Gradea
Type of injury
Description of injury
ICD-9
AIS-90
I
Contusion
Microscopic or gross hematuria, urologic studies normal
866.01
2
Hematoma
Subcapsular, nonexpanding without parenchymal laceration
866.11
2
II
Hematoma
Nonexpanding perirenal hematoma confirmed to renal retroperitoneum
866.01
2
866.11
Laceration
<1.0 cm parenchymal depth of renal cortex without urinary extravasation
866.02
2
866.12
III
Laceration
<1.0 cm parenchymal depth of renal cortex without collecting system rupture or urinary extravasation
866.02
3
Laceration
Parenchymal laceration extending through renal cortex, medulla, and collecting system
866.12
4
IV
Vascular
Main renal artery or vein injury with contained hemorrhage
4
V
Laceration
Completely shattered kidney
866.03
5
Vascular
Avulsion of renal hilum which devascularizes kidney
866.13
5
Table 50.2
Ureter injury scale
Gradea | Type of injury | Description of injury | ICD-9 | AIS-90 |
|---|---|---|---|---|
I | Hematoma | Contusion or hematoma without devascularization | 867.2/867.3 | 2 |
II | Laceration | <50 % transection | 867.2/867.3 | 2 |
III | Laceration | ≥ 50 % transection | 867.2/867.3 | 3 |
IV | Laceration | Complete transection with < 2 cm devascularization | 867.2/867.3 | 3 |
V | Laceration | Avulsion with > 2 cm of devascularization | 867.2/867.3 | 3 |
Table 50.3
Bladder injury scale
Gradea | Injury type | Description of injury | ICD-9 | AIS-90 |
|---|---|---|---|---|
I | Hematoma | Contusion, intramural hematoma | 867.0/867.1 | 2 |
Laceration | Partial thickness | 3 | ||
II | Laceration | Extraperitoneal bladder wall laceration <2 cm | 867.0/867.1 | 4 |
III | Laceration | Extraperitoneal (≥2 cm) or intraperitoneal (<2 cm) bladder wall laceration | 867.0/867.1 | 4 |
IV | Laceration | Intraperitoneal bladder wall laceration ≥2 cm | 867.0/867.1 | 4 |
V | Laceration | Intraperitoneal or extraperitoneal bladder wall laceration extending into the bladder neck or ureteral orifice (trigone) | 867.0/867.1 | 4 |
Table 50.4
Urethra injury scale
Gradea | Injury type | Description of injury | ICD-9 | AIS-90 |
|---|---|---|---|---|
I | Contusion | Blood at urethral meatus; retrography normal | 867.0/867.1 | 2 |
II | Stretch injury | Elongation of urethra without extravasation on urethrography | 867.0/867.1 | 2 |
III | Partial disruption | Extravasation of urethrography contrast at injury site with visualization in the bladder | 867.0/867.1 | 2 |
IV | Complete disruption | Extravasation of urethrography contrast at injury site without visualization in the bladder; <2 cm of urethra separation | 867.0/867.1 | 3 |
V | Complete disruption | Complete transaction with ≥2 cm urethral separation or extension into the prostate or vagina | 867.0/867.1 | 4 |
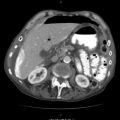
When a urologic injury is suspected in the context of penetrating trauma to the flank, abdomen, or low chest, imaging of the upper urinary system is crucial for diagnosis. CT scan with IV contrast and delayed films at 10 min is the imaging modality of choice for hemodynamically stable patients. CT imaging should permit accurate injury staging based on the AAST criteria, which are highly predictive for operative management. Medial hematoma, with or without extravasation, on early films suggests renal vascular injury while that on delayed films is usually indicative of renal pelvic injury or proximal ureteral injury. Any part of the renal parenchyma that fails to show contrast on early-phase images suggests arterial injury.
CT cystogram should be included in initial imaging when bladder injury is suspected as a result of penetrating trauma to the lower abdomen or pelvis. Indications include: gross hematuria in the setting of blunt trauma, blunt trauma with any degree of hematuria and a pelvic ring fracture, and penetrating trauma to the pelvis with hematuria. The sensitivity and specificity of CT cystogram for bladder rupture are 95 and 100 %, but should CT cystogram not show evidence of bladder injury despite clinical suspicion, retrograde cystography with full bladder distension should be performed and post-drainage images obtained. Retrograde cystography should be performed only in the absence of urethral injury.
When CT imaging is bypassed in the hemodynamically unstable patient who proceeds immediately to surgery, an on-table one-shot intravenous pyelogram (IVP) should be performed by giving a 2 mg/kg IV contrast bolus followed by flat plate x-ray 10 min later. The main purpose of the IVP is to demonstrate two functioning kidneys and an intact drainage system. The presence of an injured solitary kidney should prompt aggressive measures to spare nephrectomy that would commit the patient to a lifetime of dialysis or future transplantation.
Angiography with selective embolization is a more recent modality to attempt nonoperative management. Indications for embolization include: active hemorrhage, pseudoaneurysm, and vascular fistulas. Higher AAST grade renal injuries are associated with increased failure rates with attempts at embolization, and embolization is three times more likely to fail in penetrating trauma compared to blunt trauma. Additionally, failed embolization often ends in nephrectomy.
50.1 Indications for Operative Management
Due to improvements in computed tomography imaging and resuscitation methods, operative intervention for renal injuries has been significantly reduced. Currently 36 % of penetrating and less than 5 % of blunt kidney injuries require operative intervention In addition, about 30 % of penetrating and 45 % of blunt grade IV and V injuries are managed nonoperatively. With the broadening criteria for nonoperative management of renal injury, even in penetrating trauma including some gunshots, the only absolute indications for operative management are hemodynamic instability, expanding or pulsatile perirenal hematoma, incomplete renal injury staging, renal pelvic injury, or non-visualization of the injured kidney on IVP. AAST stage I–III renal injuries are usually hemodynamically stable and are managed nonoperatively. Isolated stage IV renal injuries may be managed nonoperatively when hemodynamically stable but must be continually reassessed and re-imaged by CT scan at 48 h or sooner if there is clinical decompensation. Superselective embolization may be attempted for certain patients with stage IV renal injuries who fail conservative management due to persistent bleeding from segmental arteries. Stage V renal injuries nearly always require operative intervention. With these guidelines in mind however, renal injuries suffered from penetrating trauma are almost always associated with other injuries that dictate the decision to operate.
Almost all ureteral injuries require immediate operative repair. In the event a ureteral injury is initially unrecognized and consequently not repaired immediately, reconstruction should be deferred for 3–6 months to allow inflammation to resolve. All bladder neck and intraperitoneal bladder injuries mandate repair, while most extraperitoneal bladder injuries can be observed unless the patient undergoes laparotomy for other injuries.
50.2 Operative Technique
Once committed to operative management, a standard transabdominal midline incision is best for assessing renal injury because both kidneys can be inspected through this approach and midline incision allows access to the remainder of the abdominal cavity. Abdominal packing, in typical trauma laparotomy fashion, will help control bleeding. Attention should first be turned to the destabilizing injury, urologic or otherwise.
50.3 Vascular Control
When the time comes to assess the bleeding kidney, vascular exposure is the first priority. Lift the transverse colon to the chest with a moist laparotomy pad and move the small bowel to the right in order to expose the retroperitoneum. Carefully incise the retroperitoneum over the aorta at the inferior mesenteric artery and extend superiorly to the ligament of Treitz (Fig. 50.1). The left renal vein can be identified where it crosses the aorta anteriorly, noting that the vein rarely crosses posteriorly and when it does it may be duplicated. Sometimes a large retroperitoneal hematoma distorts the anatomy. In this case, make the incision just medial to the inferior mesenteric vein and proceed to identify the left renal vein. Wrap a vessel loop around the vein without occluding it, unless bleeding from this vessel is heavy. The remaining renal vessels should be identified in order: left renal artery, right renal vein, and right renal artery. The left and right renal arteries are posterior and superior to the left renal vein on either side of the aorta. Apply vessel loops to the renal arteries and veins, but only occlude the vessels if severe bleeding must be controlled (Fig. 50.2).