Intermediate and definitive cleft rhinoplasties are a challenging part of definitive cleft care. The anatomy of the cleft nose is severely affected by the structural deficits associated with congenital orofacial clefting. A comprehensive understanding of the related anatomy is crucial for understanding how to improve the appearance and function in patients with secondary cleft nasal deformities. Timing of intermediate and definitive rhinoplasty should be carefully considered. A thorough understanding of advanced rhinoplasty techniques is an important part of providing adequate care for patients with these deformities.
Key points
- •
Understanding of the anatomy of a cleft nose deformity is crucial for definitive treatment of this clinical problem.
- •
Timing of intermediate and definitive cleft rhinoplasty.
- •
Preoperative evaluation of aesthetic and functional deficits.
- •
Goals of the secondary rhinoplasty include relief of nasal obstruction, creation of symmetry and definition of the nasal base and tip, and management of nasal scarring and webbing.
- •
Rhinoplasty techniques.
Video content accompanies this article at http://www.facialplastic.theclinics.com .
Introduction
The cleft nasal deformity associated with cleft lip is a complex deformity. The nose is often the most noticeable aspect of the patient’s face once the congenital cleft lip is repaired. This deformity can also cause functional nasal obstruction, which affects the patient throughout his or her development. The cleft nasal deformity involves all tissue layers of the nose including the bony platform, the inner lining, the cartilaginous infrastructure, and the external skin. The degree of the associated deformity is dependent upon the degree of the original lip abnormality. The cleft nasal deformity is also affected by scarring from previous surgeries on the lip and nose and changes resulting from patient growth. The ultimate goal of intermediate and definitive cleft rhinoplasty is to minimize functional problems and to maximize the appearance of the nose.
Introduction
The cleft nasal deformity associated with cleft lip is a complex deformity. The nose is often the most noticeable aspect of the patient’s face once the congenital cleft lip is repaired. This deformity can also cause functional nasal obstruction, which affects the patient throughout his or her development. The cleft nasal deformity involves all tissue layers of the nose including the bony platform, the inner lining, the cartilaginous infrastructure, and the external skin. The degree of the associated deformity is dependent upon the degree of the original lip abnormality. The cleft nasal deformity is also affected by scarring from previous surgeries on the lip and nose and changes resulting from patient growth. The ultimate goal of intermediate and definitive cleft rhinoplasty is to minimize functional problems and to maximize the appearance of the nose.
Development of the cleft nasal deformity
Within normal development, the paired median nasal processes fuse to form the premaxilla, philtrum, columella, and nasal tip. The bilateral maxillary processes form the lateral aspects of the upper lip. If the median nasal process fails to fuse with the maxillary process, a cleft lip deformity results. The extent of the cleft lip deformity also determines the extent of the cleft nasal deformity, which falls along a spectrum.
Anatomy of the Unilateral Cleft Lip Nasal Deformity
When a complete, unilateral cleft lip occurs, the maxilla on the cleft side is deficient, which does not allow the alar base on the cleft side to fuse in the midline. The alar base on the cleft side is, therefore, positioned more posterior, lateral, and inferior than the alar base on the noncleft side. The cleft nasal septum has attachments to the maxilla on the noncleft side, which cause a caudal septal deviation to the noncleft side, while the posterior septum bows toward the cleft side. The lower lateral cartilage (LLC) on the cleft side has a lengthened lateral crus and shortened medial crus. The weakened and malpositioned cleft-side LLC produces a nostril that is wide and horizontally oriented. This change in position of the lower lateral cartilage also affects the attachment to the upper lateral cartilage, which weakens the scroll region and therefore causes a compromise of the internal nasal valve. The middle third of the nose in the unilateral cleft lip nasal deformity is also characterized by weakness of the upper lateral cartilage and malposition of these cartilages. Again, this weakness results from inadequate skeletal support and often results in a concave upper lateral cartilage, which affects the internal nasal valve on the cleft side. The nasal floor is often absent ( Box 1 , Fig. 1 ).
Nasal tip
Medial crus of lower lateral cartilage shorter on cleft side
Lateral crus of lower lateral cartilage longer on cleft side (total length of lower lateral cartilage is same)
Lateral crus of lower lateral cartilage may be caudally displaced and may produce hooding of alar rim
Alar dome on cleft side is flat and displaced laterally
Columella
Short on cleft side
Base directed to noncleft side (secondary to contraction of orbicularis oris muscle)
Nostril
Horizontal orientation on cleft side
Alar base
Displaced laterally, posteriorly, and inferiorly
Nasal floor
Usually absent
Nasal septum
Caudal deflection to the noncleft side and posterior deviation to the cleft side

Anatomy of the Bilateral Cleft Lip Nasal Deformity
When a complete bilateral cleft lip occurs, the maxilla is deficient on both sides. The prolabium is therefore allowed unopposed anterior growth. Both alar bases are located in a more posterior, lateral, and inferior position than in a noncleft nose. The columella is shortened. There is no alteration in the anterior septum. The lateral crura of both lower lateral cartilages are lengthened, and the bilateral medial crura are shortened and splayed. The extent of columellar shortening is related to the size, shape, and position of the prolabium. The entire nasal tip is underprojected, broad, and flattened ( Box 2 , Fig. 2 ).
Nasal tip
Medial crura of LLC short bilaterally
Lateral crura of LLC long bilaterally
Lateral crura displaced caudally
Alar domes poorly defined and widely separated, producing an amorphous tip
Columella
Short
Base is wide
Nostril
Horizontal orientation bilaterally
Alar base
Displaced laterally, posteriorly, and inferiorly
Nasal floor
Usually absent bilaterally
Nasal septum
In a complete bilateral cleft lip and palate, the septum is midline; however, if cleft on 1 side is incomplete, the septum deviates toward the less affected side

Timing of cleft rhinoplasty
There is controversy regarding primary cleft rhinoplasty and its ultimate effects. However, regardless of early intervention, definitive rhinoplasty is usually necessary. Definitive rhinoplasty is typically delayed until the patient has completed facial growth. In female patients, secondary rhinoplasty is generally performed around 15 to 17 years of age, and in male patients at approximately 16 to 18 years of age.
Intermediate Rhinoplasty
Intermediate rhinoplasty is defined as any nasal surgery performed between the time of initial cleft lip repair and the time at which the patient reaches facial skeletal maturity. These procedures are becoming less frequent as primary rhinoplasty becomes more common. Intermediate rhinoplasty procedures are aimed at correcting severe functional abnormalities and minimizing the social stigmata associated with a more noticeable nasal deformity.
Definitive Rhinoplasty
Definitive septorhinoplasty can be performed once the patient has reached facial skeletal maturity. Structural reconstruction of the cleft nose often requires cartilage grafting material from the rib, ear, or septum to achieve adequate support. The goals of the secondary rhinoplasty are the creation of symmetry and definition of the nasal base and tip, relief of nasal obstruction, and management of nasal scarring and webbing.
Preoperative evaluation of the cleft nasal deformity
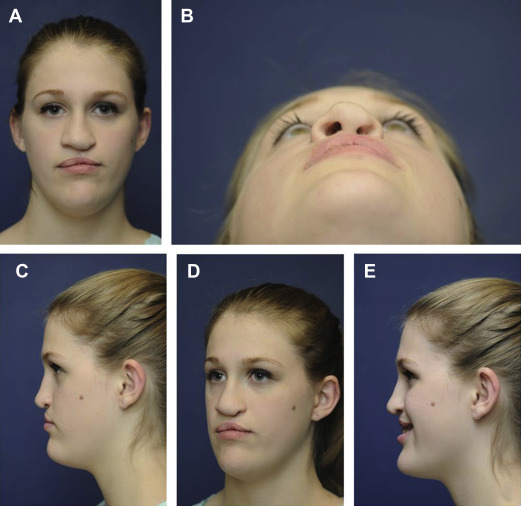
It is important to clearly identify the key factors contributing to the nasal deformity in order to select the most appropriate surgical plan. Functional deficits can be assessed through a thorough history involving nasal symptoms. A physical examination, including anterior rhinoscopy, a Cottle maneuver, a modified Cottle maneuver, and possibly an endoscopic examination is imperative to fully assess the functional deficits of the patient. A full set of preoperative photographs should be taken prior to any planned rhinoplasty procedure ( Fig. 3 , [CR] ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






