Infraorbital Discoloration: Dark Circles—An Anatomic Analysis and Treatment
Cynthia A. Boxrud
Deena A. Sylvester
Infraorbital discoloration is a common complaint among many patients who often describe the problem as dark circles. The discoloration often follows the anatomy of the orbicularis oculi muscle, which surrounds the orbital area. In the literature, most of the papers that address this issue refer to the problem as pigmentary (1,2). Although this may be the case in some patients, it certainly is not the etiology in most patients. The problem tends to be multifactorial in nature (3). A careful assessment, which requires the patient’s history with identification of the interindividual anatomic structural elements, is the key to obtaining an accurate diagnosis. This information can be readily incorporated into appropriate treatment protocols.
The evaluation of dark circles and the available treatment protocols are reviewed in this chapter.
Etiologies
Most sources and papers addressing infraorbital discoloration have focused on hyperpigmentation in the region of the lower eyelid. Although pigment deposition can play a role, more often it is the result of multiple factors, including skin translucency, vascularity, and heredity/ethnicity. The authors have reviewed records of 45 patients who presented with dark circles. An extensive history and physical examination were completed in all patients. Sixty-five percent of patients of all etiologies had a Fitzpatrick classification of III to V, and 35 % were Fitzpatrick classification I to II. Thirty percent were Mediterranean (Italian/Middle Eastern) or Latin in heritage; 35% were Northern or Eastern European; and 15% were black. Thirty-five percent had a strong history of chronic allergy or sinus disease; 2% reported chronic eye rubbing; 54% had a prominent family history of dark circles; 54% were judged to have pigment deposition contributing to the development of the dark circle; and 82% were diagnosed with a predominantly vascular component. These results demonstrate that infraorbital discoloration is truly multifactorial as
evidenced by the presence of “discoloration” in both pigmented and nonpigmented individuals. Additionally, the discoloration in the lower eyelid of more pigmented patients was not synonymous with the presence of excess pigment in the area. Many of the more darkly pigmented patients were judged to have “dark circles” due to a predominantly vascular component. It is our estimation that infraorbital discoloration more often is the result of vascular causes than pigment deposition, but it is clear that more studies evaluating the cause of “dark circles” need to be performed before we can fully understand every aspect this condition.
evidenced by the presence of “discoloration” in both pigmented and nonpigmented individuals. Additionally, the discoloration in the lower eyelid of more pigmented patients was not synonymous with the presence of excess pigment in the area. Many of the more darkly pigmented patients were judged to have “dark circles” due to a predominantly vascular component. It is our estimation that infraorbital discoloration more often is the result of vascular causes than pigment deposition, but it is clear that more studies evaluating the cause of “dark circles” need to be performed before we can fully understand every aspect this condition.
We can generalize that there are four main categories of causes for “dark circles,” which can be present in isolation or in combination: deep vascular congestion/superficial vascularity, hyperpigmentation, skin translucency, and structural shadowing. It is important to differentiate from among these various causes to allow appropriate selection of treatment modalities that will achieve the most successful outcome.
Vascular
The rich vascular network located around the medial canthus and nasal periorbital regions is the cause of the appearance of dark circles seen in children and adults with chronic allergies or sinus disease. Typically referred to as “allergic shiners,” these bluish discolorations in the orbitopalpebral groove are caused by chronic congestion of the nasal and paranasal cavities. Historically, according to Grant (4) and Marks (5,6), “the venous network of the mucous membranes in the paranasal and nasal cavities is drained chiefly by branches of the sphenopalatine veins passing backward to the pterygoid plexus. Prolonged and persistent allergic edema of the mucous membranes of [these cavities] produces pressure effects on the veins, interfering with their normal drainage.” Therefore, with engorgement of the lower venous marginal arcades and palpebral veins (which drain via the angular vein and inferior ophthalmic vein to the same sphenopalatine vein and pterygoid plexus), bluish discoloration develops in the infraorbital area (4, 5, 6, 7, 8 and 9).
A complex superficial vascular network exists within the dermis of the eyelid. When these small subcutaneous vessels become visible, they lend a reddish discoloration to the area (1). Hypothetically, their visibility could be the result of chronic eye rubbing, which creates repeated superficial trauma to the area. Rubbing of the eyes also may lead to deposition of pigment (see section on Hyperpigmentation).
Hyperpigmentation
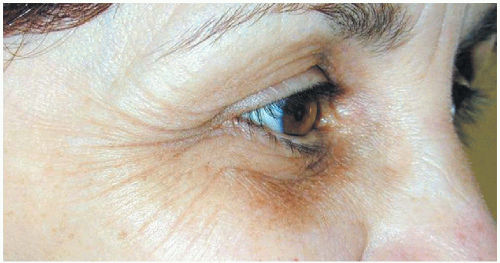
Hyperpigmentation occurs in a semicircular pattern involving the lower eyelid (Fig. 5.2C.1). Hyperpigmentation in this area can result from a multitude of focal or systemic conditions (10).
Postinflammatory hyperpigmentation can cause pigment accumulation in a superficial (more commonly) or deep (severe cases) pattern. Inflammatory conditions (such as systemic and discoid lupus and lichen planus) that disrupt the deep dermal-epidermal junction often heal with melanin deposition in the dermal macrophages, where turnover of melanin is extremely slow. If severe, other types of inflammatory conditions such as allergic dermatitis, trauma, drug eruptions, and photocontact dermatitis can lead to disruption in the dermoepidermal junction. More commonly, however, these conditions resolve with more superficial pigment deposition in the basal layer. This more superficial type of pigment deposition tends to fade over several weeks to months and is more amenable to treatment with topical bleaching creams (10).
Hyperpigmentation can result from noninflammatory lesions of the periorbital area. Examples of these conditions include melasma, ephelides, lentigo simplex, junctional nevi, solar lentigines (“liver spots”), and nevi. Systemic conditions that can lead to pigmentation of the periorbital area include metabolic and endocrine disorders (cirrhosis, Addison disease, hyperthyroidism, hyperpituitarism, Cushing syndrome), hemochromatosis, porphyria cutanea tarda, alkaptonuria, heavy metalrelated conditions (argyria, mercury, chrysiasis), and acanthosis nigricans (10).
Skin Translucency
The skin of the eyelids and periorbital area is markedly thin compared to skin elsewhere on the face. With aging, this skin becomes even thinner, causing it to become more translucent. The vascular network underlying the surface becomes visible and lends a reddish-blue hue to the periorbital area (Fig. 5.2C.2). This is especially true in the area of the infraorbital rim, where the lack of structural fat and muscle found elsewhere on the face places the coloration in relief against the underlying bone (1,10).
Structural Shadowing
Multiple anatomic aspects of the periorbital area can create shadows in the infraorbital area. Classically, deeply set orbits can cause shadowing that results in discoloration




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree