CHAPTER 23 Injectable Agents for Dermal Soft-Tissue Augmentation of the Face: Options and Decision Making
Facial aesthetic enhancement to restore youth, beauty, and vitality has seen a rapid increase in popularity over the past few decades. The higher level of understanding of the components of facial aging has led us to the appreciation that volume restoration is integral to rejuvenation as surgical repositioning (the ‘lift’). Significant advances and refined techniques have allowed minimally invasive procedures and solutions to volume loss to flourish. Patients can now have these procedures performed in the comfort of a consulting room setting and a swift return to normal activity. Of these, dermal soft-tissue augmentation is unarguably one of the most popular due to its convenience and pleasing results. In addition to smoothing facial rhytids, injectable filling agents are often used in combination to improve the appearance of the periorbita, mid- and lower face, restoring a more youthful appearance with little inconvenience and few complications. In this chapter, we will discuss many of the currently available filling agents, their unique characteristics, and specific procedures most often requested.
Fillers: restoring the aging face
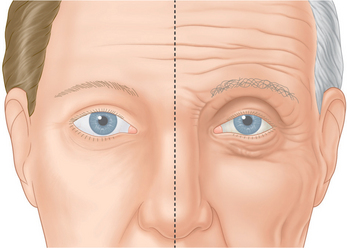
The aging face undergoes many alterations (Fig. 23-1), including changes to skin texture and color, wrinkles and furrows (due to overactive muscles and loss of elasticity), and sagging (in part, due to loss of underlying fat – see Chapter 2, and accompanying DVD clip). There are a number of options for the experienced clinician when choosing a filler for volume replacement, facial contouring, or simply to correct wrinkles and subtly restore the face to a more youthful appearance.
Injectable soft tissue options available
Collagen
Non-permanent biodegradable fillers:
Widely available and easy to use, bovine ‘collagen’ represents an excellent affordable option for temporary augmentation and is indicated for the correction of facial rhytids and scars, as well as lip augmentation. Although these agents are typically included in the long list of soft tissue fillers used for volume augmentation, their role (with the exception of lip augmentation) is primarily for line reduction/eradication. Zyderm and Zyplast (Allergan Inc, Irvine, CA). These agents were the first widely used commercially available products,1 whose names have become synonymous with the word ‘collagen’ despite the fact that there have been dozens of collagen-based injectable products commercially available worldwide since their introduction. These are composed of purified fragments of heterologous animal collagen fibrils derived from processed bovine skin, in a suspension of phosphate-buffered physiologic saline with 0.3 percent lidocaine. Supplied in prefilled syringes and stored at a temperature of 4°C, the dispersed collagen fibrils remain small and fluid. When implanted, the product rises in temperature, forming a more cohesive gel. Zyderm 1 was approved by the Food and Drug Administration (FDA) in 1981, contains a collagen concentration of 35 mg/ml, and is rapidly reabsorbed. Zyderm 2, approved in 1983, contains 65 mg/ml of collagen; reabsorption is consequently slower than with Zyderm 1. Zyplast, approved in 1985, is similar to Zyderm 1 and 2 but the fragmented collagen fibrils are chemically modified and stabilized via crosslinkage with glutaraldehyde. Zyplast is the most viscous of the three products, lasts longer than Zyderm, and although is theoretically less immunogenic than its predecessors has shown a similar rate of allergic reactions.
While early reports of bovine collagen were enthusiastic, claiming a duration of effect as long as 8–12 months, our experience has shown otherwise. Typically, bovine collagen requires two initial treatment sessions to produce the desired effect, which persists from 2–6 months, after which time maintenance treatments are required at least every 6 months or at times more often (Fig. 23-2). Single treatment sessions have been reported in some to last less than 6 weeks despite adequate technique. Good results with bovine collagen (as with all of the injectable filling agents) demand the injection of sufficient volume of product in the appropriate tissue plane; an overly conservative approach (injecting too little) will produce suboptimal effects of short duration. In addition, using sufficient volume ensures simpler maintenance, and less correction at follow-up. Deeper placement (i.e. sub- or deep dermal) produces more transient and less satisfactory effects as resorption with most dermal filling agents appears to be expedited when closer to the subcutaneous space. It has been suggested that the aesthetic improvement of facial lines rests more in the low-grade inflammation afforded by the heterologous (bovine) collagen2 rather than as a direct result of true augmentation of the dermis, but there is also a concern that may relate to potential complications arising from their use.
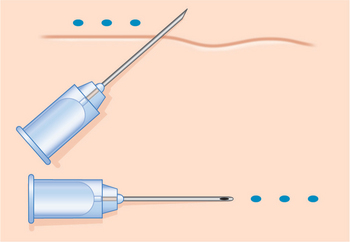
Injection technique is highly variable, but the preferred method is generally regionally dependent. The serial puncture technique is most commonly prescribed (Fig. 23-3) for use of CosmoDerm (for fine lines) and CosmoPlast (for deeper wrinkles and folds) (Allergan Inc, Irvine, CA). These are new bioengineered human collagen-replacement products approved for cosmetic use in Canada and the United States that contain human collagen purified from dermal tissue grown in the laboratory.3 These particular products are processed identically to their bovine counterparts (Zyderm/Zyplast). Although their use has been relatively limited, no allergic responses were observed in a study of 428 patients,4 and a great advantage is that a skin test is not required prior to treatment. Anecdotal reports with experienced injectors however, suggest that the persistence of these agents in some individuals might actually be even less than for bovine collagen. It is suggested that there is less antigenic stimulation, which may reduce the inflammatory effect and subsequent edema required to further reduce the appearance of rhytids.2 One advantage of all of these ‘collagen’ products is that the agents can mostly be delivered without the need for local anesthetic (already contained in each of the product mixtures) and minimal edema and bruising that allows for quicker return to normal activity and appearance.
Techniques for these agents are identical as those for Zyderm/Zyplast (Fig. 23-3).
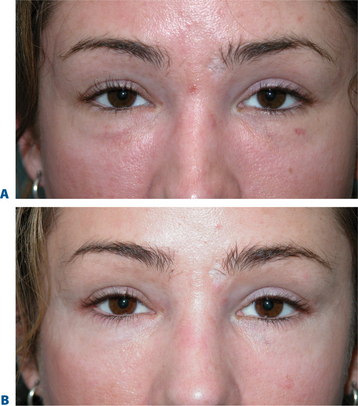
The ‘collagens’ enjoyed the majority market-share of agents for injectable soft tissue augmentation for many years, primarily due to lack of availability of other agents and ease of administration. Additionally, they were available at a time when there was a lesser appreciation of the value of injectable soft tissue augmentation. Most patients expected that they would receive treatment and have positive effects that would last for a predictable, albeit abbreviated, time period (Figs 23-4 & 23-5). The standards had been set, and most individuals expected aesthetic improvement of the order of magnitude of several months at best. Other more labor-intensive agents introduced in the early 1990s were met with some resistance when they required multiple injection sessions to achieve optimal correction (Silicon, Fat, Dermalogen). Despite the introduction of new injectable filling agents with improved characteristics, these agents are still used by many for a host of reasons including lack of better options for particular applications (including the treatment of fine rhytids) and cost.
Complications
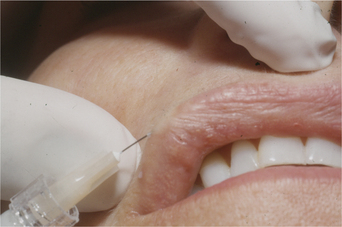
The transient nature of its clinical effect and the need for repeated treatments are injectable collagen’s main drawbacks. In addition, at least 3–5 percent of patients will experience an allergic reaction to bovine collagen5 (Fig. 23-6), necessitating double skin testing prior to treatment. Allergic responses, although rare, can also occur despite negative double skin testing and can be severe and/or long-lasting (Fig. 23-7). Adverse re-actions to bovine collagen injection in the lips are less common and transient. Redness at the injection site nearly always disappears within hours, and bruising will usually resolve within 3–7 days. The patient’s greatest dissatisfaction with ‘collagen’ relates mostly to its rapid resorption. The residence time, however, seems to be correlated with the depth of placement into the dermis, and superficial nodules (as a result of a bolus of products in the superficial dermis) or visible whitish particulate can last for months and even years. These are commonly seen in individuals who have received collagen on multiple occasions for the treatment of superficial rhytids. Another common finding in individuals who had received bovine collagen products to the lips (particularly the vermilion border) on multiple occasions is a progressive difficulty in finding the ‘vermilion plane’ that can usually (in the naïve patient) be easily found (and injected) by placing the needle in the subdermal plane parallel to the lip margin. In many patients, injection of product at the lateral lip margin with this technique can ‘roll’ the material sometimes clear across the midline to the contralateral side. It has been postulated, as well, that the obliteration of this plane is related to chronic inflammation and eventual scarring.2

Figure 23-6 An acute ulcerative reaction to Zyplast. This eventually resolved spontaneously by about 6 months.
Other ‘collagen’ products
Dermalogen
With all of the reported and anecdotal concerns relating to injectable bovine collagen, ophthalmologic pioneer, Charles D. Kelman, MD and collaborator biochemist Dale P. DeVore, Ph.D. began exploring the options and possibilities of using autologous human collagen as an injectable agent for facial soft tissue augmentation. This could potentially address the problems relating to allergy and inflammation, avoid a skin test prior to treatment, and hopefully would yield greater performance compared with the heterologous options. The concept essentially evolved into a process whereby patients undergoing cosmetic surgery (where skin was to be removed) would have their typically discarded skin ‘excess’ saved and transported via express overnight carrier to a central processing facility (Autogenesis Technologies, Acton, MA) where the collagen/dermal matrix could be extracted from the skin. The proprietary process from procurement to the final product delivered intact collagen fibers along with other constituents of the normal dermal matrix in an injectable form called Autologen.6–9 The approximate 3–5 percent sterile dispersion of dermal matrix was sent back to the injecting physician in 1 ml syringes that could be used at a defined period after receipt for the correction of dermal contour defects (Fig. 23-8). The process was a bit laborious and costly; however with appropriate injection technique persistence of wrinkle correction rivaled the bovine collagen experiences that essentially ‘owned’ the filler market at that time. The initial resistance to its use related to the limited applicability for only those individuals undergoing cosmetic procedures where skin was to be removed; at times poor yield and consistency (concentration) of the injectable product; requisite of more than one injection session for full correction in many; and the need for local anesthetic to improve patient comfort as the product contained no local anesthetic within. Shortly thereafter other human tissue products (such as Alloderm) were becoming accepted as care standards in other areas of cosmetic and reconstructive plastic surgery with a much reduced concern of the possibility of communicating disease with such products from a human donor source. There was also an improved understanding of rigorous donor tissue testing, cleansing, and sterilization/decontamination performed to insure safety. The idea of creating an allogeneic variety of human tissue collagen matrix was born whereby skin was obtained from approved tissue banks (like all other donor organs) that were certified by the American Association of Tissue Banks (AATB) and injectable human tissue collagen matrix could be created on a larger and more economical commercialized scale. Dermalogen (allogeneic human dermal matrix) was a result of this concept.2,8–10 The biologic behavior was identical to Autologen, but was far less costly and readily available, also without the requirement of skin testing (Figs 23-9 & 23-11).
The cost and time delay of procurement and custom processing, although ideal, could thereby be eliminated. Factors contributing to the resistance to its use also related to (as with Autologen) the need to use local anesthetic for comfort, as clinicians had only the bovine collagen experience (containing Xylocaine 0.3%). The product became unavailable after a few years of steady sales and satisfactory results by experienced injectors as a result of the demise of the parent company; however it will again become available (Collagen Matrix Technologies, Boca Raton, FL). As the product is highly biocompatible, it elicits almost no inflammatory response and the effects are mostly dependent on precision injection technique with delivery of product into the mid to superficial dermis. As we have all become more comfortable with the requirement for the use of local anesthetic and regional nerve blocks with our recent wealth of experiences with a host of hyaluronic acid products, its acceptance is now even greater. The advantages over the hyaluronic acid products, as with the other ‘collagens’ is its superiority specific for the treatment of finer and more superficial rhytids. Its advantage over the use of bovine is the lack of need for skin testing and the advantage over CosmoDerm/CosmoPlast also relates to persistence, lack of inflammatory reactions, and cost.
As with most of the injectable agents, preferred injection technique is highly variable and region dependent. Enhanced patient comfort is facilitated by local anesthesia. Once anesthetized a slow and deliberate application whether by serial puncture or threading can deliver excellent results with satisfactory persistence (Fig. 23-11).
Protocols for optimal treatment vary slightly from the Zyderm/CosmoDerm experiences whereby patients are treated initially and a second treatment is administered within 3–6 weeks to a satisfactory visual endpoint. Patients are seen again within the next 3–6 weeks to evaluate and consideration of a third treatment. In either scenario of a third (or even fourth) treatment or not, the experiences with skilled injectors is that the result can be up to 6 months.
More ‘collagens’
Over the past 20 years, a host of other collagen-like products have come and gone. The high level of interest in producing a collagen-based product for distribution has persisted since the introduction of bovine collagen in the early 1980s. Fascian, Cymetra, and a long list of other products have emerged after the introduction of Dermalogen, as a result of the demand for a collagen-based product for soft tissue augmentation that would not require skin testing. The nature of some of these agents however, yield suboptimal persistence, hence their waning popularity. A porcine collagen derivative, Evolence, will be introduced into the US market in the next couple of years.11 The theoretic advantages over the bovine collagens (beyond the growing European resistance to bovine products) relate to their proprietary cross-linking process that is supposed to aid against rapid degradation and resorption. A skin test, however, may also be required for this product.
Autologous fat
The oldest available filler and reportedly first used by Neuber in 1893,12 fat has the advantage of being auto-logous and abundant in the body,13 enabling the correction of contour defects without risk of allergy. The indications are most often for the correction of larger subcutaneous defects such as the nasolabial folds and senescent facial volume loss. However, the success of fat procedures depends on the method of harvesting, the type of fat used, and the injector’s level of experience, and disadvantages include donor site morbidity, calcification of the injected fat, and unpredictable resorption.13 Since the variable longevity of contour correction depends on technique, amount of fat injected, and location, improvements in harvesting, handling, and the injection process may have an impact on positive patient outcomes.14,15
Some believe autologous fat grafting to represent the ideal replacement for soft-tissue atrophy, replacing volume and contours lost in the aging process.14 Injections are delivered through large-bore needles requiring local or even general anesthesia. Techniques, handling, and instrumentation vary significantly and consensus has yet to be arrived upon. In 1997, Coleman promoted LipoStructure® – the placement of small amounts of autologous fat in multiple tunnels – for a safe, long-lasting method of recontouring the face.15 The fat autograft muscle injection (FAMI) technique, developed by Amar, involves the injection of adipose tissue within the muscles of facial expression in intricate layers of autologous fatty tissue with anatomic patented microcanulas and has shown improved long-term, aesthetic results for facial rejuvenation.16,17 In ‘fat rebalancing,’ fat is harvested from the patient, frozen, and transferred in less than 0.1 cc aliquots under low injection pressures, weaving fat in a crosshatched 3D design through the muscle to the subdermis or, when injected periorbitally, placed conservatively deep to the periocular musculature.18a,18b,19
Despite improvements in technique, however, the fact remains that autologous fat grafting demonstrates unpredictable and sometimes temporary results.20,21 Relating to the use of injectable autologous fat for facial rejuvenation, possibly the largest ‘epidemic’ of disappointment by patients regarding their treatment is the indiscriminant use of fat as a tool for improving the volume depletion and hollowness of the lower periorbita (Fig. 23-12). Unfortunately, the attempts of ‘simple’ replacement of volume of the lower eyelid and cheek are met with several obstacles including the irregular fat survival after injection compounded by the atrophy of the lower periorbital structures that reveal the imperfect solution, and is not only distressful for the patient but at times difficult if not impossible to correct. Similar to experiences in the other facial regions, results also have been highly variable and somewhat unpredictable, often with gross visibility of the irregularity of fat survival through the thin peri-orbital skin. Surgical efforts to reverse these iatrogenic problems are difficult at best (Fig. 23-13).
Complications
Harvesting and reinjecting fat are both significant procedures that are associated with downtime and the possibility of serious complications. The main prob-lems associated with autologous fat are its variable resorption rate and unpredictability.13 Although largely technique-dependent, potential complications of autologous fat grafting include prolonged edema, bruising, undercorrection, overcorrection, clumping, irregularities, fat necrosis, migration, and infection, in addition to the other risks associated with surgical procedures.13