CHAPTER 76 Laser resurfacing
Physical evaluation
1. Assess Fitzpatrick skin type (Table 76.1). Skin types I, II, III are acceptable candidates for ablative resurfacing, but extreme caution should be used in skin types IV or V. Higher Fitzpatrick skin types can be safely treated using newer fractionated ablative or nonablative lasers.
3. Dyschromia. Brown lesions present in the superficial dermis will respond whereas deeper dermal lesions will persist. Red dyschromia such as seen with acne rosea can result in copious bleeding during Er:YAG laser treatment.
4. Rhytid location and severity (Table 76.2). Differentiate and document static and dynamic rhytids.
5. Cutaneous disorders such as carcinoma, seborrheic or actinic keratoses, and solar lentigines should be noted.
6. Skin tone, texture, and pore size.
7. Adequate preoperative skin care including sunblocking agents, bleaching agents (hydroquinone), and moisturizing skin care regimen.
Table 76.1 Fitzpatrick skin type classification system
| Fitzpatrick skin type | Description |
|---|---|
| I | Extremely fair skin, always burns, never tans |
| II | Fair skin, always burns, sometimes tans |
| III | Medium skin, sometimes burns, always tans |
| IV | Olive skin, rarely burns, always tans |
| V | Moderately pigmented brown skin, never burns, always tans |
| VI | Markedly pigmented black skin, never burns, always tans |
Table 76.2 Glogau rhytid/photoaging classification scheme
| Glogau scale | Age | Description |
|---|---|---|
| Mild | 28–35 years | Little wrinkles, no keratosis, requires little or no makeup for coverage |
| Moderate | 35–50 years | Early wrinkling, sallow complexion with early actinic keratosis, requires little makeup |
| Advanced | 50–60 years | Persistent wrinkling, discoloration of the skin with telangiectasias and actinic keratosis, always wears makeup |
| Severe | 65–70 years | Severe wrinkling, photoaging, gravitational and dynamic forces affecting skin, actinic keratosis with or without cancer, wears makeup with poor coverage |
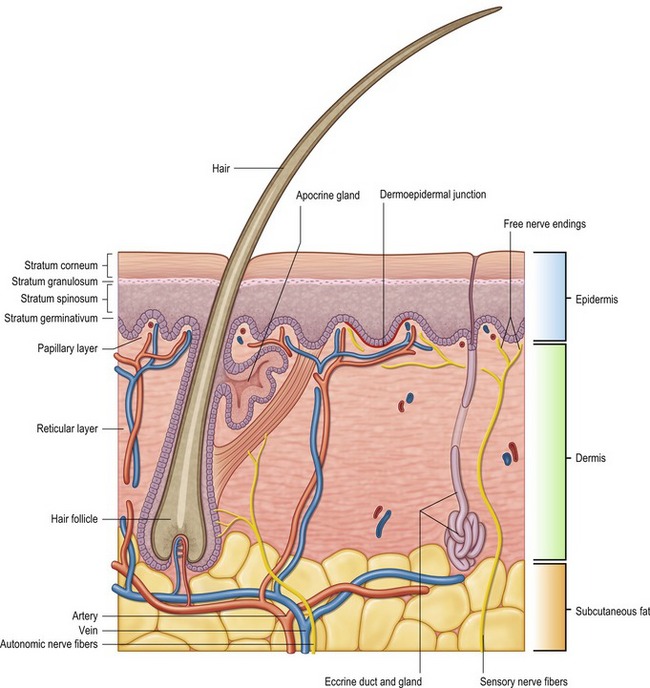
Anatomy
Laser resurfacing demands a precise knowledge of skin histology (Fig. 76.1). The epidermis makes up approximately five percent of skin thickness. The epidermis encompasses five distinct layers: stratum corneum, stratum lucidum, stratum granulosum, stratum spinosum, stratum germinativum. The stratum corneum is composed primarily of nonviable cells, which are turned over frequently and replaced by precursor cells from underlying layers. Nonablative resurfacing techniques by definition leave the epidermis intact, while ablative resurfacing techniques will remove this layer.
The dermis is divided into a papillary and reticular layer. Most ablative resurfacing techniques will remove the papillary and superficial reticular dermis. The papillary dermis begins at the basement membrane and has a high type III collagen content. The papillary dermis is relatively thin measuring about 100 µm in thickness.
Technical steps
Before any laser treatment is undertaken, appropriate safety precautions should be taken by strict application of the guidelines listed in Table 76.3. Wavelength appropriate eyewear should be provided to all operating room personnel and eyeshields should be used for the patient.
Table 76.3 Laser Safety Guidelines