Fig. 8.1
BMI criteria for Bariatric and Gastrointestinal Metabolic surgery for the Asian Population (From Lakdawala and Bhasker [3])
8.3 Pre-op Evaluation wwand Preparation
Proper preoperative patient education is essential and attendance at educational sessions is mandatory. Poor understanding of the concept of food restriction in AGB can be a potential risk factor for post-op complications. We routinely check chest PA, EKG, CBC, serum biochemistry, urinalysis, coagulation profiles, thyroid function test, HbA1C, and lipid profiles (TG, cholesterol, HDL, and LDL). Cholelithiasis or steatohepatitis are the most prevalent of the several gastrointestinal conditions in morbidly obese patients. Abdominal ultrasound is performed for evaluating the gall bladder and liver for patients showing relevant symptoms or elevated liver enzymes. Gynecologic specialist checks the ovary and uterine diseases if there are menstruation-associated problems. Patients with a history of recent chest pain or a change in exercise tolerance need to undergo a formal cardiology assessment, including stress testing and echocardiogram as indicated. Patients with suggestive histories of clinically significant sleep apnea need to undergo preoperative sleep study testing. If found to have the condition, use of a continuous or bi-level positive airway pressure apparatus postoperatively while sleeping can eliminate the stressful periods of hypoxia. Gastroesophageal reflux disease (GERD) is common in severely obese patients because of the increased abdominal pressure and shortened lower esophageal sphincter. Gastrofibroscope is not routinely performed before LAGB, but we performed that for patients who have not undergone an endoscopy before, have GI symptom such as reflux, have epigastralgia, have antireflux medications, and have familial history of esophagogastric malignancy.
The size of the left lobe of the liver often inhibits the surgeon’s ability to complete LAGB. Patients with a known enlarged fatty liver may benefit from hypocaloric diet tried for several weeks before surgery for shrinkage of the left lobe of the liver. This facilitates the LAGB procedure without complications such as inaccessibility of the cardiac region or liver capsular bleeding. Preoperatively, SC injections of heparin or low-molecular-weight heparin (LMWH) for DVT prophylaxis is not routinely performed except for those who are high-risk thrombophilic patients including superobese patients anticipating longer procedure, those with history of DVT, venous stasis ulcer, and hypoventilation syndrome of obesity. Recent data have shown that pulmonary embolism is uncommon after laparoscopic bariatric surgery and that measures such as early ambulation and sequential compression devices(SCD), without pharmacologic agents, such as heparin, can be used successfully to prevent DVT and PE in many patients undergoing LAGB [4]. We routinely use perioperative SCD and encourage patients’ early ambulation after LAGB. A prophylactic intravenous first-generation cephalosporin, in a dose appropriate for weight, is given preoperatively and, if deemed necessary, intraoperatively (long procedure or contamination). Antibiotics are continued for less than 24 h. Oral antibiotics are prescribed several days as discharge medications with narcotics, antacids, and prokinetics.
8.4 Operation
After induction anesthesia, patients’ prep is very important for safely and easily performing the procedure. Urinary catheterization is seldom necessary except in case of difficult case of revisional surgery or complication surgery in which expected procedure time is longer than 2–3 h. Nasogastric tube is not necessary except in case of significant gastric distension after induction anesthesia. Before skin prep of the patients, we always test the mobility of operation table whether or not the steep reverse Trendelenburg position is possible. For most morbidly obese patients, the huge fatty omentum prevents adequate view of the GE junction. Therefore, reverse Trendelenburg position is important for easily accessing the cardia in these patients. Vertical foot plate fixed in the table is very useful for maintenance of the steep reverse Trendelenburg position in this circumstance. The skin is soaped with skin soap. Skin prep with Betadine ranges from upper limit nipple level to lower limit anterior superior iliac spine level. Laterally, margin of surgical prep is slightly lateral to both anterior axillary lines. Antimicrobial IobanTM incise drape is preferred by some surgeons. We have found a 10 mm/30° telescope, extra-long, atraumatic graspers, and other instruments to be most useful. Extra-long trocars may be needed for superobese patients. An ultrasonic scalpel is helpful in all aspects of the dissection even in AGB procedure. A fixed retractor device secured to the operating room table for clamping and holding the liver retractor is also essential. The surgeon stands to the patient’s right, the assistant is to the patient’s left, and the camera operator is adjacent to the surgeon.
The standard trocar placement for AGB we usually perform is as follows (Fig. 8.2): The first trocar used is 15 mm trocar at or just above the umbilicus. We usually do this with open Hasson techniques. After CO2 insufflation until 15 mmHg and under the direct view from the umbilical trocar, additional four trocars are inserted: two 5 mm trocars at both subcostal areas, one 12 mm trocar at left upper quadrant, and 5 mm epigastric trocars for Nathanson liver retractor. For the superobese (e.g., BMI >60), three abdominal trocars need to be moved slightly cephalad direction for better surgical view of cardiac region. Pneumoperitoneum usually ranged within 12–15 mmHg. In case of superobese patients, adjustment up to 20 mmHg level is often necessary for elevating thick abdominal wall. Communication with the anesthesiologist for adjusting the pressure of air insufflations is very important for preventing CO2 retention or hypoxia induced by excessive pressure from abdominal cavity.
Fig. 8.2
The standard trocar placement for AGB. Dotted arrow indicates the direction of trocar advance
All operations are performed by the author utilizing LAP-BAND® (Allergan, Irvine, CA, USA) with different modifications (9.75/10.0, AP series). However, the AGB procedure may be performed with any of various types of adjustable bands. They all work on the principle of reduction of oral intake by augmenting the early satiety and decrease in appetite triggered by distention of the proximal part of the stomach. The two bands approved for use by the FDA in the United States are the LAP-BAND® (Allergan, Irvine, CA, USA) and the Realize Band (Ethicon Endo-Surgery, Cincinnati, Ohio). The Swedish Adjustable Gastric Band (Obtech Medical, Baar, Switzerland), the MIDBAND (Medical Innovation Development, Villeurbanne, France), and the Heliogast band (Helioscopie, Vienne, France) are other banding systems used in Europe, Asia, the Middle East, and South America. Key points of the techniques of placement of the AGB include (1) very small pouch formation by placement of the band on top of the stomach just below the gastroesophageal junction. A calibration tube with a 25 cc balloon may be used depending on surgeon’s preference for proper band placement and detection of the hiatal defect. (2) The pars flaccida technique, in which entry into the lesser sac is avoided by placement of the band suprabursally around gastric vessels and fat instead of close to the gastric wall. (3) Anterior fixation of the gastric fundus using three to four nonabsorbable sutures between above and below the band.
After adequate liver retraction with Nathanson retractor, access to the gastroesophageal junction becomes much easier. The telescope is placed through the left upper quadrant 12 mm port for this part of the operation to maximally view the angle of His area. Fundus is grasped with babcock forceps and retracted downward to the patient’s right side for stretching that area. With a hook diathermy, peritoneal membranes on the phrenoesophageal fat pad at the angle of His are minimally dissected to create an opening in the peritoneum (Fig. 8.3a). Swabbing with suction device in that area is useful for clearly exposing the His angle and left pillar of the crus muscle (Fig. 8.3b). The pars flaccida technique has become the approach of choice for placing the adjustable band. The filmy membranous gastrohepatic ligament onto the caudate lobe (pars flaccida) is divided for accessing the right pillar of the crus muscle of the diaphragm (Fig. 8.3c). The anterior branch of the vagus nerve and any aberrant left hepatic artery should be preserved at this point of time. Caudate lobe and crus muscle should be seen clearly because occasionally the vena cava can lie close to the caudate lobe. With an ultrasonic device (or hook diathermy), the peritoneal membrane above the right pillar of the crus muscle fascia is minimally dissected and advanced about 1–2 cm toward the patient’s left with a gentle spreading and pushing technique (Fig. 8.3d). With laparoscopic grasper, omentum encasing the perigastric vessels is carefully grasped away to the left of the patient. This facilitates band passer entry into the band tunnel opening. Special tunneling instrument (band passer), which follows the surface of the right crus posterior and inferior to the esophagus while aiming for the angle of His, should be advanced smoothly without any resistance until it can be seen at the other side near the top of the spleen (Fig. 8.3e, f). Resistance often can be felt during advancement of the band passer in case where the retrogastric tunnel is made incorrectly, for example, (1) below the right crus muscle fascia (2) penetrating the left crus fascia (3) entering the bursa omentalis (lesser sac). In these circumstances, the band passer should be withdrawn and it should be advanced with direct vision carefully. Small blood vessels can bleed, but it usually stops spontaneously or is easily controlled with coagulation. The adjustable band is placed through the large 15 mm trocar. With the guidance of the band passer, the band tubing is introduced into the posterior tunnel and pulled through from the greater to the lesser side of the stomach. The band is locked using the atraumatic forceps. A 5-mm grasper inserted between the band and stomach ensures that the band is not too tight. Three or four gastrogastric plications over the band with 2-0 nonabsorbable suture material are performed. The first stitch should be located as far posterolateral on fundus as possible because this region has been the most frequent area of fundus herniation through the band. Suture should not be performed in front of the band buckle. The accurate seromuscular bites are very important because inaccurate gastrogastric sutures can be loosened with time and eventually make the portion of the fundus redundant below the band, which is the culprit of the partial fundal prolapse causing anterolateral band slippage. Removal of the fat pad on the cardia with coagulation greatly facilitates the accurate seromuscular bites (Fig. 8.4). Adequate seromuscular bite and wrap stabilize the gastric band and minimize the complications such as fundal prolapse (slippage) or band erosion (Fig. 8.5). After the intra-abdominal procedure is completed, the tubing is retrieved through one of the trocar sites (usually left upper quadrant). With the laparoscopic grasper inserted through the 15-mm trocar incision site, a subcutaneous tunnel is made, through which the end of the tubing is grasped. The tubing is retrieved through the subcutaneous tunnel, excess tubing is trimmed, and then the port is connected to the tubing. The port is secured onto the anterior rectus fascia by four stitches made with Prolene sutures (Ethicon).
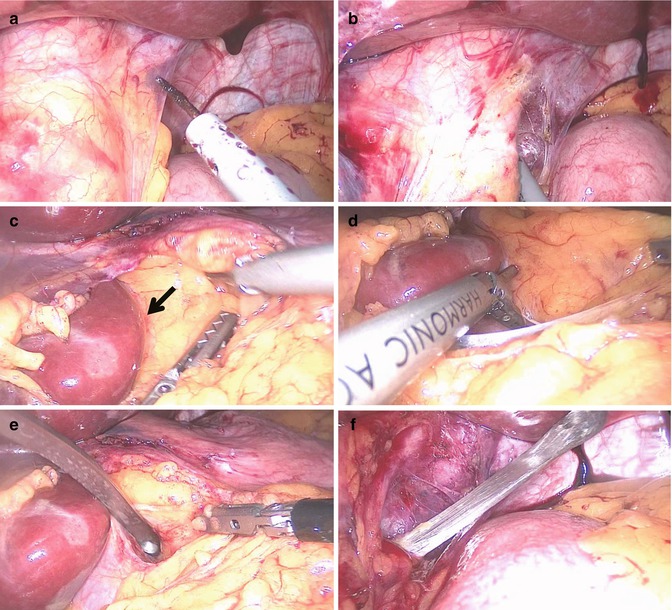




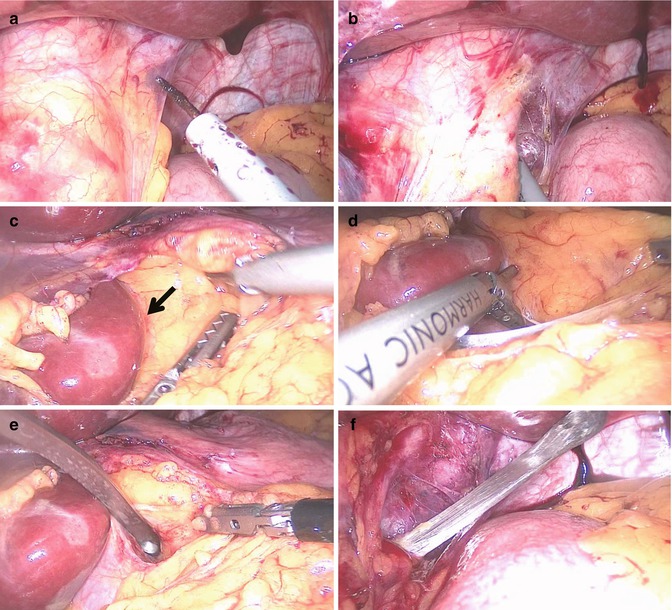
Fig. 8.3
(a) Create an opening in the peritoneum. (b) Expose the His angle and left pillar of the crus muscle. (c) Divide the membranous gastrohepatic ligament. Arrow indicates landmark area for starting retrogastric tunneling (between crus muscle and perigastric fat). (d) Dissect minimally the peritoneal membrane above the right pillar of the crus muscle fascia. (e, f) Insert the Band passer smoothly on the surface of the right crus posterior and inferior to the esophagus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







