burow for lower lip: Places triangular skin excisions adjacent and parallel to the bilateral nasolabial folds, resulting in scars that are within natural skin creases and avoids violating the aesthetic region of the chin
c. Bernard-Burow’s for upper lip: Four triangular skin excisions are needed, two perialar and two lateral to the lower lip
4. Nasolabial flap: A long segment of skin and subcutaneous tissue is transposed to reconstruct full-thickness defects of the upper or lower lip.
a. Requires a skin graft to line the inner surface at the first stage.
b. Flaps have a random blood supply and can be delayed if necessary.
c. Must account for significant contraction and therefore flaps should be made larger than the lip defect.
d. Reconstruction of the vermillion is necessary at a second stage.
e. Due to these limitations, this is not a preferred choice for subtotal or total lip reconstruction.
f. Blood supply thought to be from perforators off angular artery off of facial artery
5. Temporoparietal scalp flap
a. A regional option best suited for male patients providing full-thickness reconstruction.
b. Bilateral flaps based on the superficial temporal artery can be used for full lip reconstruction.
c. Like nasolabial flaps, a skin graft is needed to line the deep surface and the flaps can be delayed.
6. Free tissue transfer (e.g., radial forearm with palmaris longus tendon for static support for oral competence)
Figure 21-6. Bilateral modified Bernard–Burrow’s technique.
CHEEK RECONSTRUCTION
I. CHEEK ANATOMY
A. The cheek represents a relatively large area of the face delineated laterally by the preauricular skin, inferiorly by the mandibular border, medially by the nasal sidewall and nasolabial fold, and superiorly by the lower eyelid and temple
B. Several descriptions of subunits exist, but the most straightforward one divides the cheek into three subunits:
1. Suborbital: Between the nasolabial fold and anterior sideburn, lower eyelid, and gingival sulcus.
2. Preauricular: Between ear and malar eminence, includes masseteric and parotid fascia.
3. Buccomandibular: Between the gingival sulcus and the border of the mandible, includes oral lining.
C. Muscle: The muscles of facial expression are connected by a contiguous fibrous sheet known as the superficial musculoaponeurotic system (SMAS) which lies just deep to the subcutaneous layer. *Superiorly it is continuous with the temporoparietal fascia (also known as superficial temporal fascia) and inferiorly it is continuous with the platysma.
D. Innervation
1. Sensation to the cheek is mediated by branches of the maxillary (V2) and mandibular (V3) divisions of the trigeminal nerve.
2. Motor function to the muscles of facial expression is imparted by the facial nerve (VII), which travels underneath the superficial lobe of the parotid gland. More anteriorly, the distal branches are found just deep to the parotid masseteric fascia.
E. Blood supply
1. The cheek is supplied predominantly by the facial artery, which gives off the angular artery.
2. The transverse facial artery branches from the superficial temporal artery and supplies the cheek superiorly.
3. Distally, these anastomose with the infraorbital artery and infratrochlear artery.
F. Retaining ligaments
1. There are two areas along the cheek where the skin and soft tissues are relatively fixed to the underlying bone.
2. The zygomatic ligament is found on the zygoma, just posterior and inferior to the malar eminence.
3. The mandibular ligament is found along the jaw line just posterior to the chin.
4. These ligaments resist advancement of cheek skin and may require release to allow for closure of cheek defects.
II. PREOPERATIVE CONSIDERATIONS
A. Patient factors such as smoking, diabetes mellitus, immunosuppression, history of radiation, and prior scars may compromise wound healing or cause necrosis of local flap.
B. Defect size, complexity, surrounding skin quality, skin laxity, hair-bearing status, and orientation of relaxed skin tension lines all affect the selection of the most appropriate reconstruction.
C. After excision of aggressive tumors (e.g., melanoma), a simpler reconstruction such as healing by secondary intention, primary closure, or skin grafting may be preferred initially in order to allow for tumor surveillance.
D. Increased tension across the cheek will affect the appearance of neighboring facial units. For example, scar contractures of the cheek commonly result in traction on the lower eyelid or upper lip, causing ectropion.
III. RECONSTRUCTIVE OPTIONS
A. Secondary healing
1. Reserved for selected cases where the defect is small and there is a reason to not perform primary closure.
2. Larger defects left to heal secondarily risk significant scar contraction that will lead to distortion and asymmetry.
3. Secondary healing leads to superior results in flat or concave areas (e.g., temple, preauricular) as opposed to convex areas (e.g., malar eminence).
B. Primary closure: Small defects <1 cm in size can be reliably closed primarily, especially with skin undermining.
1. Elderly patients demonstrate increased skin laxity and therefore primary closure is often appropriate even for larger cheek defects.
2. In general, undermining up to 4 cm beyond the defect borders increases recruitment of surrounding tissue; further undermining does not contribute significantly to decreased wound closure tension.
3. Lesion excision and primary closure should be designed ideally along the relaxed skin tension lines.
4. Some lesions are positioned perpendicular to the relaxed skin tension lines: In these cases, it is better to accept an unfavorably oriented scar than to create a much longer scar within the relaxed skin tension lines.
C. Skin grafts: Often the most efficient technique for covering larger cheek defects, skin grafts usually result in a poorer cosmetic outcome compared to local flap reconstruction
1. Skin grafts are considered in unhealthy patients who cannot tolerate more complex reconstructive surgical options and patients who require surveillance for recurrence of aggressive tumors
2. Healed skin grafts on the cheek will demonstrate a patch-like appearance, color mismatch, and contour deformity. However, skin grafting is a preferred technique for temporal defects.
3. Full-thickness skin grafts will result in less secondary contraction and should be used whenever possible. When split-thickness grafts must be used, a thick nonmeshed graft should be harvested to optimize cosmesis.
D. Local tissue rearrangement (see Chapter 4: “Flaps”): Local flaps are useful for moderate (2 to 3 cm) and large (>3 cm) cheek defects. When designing a local flap, it is critical that the vector of maximum tension after closure of the donor site is not in an unfavorable direction (e.g., pulling down the lower eyelid predisposing to ectropion). Often, many surgical options will serve to close a cheek defect; the most appropriate reconstruction depends of the aforementioned preoperative considerations.
1. Transposition flaps: These versatile reconstructions capitalize on the substantial mobility of the cheek skin. Skin and subcutaneous tissue are borrowed from adjacent areas of relative laxity and the donor site is closed primarily. With careful planning of incisions and donor site tension, drawbacks such as complex scarring, trapdoor deformity, and irregularity in hair pattern can be minimized.
a. Banner flap
i. Simple transposition flap.
ii. Final scar is placed along the relaxed skin tension lines of the cheek and the apex of the banner is usually excised.
iii. Not the ideal choice because it typically results in a standing cutaneous deformity.
b. Rhomboid flap
i. Commonly used for coverage of defects on the lateral cheek and jawline.
ii. The classic rhomboid flap requires conversion of the defect to a rhombus with 60 and 120 degree angles.
iii. The donor flap is drawn from one of the 120 degree angles. The flap must be designed so that the vector of maximum tension after donor site closure is placed favorably.
iv. Disadvantage: Multiple incisions create one or more scars that lie perpendicular to lines of relaxed skin tension.
c. Bilobed flap
i. Modification of the banner flap, the bilobed flap uses a second secondary flap to help close the donor site of the primary flap.
ii. A pivotal arc of 90 to 110 degree is commonly used.
iii. These flaps may be used along the lateral and inferior cheek.
iv. Given the complex scarring, these flaps are generally not a first choice in cheek reconstruction.
2. Cheek advancement flap
a. Useful for preauricular defects, a flap of cheek tissue can be directly advanced into the defect with excision of Bürow triangles at the base.
b. Variations of this advancement technique may be utilized depending on defect characteristics. One example is the O-T flap, where a circular defect is converted into two opposing advancement flaps and the intervening standing cutaneous deformity is excised.
3. V–Y advancement flap
a. Appropriate for defects of the medial cheek, alar base, and along the nasolabial fold, this flap survives on perforators within the subcutaneous pedicle.
b. The flap may be designed with curved limbs that lie along the natural rhytids. With care, this flap is well-suited for infraorbital defects, with low rates of ectropion and significant advantages over Mustardé-type flaps.
c. Sufficient subcutaneous dissection around the V–Y flap is required to achieve adequate mobilization for closure.
E. Regional flaps
1. Cervicofacial flap
a. Large (>4 cm) medial cheek defects that are inappropriate for other local tissue rearrangement options can be repaired with a cervicofacial flap.
b. Various designs of cervicofacial flaps may be used depending on the size and location of the defect and flaps may be based superiorly or inferiorly
c. Often a standing cutaneous deformity will need excision
d. Mustardé flap (Fig. 21-7)
i. For defects close to or including the lower eyelid, the incision may be carried into either the subciliary line or the inferior orbital rim.
Figure 21-7. Mustardé cervicofacial flap.
ii. The incision is then taken beyond the lateral canthus and curves superiorly before extending inferiorly into the preauricular crease.
iii. The flap should be anchored to the deep temporal fascia above the lateral canthus to reduce tension on the repair and to prevent ectropion.
e. Cervicopectoral flap
i) Useful for very large cheek defects requiring significant advancement and rotation of donor tissue.
ii. Incisions are similar to a Mustardé flap but are extended onto the lower neck posteriorly and then over the clavicle anteriorly.
iii. Anchoring sutures to inferior orbital rim periosteum and temporary Frost sutures can help prevent ectropion.
F. Tissue expansion
1. Provides skin that has good color and texture match and is well-vascularized and sensate to resurface large cheek defects.
2. Tissue expansion in the head and neck region is associated with high complication rates.
3. Usually, lateral cheek and upper neck skin can be expanded to resurface defects resulting from excision of scars, large benign lesions, or previous skin grafts.
G. Free flaps
1. Reserved for complex cheek defects involving multiple tissue layers or patients who are not suitable candidates for local tissue rearrangements, such as patients with facial burns, patients who have had neck dissection, or patients demonstrating significant radiation dermatitis.
2. A classic choice is the radial forearm free flap which is usually harvested with palmaris longus tendon for lip support.
PEARLS
1. When planning lip reconstruction, think about: What tissue is missing? How much of the lip is missing? What are the relevant patient factors?
2. Before injection of local anesthetic into a lip or around a skin lesion, always think, “Do I need to first mark the vermillion border or the edges of this lesion?”
3. When a cheek defect is close to the lower eyelid, always consider the vector of pull and the risk of ectropion
4. Be able to sketch various options for local flap designs (and their resultant scars) to reconstruct defects of the lip and cheek
5. For any given cheek defect, be able to list several possible reconstructive choices; know the pros and cons of each option
QUESTIONS YOU WILL BE ASKED
1. In the elderly, why is it important to consider oral stoma size when planning the reconstruction?
To ensure postoperative denture placement.
2. In order to reduce the risk of postoperative ectropion, what structure can the cervicofacial flap be anchored to?
Deep temporal fascia.
3. What is the most common complication of the Karapandzic flap?
Microstomia.
4. What secondary procedure do Estlander flaps sometimes require? Commissuroplasty to correct rounded commissure.
THINGS TO DRAW
Draw the surface anatomy of the lips.
See Figure 21-1.
Recommended Readings
Anvar BA, Evans BC, Evans GR. Lip reconstruction. Plast Reconstr Surg. 200715;120(4):57e–64e. PMID: 17805106.
Coppit GL, Lin DT, Burkey BB. Current concepts in lip reconstruction. Curr Opin Otolaryngol Head Neck Surg. 2004;12(4):281–287. PMID: 15252247.
Menick FJ. Reconstruction of the cheek. Plast Reconstr Surg. 2001;108(2):496–505. PMID: 11496195.
Schulte DL, Sherris DA, Kasperbauer JL. The anatomical basis of the Abbé flap. Laryngoscope. 2001;111(3):382–386. PMID: 11224765.
< div class='tao-gold-member'>