div class=”ChapterContextInformation”>
15. Scalp Itch Treatment
Keywords
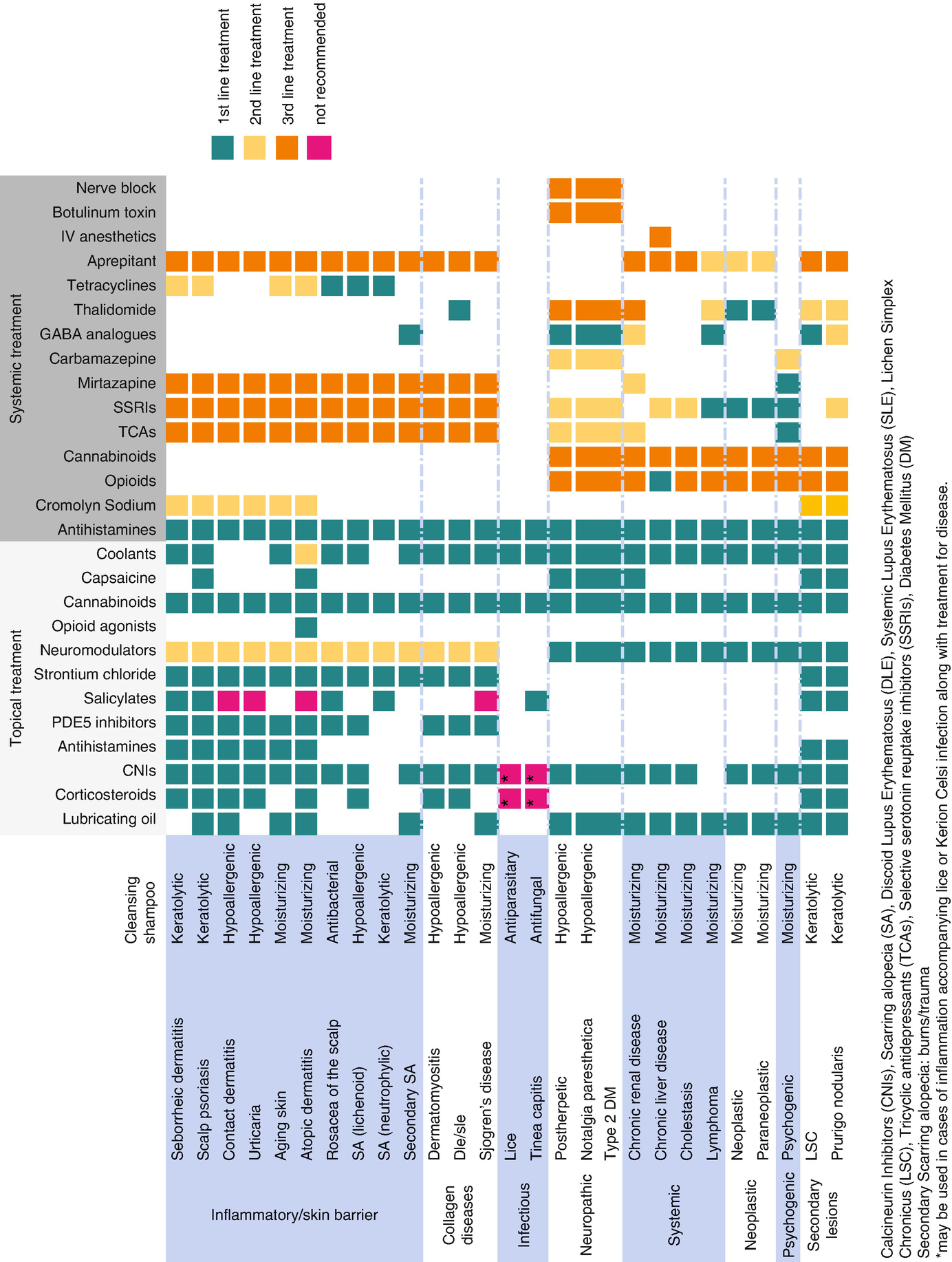
ScalpItchManagementTreatmentPruritusHydroxyzineDoxepineAmitriptylineNortriptylineParoxetineAntidepressantsMirtazapineGabapentinPregabalinOpioidsNaltrexoneNaloxoneCromolyn sodiumThalidomideAprepitantDronabinolCarbamazepineCorticosteroidsCalcineurin inhibitorsAntihistaminesPDE5 inhibitorsSalicylatesStrontium chlorideNeuromodulatorsOpioid agonistsCannabinoidsCapsaicinCoolantsScalp itch is a common cause of complaint in the dermatological setting and also accompanies many of the scalp disorders. The first step to treat scalp pruritus is to find the underlying cause. In order to help attenuate scalp itch, helping skin barrier and microflora balance, general antipruritic management, specific mediator targeting, and specific disease treatment must be combined.
Treatment of scalp pruritus
A thorough evaluation must comprehend a complete history, clinical, and trichoscopical evaluation and sample taking when necessary. It is important to identify if pruritus is localized to a specific area of the scalp, the whole scalp, or the scalp and other body parts. Also, establish if it involves a primary skin lesion or if no primary skin lesion is involved; secondary lesions such as lichen simplex chronicus and prurigo nodularis may accompany both cases.
Inquire about scalp hygiene routine, products that are used every day, recent scalp/hair treatments, scratching behavior, and its burden in quality of life. Distinguish if the sensation is itching, burning, or stinging. Ask the patient about their opinion regarding the origin of their scalp condition, aggravating or relieving factors, and its response to current or previous treatments.
General Management of Scalp Pruritus
Hygiene Recommendations
- (a)
Cleansing
- (i)
Daily scalp cleansing is recommended. Shampoo must be chosen according to the underlying cause for scalp itching. In cases of seborrheic dermatitis, a medicated shampoo with desquamating and/or antifungal properties is preferable. In contact dermatitis or scalp eczema, a hypoallergenic and moisturizing shampoo is the best. In case of scalp psoriasis, a keratolytic and/or steroid containing shampoo is recommended.
- (i)
- (b)
Lubricating
- (i)
Lubricating the scalp is possible in cases where pruritus is associated with scalp xerosis. Moisturizing shampoo, oil-based lotions, or coconut oil may be used as scalp skin emollients.
- (i)
- (c)
Sun protection
- (i)
Sun protection is highly recommended with physical barriers such as caps and hats.
- (i)
- (d)
Avoiding irritating habits/agents
- (i)
Avoiding scratching. Although difficult, explain about the importance of breaking the itch-scratch cycle. Cognitive therapy, cutting of fingernails, and substituting scratching and rubbing with patting and cooling might help modify scratching behavior [2].
- (ii)
Brushing/styling recommendations: Avoid mechanical/chemical trauma such as excessive scalp brushing irritant cosmetical substances and excessive heat.
- (i)
Topical Antipruritic Agents
Topical treatments for the scalp are first-line treatments in cases where cutaneous lesions are present and when itch is localized to the scalp. Formulations require sufficient bioavailability of the active drug after percutaneous absorption. Preferred formulations have gel, foam, or ointment bases.
Topical Corticosteroids
Topical corticosteroids are first-line therapy for scalp itch associated with inflammatory conditions of the scalp. Clobetasol 0.05% foam or ointment is the preferred formulation. Long-term use of ultrapotent steroids may cause side effects such as folliculitis and telangiectasia. Although prolonged application of topical steroids can cause skin atrophy, the author has never seen atrophy on scalp. In children, always consider systemic absorption [3, 4]. Avoid corticosteroids in case of scalp dysesthesia.
Calcineurin Inhibitors
Tacrolimus 0.1% ointment and pimecrolimus 1% cream are immunomodulators that have anti-inflammatory properties, as well as an antipruritic effect by activating and then desensitizing TRVP-1 on peripheral nerve fibers [5]. A thin layer should be applied twice daily and rubbed gently but completely. Consider the possibility of compounding in a topical solution.
Pruritus is reduced within 48 hours of initial application, and it is safe and effective for prolonged use [6]. Side effects include transient burning or stinging sensations, and it should not be used in cases of infection.
Antihistamines
Although well-known contact sensitizers, topical antihistamines are commonly used. Diphenhydramine 2% lotion or gel is useful in acute allergic reactions. Doxepin 5% cream, a tricyclic antidepressant that is a potent H1 and H2 antagonist, has been shown to significantly reduce pruritus in patients with atopic dermatitis, lichen simplex chronicus, and contact dermatitis [7].
Phosphodiesterase 4 Inhibitors
Crisaborole 2%, a petrolatum-based ointment, is a nonsteroidal phosphodiesterase 4 (PDE4) inhibitor. It has shown efficacy in treatment of skin pruritus associated with atopic dermatitis. Ointment is usually difficult to wash off from the scalp, thus making it an option in localized eczema of the scalp [8, 9].
Salicylates
Salicylates are COX 2 inhibitors that have anti-inflammatory and keratolytic properties. They are effective in cases of pruritus caused by scaly dermatoses such as psoriasis or seborrheic dermatitis.
Salicylic acid is the most commonly used salicylate . Compounded or commercial formulations of salicylic acid 2–6% as ointment, lotion, or shampoo can be utilized. In cases of thick scales, a 6% leave-in lotion or a 3% ointment (applied at night and shampooed in the morning) helps in reducing the hyperkeratosis faster. Shampoo can be utilized in association and for maintenance. Patients must be instructed to apply on wet scalp and rinse after 5–10 minutes. It can be used daily or alternated with normal shampoo, depending on the severity of the disease. A combination of 3% salicylic acid and 1% hydrocortisone can also be used [10].
Strontium Chloride
Strontium chloride is a salt that has an antipruritic and antinociceptive effect by binding and activating the calcium sensing receptor (CaSR). It is useful in histamine and IgE-related itch and also in neuropathic and scar-forming itch. It suppresses inflammation through TNF-α and has antipruritic effect through the protease-activated receptor 2 (PAR-2), thus making it a good option in scarring alopecias , such as LPP. It can be found commercially alone in hydrogel 4% formulation or as a combined formulation of 4% strontium chloride plus 1% hydrocortisone and 2% diphenhydramine . Mild irritation might occur as a side effect [11].
Topical Neuromodulators
Topical anesthetics such as pramoxine, polidocanol, lidocaine, and benzocaine may offer temporary relief in scalp itch due to different causes. However, they may have an irritant effect on the skin and cause an itch/burning sensation. Polidocanol is a surfactant with both local anesthetic properties and moisturizing effects. A commercial formulation of polidocanol 3% + urea 5% as shampoo or lotion is a good option in cases of scalp itch.
Pramoxine has an antipruritic effect by stabilizing the membrane of sensory nerves. Pramoxine 1% lotion should be applied twice daily. It can be used as a single agent or in combination with topical steroids or lactic acid.
A compound formulation combining 5–10% ketamine, 5% amitriptyline, and 5% lidocaine can improve itch in a variety of pruritic conditions, including neuropathic pruritus [12].
Opiod agonists: Topical compounded preparation of an opioid receptor antagonist such as 1% naltrexone cream has shown good anti-itching activity. Topical liposomal butorphanol is under study [13].
Cannabinoids
Cannabinoid receptor agonists attenuate histamine-related itch. N-palmitoylethanolamine, a cannabinoid receptor CB2 agonist extracted from palm oil, has been compounded into 0.3% cream and shown to reduce pruritus in patients with atopic dermatitis, lichen simplex chronicus, prurigo nodularis, and uremic pruritus. Because of its commercial formulation in cream vehicle, it may be used in cases of xerotic scalps such as elderly scalp, atopic dermatitis, and Sjögren disease [14].
Capsaicin
Topical capsaicin, the active compound in chilli pepper, is an exogenous vanilloid that desensitizes the nerve endings, thus attenuating response to local stimuli. Repeated application of capsaicin inhibits accumulation of calcitonin gene-related peptide (CGRP) and substance P (SP). Capsaicin is commercially available in concentrations of 0.025–0.1%. A burning sensation is common during the first 2 weeks of application. You can avoid this symptom by applying a topical anesthetic before application of capsaicin at the beginning of treatment. Transdermal 8% capsaicin has been approved for use in postherpetic neuralgia. Other possible applications include scalp psoriasis, atopic dermatitis, notalgia paresthetica, lichen simplex chronicus, prurigo nodularis, and uremic pruritus [12, 15].
Coolants
Menthol, camphor, and calamine are coolant agents; their efficacy in treating itch is controversial. Patients who say to improve when taking cold showers or applying ice might benefit from their use. Another mechanism of action involves the ability of menthol to selectively activate κ-opioid receptors and of camphor to act on both transient receptor potential vanilloid (TRVP) 1 and 3 channels, thus making it a good option for treating scalp itch. Menthol 1–7% cream, camphor 0.45% oil, and calamine 3–7.5% are possible options. Common side effects include skin irritation and sensitization; thus, prolonged use is not advised [12, 16].
Herbal Remedies
Arnica
Arnica is derived from the dried flowers of Arnica montana or other arnica species. The active ingredients helanalin 11α, 13-dihydrohelenalin, chamissonolid, and their ester derivatives reduce inflammation by inhibition of the transcription factor nuclear factor κB (NF-κB) and also act as a COX2 antagonist.
When used as an infusion, 2 g of dried arnica is mixed with 100 mL of water. Hair lotions, oils, and shampoos containing arnica are available commercially. The maximum concentration of arnica oil recommended in topical formulations is 15%.
Side effects include allergic and irritant contact dermatitis which could potentially aggravate scalp itch.
German Chamomile
German chamomile has an anti-inflammatory, antimicrobial, and wound-healing action. The active ingredients are sesquiterpene alcohol, α-bisabolol, chamazulene, and flavonoids. These ingredients have anti-inflammatory action as cyclooxygenase and lipoxygenase inhibitors. Flavonoids also inhibit histamine release.
A tea is made by using 2–3 teaspoons (tsp; 10–15 mL) of dried flowers per cup of water and may be applied to the scalp with a compress. Hair lotions, oils, and creams are also widely available.
Tea Tree Oil
The major component of tea tree is terpinen-4-ol. It has an anti-inflammatory effect by reducing the production of tumor necrosis factor, interleukin-1 (IL-1), IL-8, IL-10, and prostaglandin and has activity against Malassezia furfur and demodex. Five percent tea tree oil shampoo is effective for the treatment of mild to moderate seborrheic dermatitis and potentially effective in scalp rosacea; however, it is a well-known allergen [17].
Black Licorice
Glycyrrhetinic acid is an ingredient of black licorice with mineralocorticoid properties. It is a potent inhibitor of 11-B-hydroxysteroid hydroxygenase and also has broad-spectrum antimicrobial and anti-inflammatory activity. Commercial shampoo containing this ingredient improved itching in patients with seborrheic dermatitis [18].
Other Herbal Therapies
Virgin coconut oil demonstrated decrease in pruritus in patients with atopic dermatitis. The mixture of honey, beeswax, and olive oil has proved safe and efficacious in pediatric patients. Herbal Chinese medicine with external wash containing Rhizoma polygonati (4.0 g), Flos lonicerae (2.0 g), Radix glycyrrhizae (2.0 g), and Herba menthae (2.0 g) applied twice daily proved efficacy in controlled trials. An increased efficacy was seen when combined with oral Chinese herbal medicine and flying needle therapy.
Korean herbal decoction of Sophora flavescens, Phellodendron amurense, Schizonepeta tenuifolia Briquet, Liriope platyphylla, and Perilla frutescens var. acuta for 15 minutes once or twice daily has also shown an anti-inflammatory and antipruritic effect in patients with atopic dermatitis, and no secondary effects were noted. BSAM, containing carnosic acid, apigenin, epigallocatechin-3-gallate, glycyrrhetinic acid, resveratrol, baicalin, and asiaticoside showed anti-inflammatory activity, with decrease in pruritus in patients with atopic dermatitis [17].
Systemic Antipruritic Agents
Doses for systemic treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







