Laser Therapies for Disorders of Hyperpigmentation
Malcolm S. Ke
Teresa Soriano
Laser and light source therapy for disorders of hyperpigmentation in darker skin types are limited by their potential to cause postinflammatory dyspigmentation. Any aggressive therapy resulting in inflammation may induce this unwanted response, hence fulfilling the adage, “the treatment may be worse than the disease.” Perioperative use of topical bleaching agents and sun-protective measures are valuable in optimizing outcomes. Inciting factors, if present, need to be identified and discontinued to prevent further dyspigmentation during and after surgical treatment.
The use of lasers and light sources for hyperpigmentation is generally based on wavelengths targeting melanin or pigment as the chromophore. Although no quantitative differences in melanocytes are seen in various ethnic groups, melanocytes of darker-skinned individuals produce greater quantities of melanin and demonstrate exaggerated responses to cutaneous injury. This translates clinically to an increased susceptibility to irritation and to a greater risk of further pigment alteration in darker-skinned individuals. It is wise to perform a test spot on a representative lesion before treating the entire area.
Nonablative light sources, such as the intense pulsed light system, have been used safely and effectively to treat patients with darker skin. Various Q-switched lasers that deliver pulses in the nanosecond range are commonly used to treat pigmentary disorders. They include the 532-nm Nd:YAG, 694-nm ruby, 755-nm alexandrite, and 1,064 nm Nd:YAG. Given increased melanin absorption at shorter wavelengths, the use of longer wavelength lasers is generally preferred in treating darker-skinned patients. Ablative lasers such as the 2,940-nm Erbium:YAG and 10,600-nm CO2 lasers carry a significant risk of postinflammatory dyspigmentation; therefore, they are reserved for selective resistant cases and should be used with caution. A new modality called fractional photothermolysis may prove to be the happy medium between ablative and nonablative techniques.
Clinical Applications
Melasma
Melasma is an acquired form of hyperpigmentation that is more prevalent in darker-skinned women. It typically manifests as brown to gray patches on the face that worsen with sun exposure. Melasma may occur during pregnancy or oral contraceptive use but commonly arises de novo. Histologically, melanin can be found in the epidermis, dermis, or both.
The treatment of melasma is challenging and is best approached with a combination of treatment and preventative measures. Although the condition may resolve after termination of pregnancy, ceasing oral contraceptive use, or sun avoidance, it commonly persists indefinitely. The use of topical bleaching agents alone in conjunction with sun-protective measures may provide an adequate cosmetic outcome. Both phenolic and nonphenolic depigmenting agents have been shown to improve melasma in darker skin types.1 In evaluating combination treatments, Pathak et al. reported optimal results with the application of 2% hydroquinone, 0.05% to 0.1% retinoic acid, and a broad-spectrum sunscreen for the treatment of melasma in Latinas.2 Various chemical peels have also been used alone or in conjunction with topical bleaching agents in an effort to expedite results, prevent relapse, or treat recalcitrant cases.3,4,5,6,7,8
The use of lasers for the treatment of melasma has yielded suboptimal results. Earlier studies with the 510-nm pigmented lesion dye laser revealed minimal improvement and even darkening of treatment areas.9,10 Results with the Q-switched ruby laser were inconsistent.11,12 Ablative lasers such as the Erbium:YAG and CO2 lasers carry a high risk of dyspigmentation, especially in darker skin types. In a study using the Erbium:YAG laser to treat 10 patients with melasma recalcitrant to bleaching creams and chemical peels, all patients developed postinflammatory hyperpigmentation 3 to 6 weeks postoperatively.13 Combination laser
treatment with a Q-switched alexandrite and CO2 laser in a split face study in six Thai women revealed greater improvement in MASI scores on the combination treated side as opposed to the side treated by the alexandrite laser alone.14 However, two patients developed severe hyperpigmentation, and two patients had transient hypopigmentation.
treatment with a Q-switched alexandrite and CO2 laser in a split face study in six Thai women revealed greater improvement in MASI scores on the combination treated side as opposed to the side treated by the alexandrite laser alone.14 However, two patients developed severe hyperpigmentation, and two patients had transient hypopigmentation.
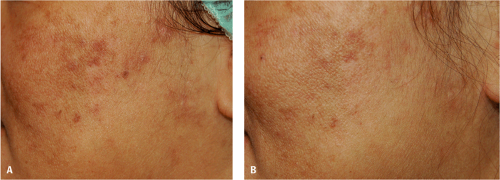
A relatively new nonablative technology, fractional photothermolysis (FP), has shown promise for the treatment of melasma (Fig. 13-1). FP produces a pixilated pattern of multiple columns of thermal damage, referred to as microthermal treatment zones (MTZs), on the skin.15,16 FP can control the pattern density and depth of thermal damage. In this way, different three-dimensional MTZ shapes can be created. This thermal damage extends into the reticular dermis while producing photocoagulation of the epidermis. Importantly, FP does not affect the tissue surrounding MTZs. Thus, the remaining viable cells support a rapid healing time, with re-epithelialization achieved in 1 day. With the extrusion and replacement of damaged tissue, a “fractionalized resurfacing” occurs. The procedure is repeated four to five times at 2- to 4-week intervals. Postprocedure side effects are typically mild and include erythema and edema. Because there is no dermal or epidermal ablation, there is none of the significant recovery time associated with ablative laser therapy.15
Preliminary studies have shown improvement of melasma after a series of fractional resurfacing treatments.17,18 In a study of 10 patients with skin types III through V treated for recalcitrant melasma, 60% had >75% clearing after four to six fractional resurfacing treatments at 1- to 2-week intervals.17 The precise mechanism leading to clinical improvement of melasma is unclear. Increased absorption of the concurrent bleaching agents through the microthermal treatment zones and/or increased elimination of epidermal and dermal pigment are proposed theories. Further investigations are necessary to assess the efficacy and safety of this technology in Fitzpatrick skin types V and VI.
Postinflammatory hyperpigmentation
Postinflammatory hyperpigmentation (PIH) is one of the most common causes of altered skin pigment and presents as dark patches occurring at sites of previous cutaneous inflammation. Although it can manifest in various skin types, it is more frequently seen with greater intensity and persistence in darker skin types, affecting men and women equally.19,20 Essentially any disease with cutaneous inflammation can potentially result in PIH in individuals capable of producing melanin. Common culprits include acne, atopic dermatitis, lichen planus, mechanical trauma, ionizing and nonionizing radiation, heat, contact dermatitis, and photo-induced dermatoses.20,21 In addition, cutaneous laser therapy is a common cause of PIH.22
The management of PIH involves prevention of further pigment deposition and diminishing hyperpigmentation. First and foremost, treatment or removal of the etiologic insult is essential to avert development of new lesions. Protecting the areas from sun exposure is also critical to prevent darkening of existing lesions. In some circumstances, the above measures, along with a tincture of time, result in the resolution of PIH. However, in cases of incomplete or slow resolution, other treatment modalities can be incorporated.
In general, laser therapy for PIH in darker skin types has been disappointing as it carries the risk for further pigment darkening. However, in some instances and for certain conditions, laser treatment has been reported to be useful. Tafazzoli et al. conducted a study evaluating the 694-nm Q-switched ruby laser to treat postsclerotherapy hyperpigmentation in eight patients, noting a 75% to 100% resolution in 58% of the treated areas and 25% improvement in 33% of the treated areas.23
Monotherapy with topical retinoids has been shown to facilitate resolution of PIH. A randomized, double-blind, vehicle-controlled study evaluating tretinoin 0.1% cream versus vehicle alone for 40 weeks to treat facial PIH in black patients demonstrated significant lightening.24
Overall improvement was initially noted after 4 weeks of therapy. Of the tretinoin-treated patients, 12 of 24 (50%) experienced erythema and desquamation; however, none had any further hyperpigmentation or dyspigmentation. In another double-blind, randomized, vehicle-controlled study, Grimes and Callender reported the efficacy of once-daily tazarotene 0.1% cream in the treatment of PIH from acne in patients with Fitzpatrick skin types IV through VI.25 Significant advantage over vehicle was noted at 10 weeks of therapy. Patients noted minimal erythema, burning, and peeling. Additionally, an open-label study of darker-skinned patients with acne showed the utility of adapalene 0.1% gel to reduce PIH.26
Overall improvement was initially noted after 4 weeks of therapy. Of the tretinoin-treated patients, 12 of 24 (50%) experienced erythema and desquamation; however, none had any further hyperpigmentation or dyspigmentation. In another double-blind, randomized, vehicle-controlled study, Grimes and Callender reported the efficacy of once-daily tazarotene 0.1% cream in the treatment of PIH from acne in patients with Fitzpatrick skin types IV through VI.25 Significant advantage over vehicle was noted at 10 weeks of therapy. Patients noted minimal erythema, burning, and peeling. Additionally, an open-label study of darker-skinned patients with acne showed the utility of adapalene 0.1% gel to reduce PIH.26
The concomitant use of various bleaching agents has been shown to improve PIH. Kligman and Willis proposed the combination of tretinoin, hydroquinone, and dexamethasone for the effective treatment of PIH.27 In a small study, the application of 2% hydroquinone and 10% glycolic acid gel twice daily and 0.05% tretinoin cream at night was shown to improve PIH in patients with darker skin types.28 Similarly, Yoshimura et al. described the efficacy of tretinoin combined with hydroquinone and lactic acid in reducing PIH.29
For PIH refractory to topical bleaching agents alone, chemical peels can be a safe and effective option in darker skin types.30 Pretreatment with bleaching agents, such as hydroquinone, should be used to minimize the risk of peel-induced hyperpigmentation. Chemical peels should be started at a lower concentration and titrated up as tolerated and necessary. Superficial chemical peels such as salicylic and glycolic acids, which target the stratum corneum to the papillary dermis, can safely be used to facilitate the resolution of PIH. In a study of five patients with skin types V and VI, pretreatment for 2 weeks with hydroquinone 4% cream followed by a series of five 20% to 30% salicylic acid chemical peels (B-lift) at 2-week intervals resulted in 51% to 75% improvement of PIH in one patient and 75% improvement of PIH in four patients.6 No adverse effects were noted. Burns et al. demonstrated greater and more rapid improvement with the addition of glycolic acid peels to a topical regimen of hydroquinone, glycolic acid gel, and tretinoin.28 In this study, patients with skin types IV through VI received six serial glycolic acid peels along with the topical regimen, noting an additional benefit with minimal adverse effects compared with the patients who were treated with the topical regimen alone.
Medication-induced hyperpigmentation
Some medications—such as amiodarone, minocycline, tricyclic antidepressants, phenothiazine, antimalarials, clofazamine, gold, silver, bismuth, and arsenic—may induce dyspigmentation over sun-exposed areas, varying from blue-gray to red-brown. Chemotherapy-induced hyperpigmentation may appear as a localized eruption, such as the flagellate pigmentation of bleomycin or the flexural hyperpigmentation of topical carmustine, or as generalized hyperpigmentation as with busulfan, cyclophosphamide, or methotrexate.
Removal of the offending agent can lead to the resolution of the pigmentation over time; however, some medication-induced pigmentation may persist for years despite cessation of therapy.
Q-switched lasers can be useful in the treatment of certain medication-related hyperpigmentation. The Q-switched ruby and alexandrite lasers have been reported to be effective in the resolution of the imipramine-induced blue-gray pigmentation without discontinuing the medication.31




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree