Large-Volume Fat Grafting for the Breast
Wesley N. Sivak
J. Peter Rubin
DEFINITION
Autologous fat grafting has become a common technique for addressing volume and contour deficiencies in plastic surgery.
A survey conducted in 2013 showed that approximately 80% of plastic surgeons have incorporated fat grafting into their clinical breast surgery practice.1
Fat grafting has been utilized for facial rejuvenation, breast augmentation, mitigating radiation damage, capsular contracture, post-traumatic deformities, congenital anomalies, and burn injuries.
Autologous fat grafts have numerous beneficial characteristics including simple surgical procedure, low cost, and nearly universal accessibility.
Although early use was largely as an aesthetic treatment, recent advancements have made fat grafting an attractive alternative for many reconstructive challenges.
Contour abnormalities and volume defects of the breast routinely require large-volume fat grafting, often necessitating several sessions to achieve the desired result.
ANATOMY
Female breasts are composed of glandular tissue that produces milk and adipose tissue; the amount and distribution of fat largely determine the size and shape.
Milk production within the breast occurs within lobules that are organized into 15 to 20 lobes. Milk travels through a network of ducts that coalesce and exit the skin via the nipple.
Adipose tissue, connective tissue, and ligaments provide support and shape to the breast. Nerves passing through these tissues provide sensation. The breast contains abundant blood vessels, lymph vessels, and lymph nodes.
The breast due to its architecture and rich blood supply responds well to fat transfer; the architecture permits expansion of the tissues while ensuring close proximity to blood supply.
Fat grafts are typically harvested from a donor region of abundance (eg, abdomen, flank, or thigh) and serially injected into the deficient recipient site.
Harvested adipose tissue is composed of particles of tissue encompassing adipocytes and stromal vascular fraction cells, which include adipose stem cells (ASCs) or preadipocytes, fibroblasts, vascular endothelial cells, and a variety of immune cells.
Clinical studies have demonstrated safety and favorable fat graft retention rates with strict adherence to basic principles and proper, rigorous technique (ie, Coleman technique).
Stromal vascular fraction cells (and the ASCs within) improve fat graft survival, largely through their angiogenic properties.
PATIENT HISTORY AND PHYSICAL FINDINGS
Patient selection must begin with a detailed history, noting pertinent medical comorbidities that may limit therapeutic potential.
Candidates must be able to withstand the anesthetic requirements of the procedure; it may not be prudent to offer fat grafting to those with significant systemic ailments.
Fat grafting to small areas can be performed under local anesthesia, but large-volume grafting will generally require sedation at a minimum.
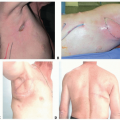
Physical examination entails a thorough assessment of the defect in question in addition to assessment of potential donor sites.
This allows the physician to formulate a plan for correction of the defect in question.
Patients must be informed that several rounds of fat grafting may be needed to achieve the desired results.
For fat grafting to the breasts, significant fat volume is generally required; often, there is a limit as to the correction that can be made given the paucity of fat in some patients.
Asking the patient to gain weight prior to the procedure is feasible only if the patient is willing and able to maintain that weight afterward. This strategy is generally not recommended as weight loss following fat grafting can lead to loss of volume and failure to maintain adequate correction.
IMAGING
For breast fat grafting, screening mammography should be performed preoperatively consistent with current guidelines.
Typically, no radiologic or other diagnostic studies are required; physical examination alone will suffice to formulate an effective grafting strategy.
SURGICAL MANAGEMENT
It is not sufficient to merely graft fat diffusely in the breast. The grafted fat must be placed appropriately to accomplish the desired objectives of shaping the breast.
The surgeon must be familiar with the potential levels of placement (eg, subdermal, subglandular, intramuscular, and supraperiosteal) and the amounts necessary at each level to accomplish a desirable change.
These amounts will vary across regions of the body as well as from patient to patient.
Determining the amounts of fat to place and the levels in which to place the fat in order to create subtle, lasting contour changes requires a sophisticated surgical plan.
The Coleman method of fat grafting remains essentially unchanged since the original inception three decades ago.2
The process relies upon harvesting the fat gently to preserve its architecture, refining the fat with centrifugation to remove nonviable components and provide a predictable volume, and placement of the fat in small aliquots to increase the surface area and ensure a robust blood supply to the grafted tissue.
When these principles are adhered to, fat grafting can be a reproducible and safe procedure.
Histologic studies have shown that this method of harvesting and refinement with centrifugation yields fat with a high percentage of survival and near-normal adipose cellular enzyme activity.3
However, this method of fat processing lacks efficiency for large-volume fat grafting. Therefore, the Coleman technique is used to refine results of large-volume fat grafting (“touchup” procedures), and a simple method of harvesting large volumes of fat with machine-powered suction and decanting the aspirate is described below.
Preoperative Planning
Patients should be marked in the standing position prior to surgery. When in the operating room, significant changes in breast shape can occur with changes in position.
Areas of volume deficiency on the breast should be marked and the volume to be added estimated, keeping in mind that approximately 40% resorption of volume can be expected during healing. The plane of injection will depend on surgical goals. Superior pole fullness can be achieved predominantly with subcutaneous injection, whereas increasing central projection will require deep injection.
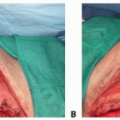
A mastopexy can be performed concurrent with fat grafting, and we recommend a technique with minimal parenchymal dissection to preserve nipple/areolar blood supply after grafting.
Concentric circles should be drawn around adipose depots that are going to be harvested to ensure areas are not overharvested.
Positioning
With the patient in the supine position, both typical donor sites (eg, abdomen, flank, and thigh) and the breasts are easily accessible.
Following fat harvest and processing, grafting can be done with the patient either supine or with the bed flexed into a sitting position with arms abducted.
Sitting position will allow for better assessment and correction of ptosis, clearly delineating the inframammary fold.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree