Jejunal Free Flap
J. J. COLEMAN III
EDITORIAL COMMENT
The jejunal free flap for esophageal reconstruction is an elegant and attractive technique; however, it is not clear if swallowing or voice restoration with a Blom-Singer valve is any better with this flap than with a tubed flap such as the radial forearm.
The jejunal free flap or jejunal free autograft is a reliable, frequently used method of transferring a segment of bowel to replace an area lined with mucosa. Because of the length of the small bowel, its constant blood supply, and its more favorable bacterial content, the jejunum has been more popular than segments of the colon or stomach. The size of the jejunal branches of the mesenteric vessels allows revascularization at the site of reconstruction with microscope or loupe magnification.
INDICATIONS
Although usually used to reconstruct circumferential defects of the laryngopharynx, this flap is also useful in reconstruction of partial pharyngeal defects, oral cavity, and vagina. The defect created by extirpation of malignancy in the upper aerodigestive tract is characterized by heavy bacterial contamination, possible previous radiotherapy, and complex functional significance. Because late-stage disease requiring such surgery has a high likelihood of early recurrence, single-stage restoration of function and reasonably normal appearance are crucial.
The predominant functions of the upper aerodigestive tract are alimentation and respiration; more specialized actions include swallowing and speech. Although the precise recreation of speech has been elusive, swallowing is facilitated by providing a patent conduit between the oral cavity and the remaining esophagus. Jejunum is of a similar caliber and structure to the cervical esophagus and pharynx and is thus useful for replacement of total laryngopharyngectomy defects from the nasopharynx at the base of the skull to the thoracic inlet, or occasionally to the aortic arch. It is most useful when the larynx has been removed because its copious secretions may result in aspiration with the larynx in place.
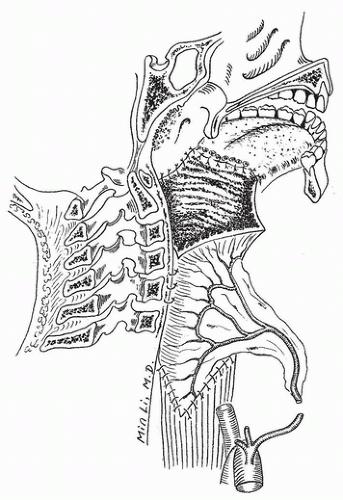
Using the jejunum as a tube-fillet combination, the total or partial glossectomy/laryngectomy defect can be reconstructed with a single segment of bowel (Fig. 226.1). Partial defects of the hypopharynx, oropharynx, and oral cavity are also amenable to reconstruction using a patch of jejunum, again best suited in the absence of the larynx. The length of the mesentery of the jejunum and the need for midline position of the bowel require recipient vessels in the neck. If previous radical neck dissection or vascular disease result in deficient vessels, a flap with a longer pedicle, such as the gastroepiploic flap or the radial forearm flap, may be necessary to reach branches of the axillary artery. The presence of ascites is a contraindication to this procedure.
Although the jejunum is expendable and useful as both a circumferential and patch repair, other methods are also available (1). When the larynx remains intact, the jejunum should not be used unless the segment is at or below the cricopharyngeus. For patch-type defects or when the larynx is intact, the lateral arm, radial forearm, scapula, and lateral thigh flaps all provide epithelial lining to replace pharyngeal mucosa, with minimal to moderate donor-site morbidity. Circumferential
defects can be closed with the larger skin flaps of the radial forearm and scapula.
defects can be closed with the larger skin flaps of the radial forearm and scapula.
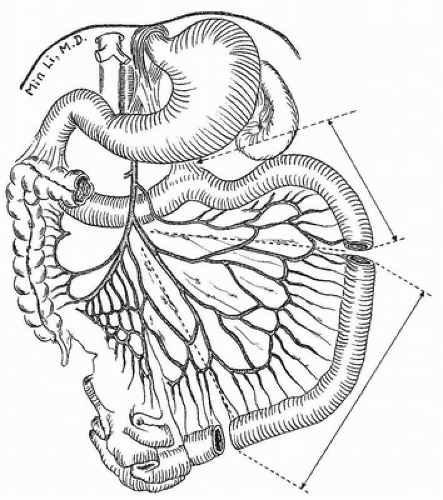
ANATOMY
The jejunum is the second portion of the small intestine, beginning at the ligament of Treitz and extending approximately 8 feet distally. The blood supply includes the jejunal branches of the superior mesenteric artery and vein that pass through the mesentery and arborize to supply the gut. In the proximal mesentery, there is usually only one arcade of vessels distal to the segmental artery and vein, with the vasa recta extending directly off the arcade. This makes the relationship between the branch of the superior mesenteric artery and the segment of gut it supplies more direct than in the ileum, where there are two or three arcades of vessels between the superior mesenteric artery and vein and the vasa recta to the bowel (Fig. 226.2). When harvested, the diameter of the jejunal vessels from the superior mesenteric artery and vein range from 2 to 4 mm.
FLAP DESIGN AND DIMENSIONS
To some degree, the segment of jejunum available on a single pedicle depends on body habitus and the length of the mesentery. The selection of an appropriate branch and its subsequent blood supply can result in lengths of bowel from 10 to 30 cm. The mesentery of the small bowel varies with body habitus but generally ranges in length from 15 to 20 cm.
Selection of appropriate vessels in the neck before harvesting the jejunal free autograft is of paramount importance. The ischemia tolerance of jejunum is low, requiring revascularization in 2 hours or less. Because the ideal location for the bowel conduit is in the midline (the anatomic site of the pharynx and cervical esophagus), and because there is an obligate length of mesentery necessary before anastomosis can be done, vessels situated in the lateral neck are best for recipients.
OPERATIVE TECHNIQUE
The transverse cervical vessels can be found just lateral to the jugular vein deep to the omohyoid in the medial posterior triangle; these are ideal for anastomosis low in the neck. The facial and occipital branches of the external carotid, which lie just beneath the digastric muscle on the lateral neck and external jugular vein, may be dissected out and placed laterally in the superior neck (Fig. 226.3). Anastomosis to the main internal jugular or the proximal medial branches of the external carotid requires bowing of the jejunum off the midline or
folding of the mesentery. The former impairs subsequent transit of food through the conduit, and the latter increases the risk of venous thrombosis. Whatever vessels are chosen should be completely prepared for micosurgical anastomosis before division of the jejunal vessels.
folding of the mesentery. The former impairs subsequent transit of food through the conduit, and the latter increases the risk of venous thrombosis. Whatever vessels are chosen should be completely prepared for micosurgical anastomosis before division of the jejunal vessels.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree